IJCRR - 6(14), July, 2014
Pages: 49-53
Date of Publication: 22-Jul-2014
Print Article
Download XML Download PDF
A RARE CASE OF FIBROUS PSEUDO TUMOR
Author: Sudha V., Ganthimathy Sekhar, Karunakumar, Jayaganesh, Vimal Chander R.
Category: Healthcare
Abstract:Fibrous pseudotumor or periorchitis is a reactive fibromatous proliferation that might involve the coverings of the testis, spermatic cord and epididymis. It is believed to be a reactive, non-neoplastic lesion that may clinically mimic testicular malignancy. Here, we present a case of fibrous pseudo tumor in a 72-year-old male.
Keywords: Periorchitis, pseudotumor
Full Text:
INTRODUCTION
Benign intrascrotal fibrous proliferations (fibrous pseudotumor of scrotal contents) are uncommon with most arising from the paratesticular region. They have been variably designated as chronic proliferative periorchitis, inflammatory pseudotumor, pseudofibromatousperiorchitis or reactive periorchitis.1,2,3 These lesions are usually nodular and involve the testicular tunics. They may also be diffuse and involve the epididymis and spermatic cord. Clinically they mimic malignancy resulting in the treatment by radical orchidectomy.4,5,6
CASE HISTORY
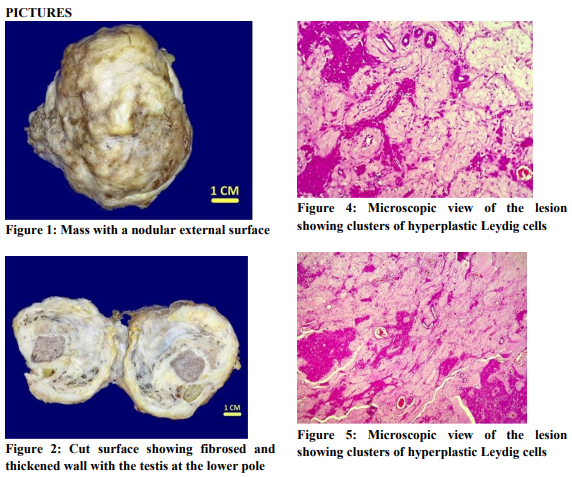
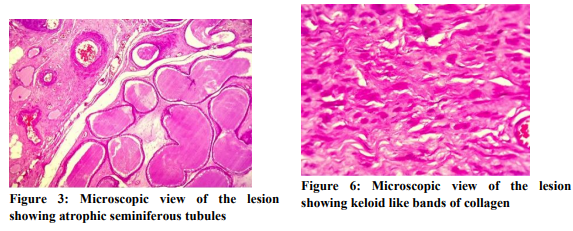
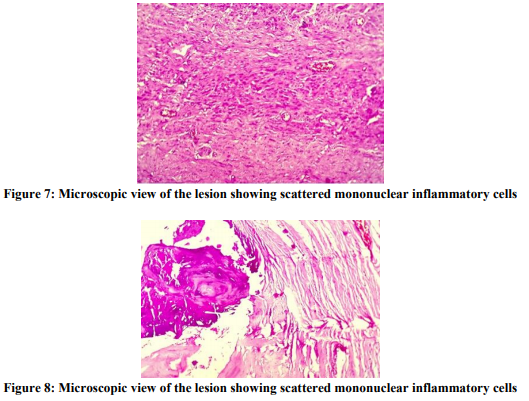
A 72-year-old male came with the complaints of a right-sided inguinal swelling of three years duration. On examination, he was found to have an inguinal hernia with a nodular hard scrotal mass on the same side. There were no other significant physical findings. The scrotum and testis of the other side were normal. Right herniorraphy with high orchidectomy was performed .The orchidectomy specimen was sent for histopathological examination. We received a specimen of right testis with cord structures measuring 7x5x3 cm .The mass was hard in consistency with a nodular external surface. It was gritty and hard to cut. The cut surface revealed fibrosed and thickened wall with chalky white areas measuring about 3 cm in thickness with the testis at the lower pole measuring 2x2 cm .The testis and spermatic cord appeared normal grossly. [Figures 1 and 2] Light microscopic sections studied from the testis showed atrophic seminiferous tubules separated by clusters of hyperplastic Leydig cells. [Figures 3,4 and 5] The wall surrounding the testis showed dense fibrous tissue with keloid like bands of collagen and large areas of calcification. Sparse scattered mononuclear inflammatory cells were present. [Figures 6,7 and 8] DISCUSSION Fibromatous lesions of testicular tunics were recognized by Sir Astley cooper in 1830.4The term Fibrous pseudotumor was introduced by Mostofi and Price.5 It is an uncommon lesion with an incompletely understood etiology. It’s a reactive non neoplastic condition that most often affects patients in their second and third decade of life and is very rare before 18 years.5,7,8,9,10 Only 4 cases have been reported under 18 years.
Benign intrascrotal fibrous proliferations (fibrous pseudotumor of scrotal contents) are uncommon with most arising from the paratesticular region. They have been variably designated as chronic proliferative periorchitis, inflammatory pseudotumor, pseudofibromatousperiorchitis or reactive periorchitis.1,2,3 These lesions are usually nodular and involve the testicular tunics. They may also be diffuse and involve the epididymis and spermatic cord. Clinically they mimic malignancy resulting in the treatment by radical orchidectomy.4,5,6 CASE HISTORY A 72-year-old male came with the complaints of a right-sided inguinal swelling of three years duration. On examination, he was found to have an inguinal hernia with a nodular hard scrotal mass on the same side. There were no other significant physical findings. The scrotum and testis of the other side were normal. Right herniorraphy with high orchidectomy was performed .The orchidectomy specimen was sent for histopathological examination. We received a specimen of right testis with cord structures measuring 7x5x3 cm .The mass was hard in consistency with a nodular external surface. It was gritty and hard to cut. The cut surface revealed fibrosed and thickened wall with chalky white areas measuring about 3 cm in thickness with the testis at the lower pole measuring 2x2 cm .The testis and spermatic cord appeared normal grossly. [Figures 1 and 2] Light microscopic sections studied from the testis showed atrophic seminiferous tubules separated by clusters of hyperplastic Leydig cells. [Figures 3,4 and 5] The wall surrounding the testis showed dense fibrous tissue with keloid like bands of collagen and large areas of calcification. Sparse scattered mononuclear inflammatory cells were present. [Figures 6,7 and 8]
DISCUSSION
Fibromatous lesions of testicular tunics were recognized by Sir Astley cooper in 1830.4The term Fibrous pseudotumor was introduced by Mostofi and Price.5 It is an uncommon lesion with an incompletely understood etiology. It’s a reactive non neoplastic condition that most often affects patients in their second and third decade of life and is very rare before 18 years.5,7,8,9,10 Only 4 cases have been reported under 18 years.
Most patients present with a slowly growing mass in the subcutaneous or deep soft tissues and may be associated with systemic symptoms. Although uncommon, reactive fibrous proliferative lesions apparently represent the third most common benign tumor forming paratesticular condition after spermatic cord lipoma and epididymaladenomatoid tumor.4,11 Jones et al proposed a classification for benign fibrous proliferations of the testis and paratesticular region based on the neoplastic or non-neoplastic nature of the lesion and separated the lesions / tumors into various categories based on clinical and pathologic features, location, and immunohistochemical studies.1 They and others believe that certain intrascrotal fibrous proliferations are truly neoplastic;4, 12 however, it is generally agreed that fibrous pseudotumors, nodular and diffuse, are reactive, non neoplastic lesions.4,13 Although fibrous pseudotumors of the testicular tunics are accepted as reactive lesions, their pathogenesis is not well understood. They are often associated with hydrocele in 50 %, trauma, infection or inflammatory process in 30 %.5,14 Some suggest lymphatic obstruction have a role in the development of these lesions.5The cell of origin for fibrous pseudotumor appears to be the fibroblast or myofibroblast as suggested by Immunohistochemistry.9 The terms fibroma, non specificperitesticular fibrosis, nodular fibrous periorchitis, chronic proliferative periorchitis, proliferative funiculitis, nodular fibropseudotumour, inflammatory pseudotumor, reactive periorchitis, pseudofibrousperiorchitis, peritesticularfibromatosis, and fibrous mesothelioma have been used for this lesion partly reflecting the variable and overlapping spectrum of pathological findings and various etiological theories.1,2,3 Some have restricted the use of “Pseudotumor” to mass forming lesions and have used “Fibrous periorchitis” for more diffuse lesions. The morphology of the non-neoplastic lesions shows variable histology; some contain spindle cells with a whorled appearance and hyalinized collagen. The burnt out lesions are represented by focal (dystrophic) calcification and ossification. Histology may show cellular, granulation tissue type fibrous proliferation and markedly reactive stromal cells.15 There may be an inflammatory component including plasma cells, histiocytes, eosinophils and lymphocytes.
CONCLUSION
Fibrous periorchitis is distinctly uncommon reactive or non-neoplastic lesion, which should be considered in the differential diagnosis when one encounters a lesion with predominantly fibro collagenous stroma.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Jones MA, Young RH, Scully RE. Benign fibromatoustumours of the testis and the para testicular region: A report of 9 cases with proposed classification of fibromatoustumours and tumour like lesions. Am J Surgpathol 1997;21:296-305.
2. Benisch B, Peison B, Sobel HJ. Fibrous mesotheliomas (Pseudofibroma) of the scrotal sac: A light and ultra structural study. Cancer 1981;47:731-5.
3. Srigli JR, Hartwick RW. Tumors and cysts of paratesticular region.PatholAnnu1990;25:51- 108
4. Ulbright TM, Amin MB, Young RH. Tumors of the Testis, Adnexa, Spermatic Cord, and Scrotum.Atlas of Tumor Pathology.3rd series.Fascicle 25. Edited by Juan Rosai: Washington, DC: Armed Forces Institute of Pathology; 1999: 317-9.
5. Mostofi FK, Price EB. Tumors of the Male Genital System.In Atlas of Tumor Pathology.2nd series.Fascicle 8. Edited by Harlan I.Firminger: Washington, DC: Armed Forces Institute of Pathology, 1973:151-4
6. Parveen T, Fleischmann J, Petrelli M. Benign fibrous tumor of the tunica vaginalis testis. Report of a case with light, electron microscopic, and immunocytochemical study, and review of the literature. Arch Pathol Lab Med. 1992;116:277-80.
7. FetschJF,Montgomery EA, Meis JM. Calcifying fibrous pseudotumor. Am J SurgPathol1993;17:502
8. Jimenez-Heffernan JA,Urbano J, Tobio R, et al.Calcifying fibrous pseudotumor: a rare entity related to inflammatory pseudotumor.Actacytol 2000;44;932
9. Seethala RR, Tirkes AT, Weinstein S, Tomaszewski JE, Malkowicz SB, Genega EM. Diffuse fibrous pseudotumor of the testicular tunics associated with an inflamed hydrocele. Arch Pathol Lab Med 2003, 127:742-4
10. Bostwick DG. Spermatic cord and testicular adnexa. In: Bostwick DG, Eble JN (eds). Urologic Surgical Pathology. St Louis, MO: CV Mosby Co; 1997:647–674.
11. Tobias-Machado M, Correa Lopes Neto A, HeloisaSimardi L, Borrelli M, Wroclawski ER. Fibrous pseudotumor of tunica vaginalis and epididymis. Urology 2000; 56:670xx– 670xxii.
12. Parveen T, Fleischmann J, Petrelli M. Benign fibrous tumor of the tunica vaginalis testis. Arch Pathol Lab Med. 1992;116:277–280.
13. Oliva E, Young RH. Paratesticular tumor-like lesions.SeminDiagPathol. 2000;17:358.
14. Akbar SA, Sayyed TA, HasanJafri SZ, Hasteh F, Neill JSA. Multimodality imaging of paratesticular neoplasms and their rare mimics.Radiographics 2003; 23:1461–1476.
15. HollywoodK, Fletcher CDM. Pseudosarcomatousmyofibroblastic proliferations of the spermatic cord (“Proliferative funiculitis”)Histologic and immunohistochemical analysis of a distinctive entity. Am J surgpathol 1992;16:448-454
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License