IJCRR - 13(22), November, 2021
Pages: 86-93
Date of Publication: 20-Nov-2021
Print Article
Download XML Download PDF
Bisap Score and Ranson's Score in Predicting Severity of Acute Pancreatitis: A Comparative Study
Author: Kommi Swetha, Chakravarthy D J K, Eli Lakshmi Aditya, C Radhamani, Vallepalli Ramakrishna
Category: Healthcare
Abstract:Introduction: Acute pancreatitis is an inflammation of the pancreas, due to alcohol or gallstones. Severe pancreatitis may lead to higher morbidity and mortality. Early, an efficient and structured scoring system is required to know the potential outcome of the patient. Aims: The study aims to assess the accuracy of the bedside index for severity in acute pancreatitis (BISAP) and Ranson's scoring system and to compare both in predicting the severity of acute pancreatitis. Methodology: This is a cross-sectional observational study of 90 patients with acute pancreatitis admitted to GSL medical college and general hospital, Rajahmundry. Results: The mean age of the study group was 38.34 \? 10.41 years. Of the total 90 patients, 47 patients had mild disease, 27 patients had moderately severe courses, and 16 patients had severe courses. Renal failure was the most common organ dysfunction in severe acute pancreatitis and the Mortality rate in this study was 1.1%. Ranson's score had a sensitivity of 93.75% (95% CI 69.77%--99.84%), specificity of 94.59% (95% CI 86.73%--98.5%). BISAP score had a sensitivity of 87.5% (95% CI 61.65% -- 98.45%), specificity of 98.6% (95% CI 92.7% -99.97%). Conclusion: Ranson's score had a higher sensitivity and BISAP had higher specificity in the prediction of severe pancreatitis. Components of the BISAP scoring system are easily available when compared to Ranson's scoring system as the latter may require 48 hours for completion of the assessment.
Keywords: Acute pancreatitis, BISAP score, Ranson’s score, Abdominal pain, Renal failure, Pleural Effusion
Full Text:
INTRODUCTION
Acute pancreatitis is a sudden inflammation of the pancreas, involving peripancreatic tissue and multiple organs. It results from a complex process with a variable aetiology and natural histories, and early identification of patients at high risk can be difficult.
Most episodes of acute pancreatitis (80%) are mild and self-limiting without sequelae. In 10-20% of cases of acute pancreatitis, necrosis will develop in various parts of the pancreas and the surrounding tissue. In such cases systemic inflammatory response syndrome and/or multiorgan failure is seen, may result in death.1,2 Unpredictable and variable individual responses are seen in pancreatic injury.
Pancreas has both exocrine and endocrine functions. Alcohol intake and biliary tract diseases account for the majority of cases (90%) of acute pancreatitis. In Europe and Asia, gallstone-associated pancreatitis predominates. Gallstones are responsible for 50 – 60 % and alcohol for 8 – 32 % of attacks of acute pancreatitis in the U.K.3 Moreover, females are more prone to gallstone pancreatitis, and males for alcohol-induced pancreatitis.
In more than 90% of patients, the predominant feature of acute pancreatitis is a pain in the abdomen. Pain is mostly in the epigastrium, constant, boring, or penetrating, and may radiate to the back. Pain starts 12-48 hours after a bout of alcohol or after a large meal in case of gallstone pancreatitis. Fever, vomiting, tachycardia, epigastric tenderness, hypoactive or absent bowel sounds, and abdominal distension are the other features. Other manifestations include pleural effusion (mostly left side), ascites, and elevation of left hemidiaphragm with tachypnoea, dyspnoea, and cyanosis. Painless pancreatitis, although uncommon, is a definite and well-recognized entity. The evaluation of pancreatic enzymes (Lipase and Amylase) released from the inflamed tissue is the cornerstone of a biochemical diagnosis of acute pancreatitis.4
The simultaneous determination of amylase and lipase offers sensitivity and specificity of 90 to 95 % for detecting acute pancreatitis in patients presenting with acute abdominal pain.5 Contrast-Enhanced Computed Tomography (CECT) is the imaging modality of choice.
Many multifactor scoring systems such as Ranson’s criteria, BISAP, APACHE-II (Acute Physiology and Chronic Health Enquiry) have been described in an attempt to accurately predict the outcome of the disease.
BISAP SCORING SYSTEM
In 2008, Wu et al.6 retrospectively developed a new scoring system, the bedside index for severity in acute pancreatitis (BISAP), to estimate the risk of in-hospital mortality in patients with acute pancreatitis.
Components of the BISAP score include
1. Age > 60 years
2. Bun > 25 mg/dl
3. Impaired mental status (Glasgow coma scale score < 15)
4. SIRS- is defined as two or more of the following:
Temperature of < 36 or > 38 ° c
Respiratory rate > 20 breaths/min or paco2 < 32 mm hg
Pulse > 90 beats/min
WBC < 4,000 or >12,000 cells/mm3 or >10% immature bands
5. Pleural effusion detected on imaging.
One point is assigned for each variable within 24 hrs of presentation. Score ≥3 is read as severe acute pancreatitis (SAP).
The severe disease should be predicted by careful clinical assessment, together with a multiple-factor scoring system and imaging studies.1 Several scoring systems can predict severe complications, but current methods of risk stratification of acute pancreatitis are complex as the data required is not collected at an early stage.17
The bedside index for severity in acute pancreatitis (BISAP) is a pretty simple and precise method for identifying the risk of in-hospital death.1 this study aimed to evaluate the usefulness of the BISAP scoring system as an early severity scoring system, to evaluate Ranson’s scoring system and to compare BISAP with Ranson’s scoring system.
MATERIALS AND METHODS
The present study was carried out in the department of General medicine, GSL Medical College and General Hospital, Rajahmundry from 1st October 2018 TO 30th June 2020 with the approval of the Institutional Ethics committee (485-EC/485-09/18). It is a cross-sectional observational study. A total of 90 cases were studied.
All patients aged more than 20 years with history and clinical findings suggestive of acute pancreatitis with evidence of elevated pancreatic enzymes serum amylase, lipase and bulky oedematous pancreas on USG abdomen were included in the study. Patients having structural abnormalities of the pancreas, chronic pancreatitis, recurrent acute pancreatitis and carcinoma of the head of the pancreas were excluded.
All the selected patients were subjected to detailed clinical examination, laboratory investigations and radiological imaging. The BISAP score was calculated using data of the first 24-hours from admission and the Ranson's score using data from the first 48 hours of hospitalization. Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) or Ultrasound imaging of the abdomen was obtained at any time in the first seven days of hospitalization was used to differentiate necrotizing from interstitial pancreatitis. The scores were compared with the clinical severity, which was graded according to the revised Atlanta classification. Persistent organ failure was graded by the Modified Marshall scoring system.
All the patients were graded as having mild, moderately severe, and severe acute pancreatitis based on the revised Atlanta classification. Patients with mild acute pancreatitis had no local complications or organ failure. Patients with moderately severe acute pancreatitis had transient organ failure or local or systemic complications or both, whereas patients with severe acute pancreatitis had persistent organ failure.
According to Marshall score, Organ failure is defined as the involvement of ≥ 2 organ systems in one or more of the three (respiratory, renal, and cardiovascular) out of the five. For all patient’s organ failure scores were calculated every 24 hours.
Patients with acute oedematous pancreatitis were managed in the general ward while those with severe disease (Ranson’s and BISAP score > or =3) were admitted to an intensive care unit. Standard management protocols were followed for treating all patients till discharge.
Data were analysed using SPSS software version 17. Different scores on Ranson’s and BISAP were compared to vital signs, haematological parameters, and biochemical parameters that denote organ failure using one-way ANOVA. Ranson’s and BISAP scores were compared in assessing organ failure, pleural effusion using Pearson’s chi-square test for proportions. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were calculated for both BISAP and Ranson’s scores. Receiver operator curves (ROC) for SAP and pancreatic necrosis were plotted for Ranson’s score and BISAP score. Ranson’s score and BISAP score was compared along with organ failure using Kendall’s coefficient of concordance. Linear regression for organ failure as an outcome variable was carried out using biochemical parameters, Ranson’s, and BISAP score, pleural effusion as predictor variables.
RESULTS
A total of 90 persons with features of acute pancreatitis, 81(90%) males and 9(10%) females who fulfilled the inclusion criteria were enrolled in this study after obtaining informed consent. The mean age of the study group was 38.34 ± 10.41 years. The cause of acute pancreatitis was gallstones in 15 patients (16.7%), alcohol in 57 patients (63.3%), hypertriglyceridemia in one patient (1.1%) and idiopathic in 17 patients (18.9%). Abdominal pain was present in 78 (86.7%) patients and vomiting in 25 (27.8%) patients (Table-1). There was a significant difference in the means of various Ranson’s scores with Respiratory rate (RR) (p=0.001), mean Glasgow coma scale (GCS) (p=0.00), mean systolic blood pressure (p= 0.005), mean Total leucocyte count (TLC) (p<0.001) (Table-2).
There was a significant difference between various Ranson’s scores with mean BUN (blood urea nitrogen) (p<0.001), mean BUN increase (p<0.001), mean serum creatinine (p<0.001), mean blood sugar(p=0.003), mean serum AST(p=0017), mean serum LDH (p<0.001), mean paO2(p<0.001), mean paCO2(0.001), mean paO2/Fio2(p<0.001), mean base excess(p<0.001), mean fluid deficit (p<0.001) (Table-3).
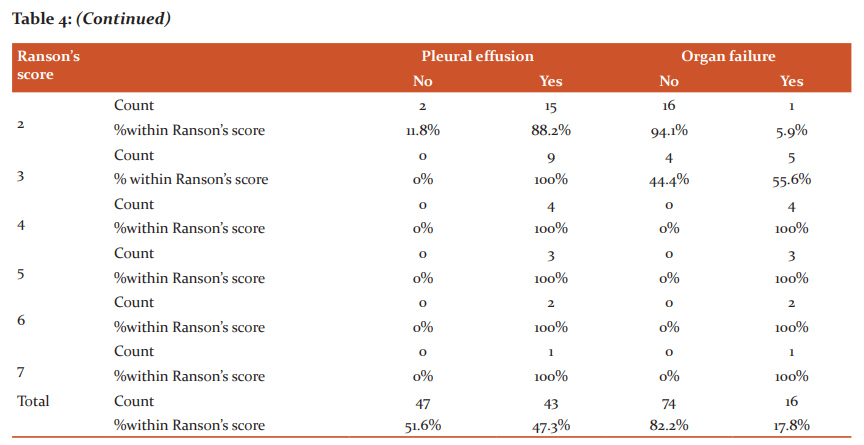
The incidence of pleural effusion increased with an increase in Ranson’s score. Increasing scores on Ranson’s score was related to increasing rates of organ failure. The incidence of pleural effusion and organ failure stratified by Ranson’s score has p<0.001, which is statistically significant (Table-4).
The analysis for prediction of pancreatic necrosis showed Ranson’s score had a sensitivity, specificity, positive predictive value, negative predictive value and accuracy of 84.21% (95% CI 60.42%-96.62%), 95.77% (95% CI 88.14%-99.12 %), 84.21% (95% CI 63.40%--94.26%), 95.77% (95%CI 88.91%---98.46%), 93.33% (95% CI 86.05%--97.51%) respectively.
The statistical analysis for prediction of Severe acute pancreatitis (SAP) showed Ranson’s score had a sensitivity of 93.75% (95%CI 69.77%--99.84%), a specificity of 94.59% (95% CI 86.73%--98.5%), the positive predictive value of 78.95% (95% CI 58.91--98.75%), the negative predictive value of 98.59% (95% CI 91.29%--98.17%) and accuracy of 94.44% (95% CI 87.51--98.17%). Ranson’s score was very sensitive for the prediction of SAP but less sensitive for the prediction of pancreatic necrosis.
According to Ranson’s score, for predicting pancreatic necrosis Area under the curve (AUC) was calculated to be 0.954 with 95% CI 0.900---1.000, p<0.001, and yoden index 0.8. The area under receiver–operator curve for Ranson’s score in predicting SAP was 0.981 with a 95% confidence interval 0.956 to 1.000, Yoden index 0.88, and p<0.001.
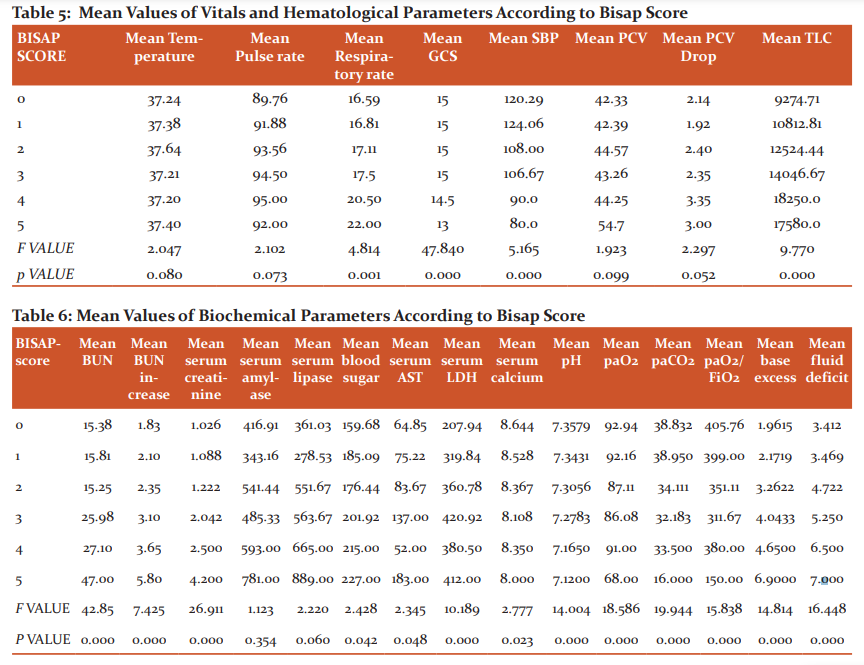
There was a significant difference between various BISAP scores with mean RR (p=0.0061), mean GCS (p=0.03), mean SBP (p<0.001), mean TLC (p<0.001) (Table 5).
There was a significant difference between various BISAP scores with mean BUN (p<0.001), mean BUN increase(p<0.01), mean serum creatinine (p<0.001), mean blood sugar (p=0.042), mean serum AST(p=0.048), mean serum LDH (p<0.001), mean serum calcium (p=0.023), mean pH (p<0.001), mean paO2 (p<0.001), mean paCO2 (p<0.001), mean paO2/FiO2 (p<0.001), mean base excess (p<0.001), mean fluid deficit (p<0.001) (Table 6).
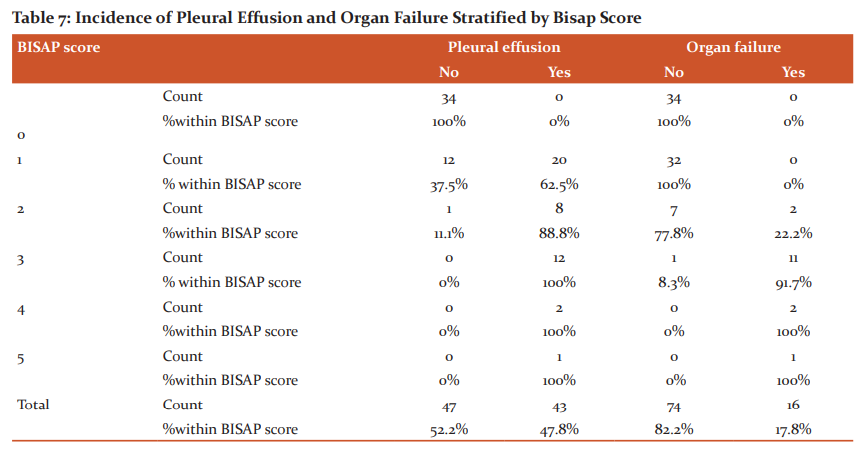
The incidence of pleural effusion increased with an increase in the BISAP score. Increasing scores on the BISAP score was related to increasing rates of organ failure. The incidence of pleural effusion and organ failure stratified by the BISAP score has P<0.001, which is statistically significant (Table 7).
The analysis for prediction of pancreatic necrosis showed BISAP score had a sensitivity, a specificity, positive predictive value, negative predictive value and accuracy of 73.68% (95% CI 48.80% -- 90.85%), 98.59% (95% CI 92.40%---99.96%), 93.33% (95% CI 66.25% -- 96.75%), 93.33% (95% CI 86.83% --96.75%), 93.33% (95% CI 86.05% -- 97.51%) respectively.
The statistical analysis for prediction of SAP showed BISAP score had a sensitivity of 87.5% (95% CI 61.65% -- 98.45%), specificity of 98.6% (95% CI 92.7% --99.97%), positive predictive value of 93.33% (95% CI 66.45% -- 99.0%), negative predictive value of 97.33% (95% CI 90.89% -- 99.26%) and accuracy of 96.67% (95% CI 90.57% -- 99.31%). BISAP score was very sensitive for prediction of SAP, but less sensitive for prediction of pancreatic necrosis.
For predicting pancreatic necrosis, according to the BISAP score, the area under the curve was 0.970 with a 95% confidence interval of 0.931to1.000, p<0.001, and yoden index 0.86. The area under the receive-operator curve for BISAP score in predicting SAP was 0.988 with a 95% confidence interval 0.970 to 1.000, yoden index 0.86, and p<0.001.
There was a significant concordance between Ranson’s score with BISAP score with Kendall’s coefficient of concordance being 80% with p<0.001.
Linear regression was conducted to determine predictors for organ failure. PR, RR, SBP, GCS, temperature, TLC, PCV, PCV drop, serum lipase, serum amylase, BUN, BUN increase, serum creatinine, blood sugar, serum AST, serum LDH, serum calcium, pH, paO2, paCO2, base excess, paO2/FiO2, fluid deficit, Ranson’s score, BISAP score, pleural effusion was entered as predictors for organ failure. These predictors contributed 92.3% variance in the model with ANOVA f (27,61) =13.029, p<0.001. BUN emerged as a significant predictor for organ failure compared to all other predictors with beta=0.313, p=0.18.
DISCUSSION
This study evaluated the usefulness of BISAP and Ranson’s scores as early markers of the severity of acute pancreatitis and compared the accuracy of predicting organ failure. The ability to stratify patients early in the course of disease into mild and severe forms is a major step in improving management strategies in acute pancreatitis.
The age of the study subjects in the present study varied from 20 to76 years with a mean age of 38.34±10.41years. The majority of the study population was in the age group of 30 to 40 years. In an Indian based study conducted in Srinagar, Jammu, by Banday et al.7 mean age of the study population was 42.32yearrs. The mean age of the study Population in another study done in Varanasi Uttar Pradesh by Khanna et al.8 was 40.5 years.
There is a distinct male preponderance in the present study concerning gender, and the majority were males 90%, and females were10%. This result didn’t match with other studies conducted elsewhere. This could be due to the difference in the aetiology of acute pancreatitis, alcohol being the most common etiological factor in this study and alcohol consumption in females being very rare in this region.
In the present study, the etiological agent for acute pancreatitis was alcohol in 63.3% and gallstones in16.7% of the study population. In Harshit Kumar et al.9 study, the most common aetiology of acute pancreatitis was gallstones (74%), followed by alcohol (18%). In the present study, Ranson’s score of <3 was noted in 78.8% and ≥3 in 21.2% of the study population. In Shandana Tarique et al.'s 10 studies, Ranson’s score of< 3 was observed in 50% and ≥3 in 50% of the study population. In a Pakistan based study done by Anum Arif et al., 11 64.1% of the population had Ranson’s score <3 and 35.9% of the population had Ranson’s score≥3.
In the present study BISAP score of <3 was noted in 82.5% and ≥3 in16.5% of the study population. In Yadav et al.12 study BISAP score of < 3 was observed in 61.3% and ≥3 in 38.6% of the study population. In a study done by Papachrisotu et al., 1 85.9% of the study population had a BISAP score of<3 and 14.1% of the study population had a BISAP score of ≥3.
In the present study, pancreatic necrosis developed in 4.2% of patients with Ranson’s score<3, in 84.2% of patients with Ranson’s score ≥3, 6.6 % of patients with BISAP score≤2 and in 93.3% of patients with BISAP score≥3. In Lalith Kumar et al.13 study, 2 out of 80 patients (2.5%) with Ranson’s score<3 and 7 out of 20 patients (35%) with Ranson’s score≥3 had pancreatic necrosis. In Sanjit Karki et al.14 study incidence of pancreatic necrosis was observed in 7.2% of cases with BISAP score≤2 and in 69.2% of pts with BISAP score≥3.
Pancreatic necrosis was associated with increased severity and mortality. In the present study incidence of pancreatic necrosis was observed more in patients with a BISAP score of ≥3. In the present study, SAP developed in 1.4% of patients with Ranson’s score<3, 78.9% of patients with Ranson’s score≥3, 2.66% of patients with BISAP score≤2 and in 93.3% of patients with BISAP score≥3. In Korean based study done by Cho JH et al.15 incidence of SAP was seen in 4.6% of patients with Ranson’s score<3 and 18.8% of patients with Ranson’s score≥3. In Yadav et al.12 study, the incidence of SAP was observed in 2.7% of cases with BISAP score≤2 and in 86.9% of cases with BISAP score≥3. More recently, organ failure is a much stronger predictor of mortality than local complications such as peripancreatic fluid collections and necrosis. In addition, organ failure is a major determinant of the duration of hospitalization for patients with acute pancreatitis.16
In a Chennai based study by Lalith Kumar et al.13 Ranson’s score had a sensitivity of 90.91%, a specificity of 77.53%, a positive predictive value of 43.56%, a negative predictive value of 98.57%, and an accuracy of 91% for predicting pancreatic necrosis and BISAP score had a sensitivity and specificity of 81.82%,94.38% with positive predictive value 64.29%, negative predictive value 97.67%, and accuracy of 93%. A Portugal based study done by Simoes et al.17 found that Ranson’s score had a sensitivity of 91.2%, a specificity of 74.4%, a positive predictive value of 57.4%, and a negative predictive value of 95.7% for predicting SAP. In Rudrarpan Chatterge et al.18 study sensitivity, specificity, positive predictive value, and negative predictive value of BISAP score in predicting SAP were 80%,68.66%,43.24%,92% respectively.
In the present study, receiver-operating characteristic curves yielded an AUC of 0.970 (95% CI 0.931—1.000) for BISAP score and 0.954 (95% CI 0.900—1.000) for Ranson’s score in predicting pancreatic necrosis. In Zhang J et al.19 study the AUC for BISAP score in predicting the development of Pancreatic necrosis was 0.834 (95% Cl 0.739–0.929), and that of Ranson’s score was 0.840 (95% CI 0.741–0.939).
In the present study for predicting the development of SAP AUC of BISAP score was 0.988 (95% CI 0.970---1.000, p-value <0.001) and that of Ranson’s score was 0.981(95% CI 0.956---1.000, p-value <0.001). In a Papachristou et al.1 study an AUC of 0.81(CI 0.74 – 0.87) for BISAP Score and 0.94 (95% CI 0.89—0.97) for Ranson’s score in predicting the development of SAP. In Korean based study done by Kim BG et al.20 AUC of BISAP and Ranson’s scores in predicting SAP were 0.873(95% CI 0.770—0.976) and 0.947(0.001—1.000) respectively.
CONCLUSION
BISAP scoring system accurately predicted the outcome in patients with acute pancreatitis in the present study. Moreover, the BISAP score is easy to perform and can be done at the bedside of patients with acute pancreatitis in every setup. BISAP score is simple, more convenient and has proved to be a powerful tool in predicting the severity of acute pancreatitis at par with Ranson’s score.
ACKNOWLEDGEMENT: We acknowledge our sincere thanks to all technical staff, statisticians, and clerical staff for their extended support throughout the study period. Our sincere thanks to the editor and the journal staff for publishing the article.
CONFLICT OF INTEREST: Nil
SOURCE OF FUNDING: Nil


References:
-
Papachristou GI, Muddana V, Yadav D, O'Connell M, Sanders MK, Slivka A et al. Comparison of BISAP, Ranson's, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis. Am J Gastroenterol. 2010 Feb;105(2):435-41
-
Pezzilli R, Zerbi A, Di Carlo V, Bassi C, Delle Fave GF; Working Group of the Italian Association for the Study of the Pancreas on Acute Pancreatitis. Practical guidelines for acute pancreatitis. Pancreatology. 2010;10(5):523-35.
-
Poston GJ, Williamson RC. Surgical management of acute pancreatitis. Br J Surg . 1990 Jan;77(1):5-12.
-
Tenner S, Baillie J, DeWitt J, Vege SS; American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013 Sep;108(9):1400-15; 1416.
-
Klaus M, John B.Acute Pancreatitis. BMJ 1998; 316: 44-8.
-
Wu BU, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008 Dec;57(12):1698-703.
-
Banday IA, Tattoo I, Khan AM, Javeed J, Gupta G, Latief M. Modified Computed Tomography Severity Index for Evaluation of Acute Pancreatitis and its Correlation with Clinical Outcome: A Tertiary Care Hospital Based Observational Study. J Clin Diagn Res. 2015 Aug;9(8): TC01-5.
-
Khanna AK, Meher S, Prakash S, Tiwary SK, Singh U, Srivastava A et al. Comparison of Ranson, Glasgow, MOSS, SIRS, BISAP, APACHE-II, CTSI Scores, IL-6, CRP, and Procalcitonin in Predicting Severity, Organ Failure, Pancreatic Necrosis, and Mortality in Acute Pancreatitis. HPB Surgery: 2013 ;2013:367581.
-
Harshit Kumar A, Singh Griwan M. A comparison of APACHE II, BISAP, Ranson's score and modified CTSI in predicting the severity of acute pancreatitis based on the 2012 revised Atlanta Classification. Gastroenterology Report. 2018 May;6(2):127-131.
-
Tarique S, Sarwar S, Iqbal F. Validity of Ranson's Score for Predicting Mortality and Morbidity in Acute Pancreatitis. Proceedings S.Z.P.G.M.I. 2003;17(2):67-70.
-
Arif A, Jaleel F, Rashid K. Accuracy of BISAP score in prediction of severe acute pancreatitis. Pak J Med Sci. 2019 Jul-Aug;35(4):1008-1012.
-
Yadav J, Yadav SK, Kumar S, Baxla RG, Sinha DK, Bodra P et al. Predicting morbidity and mortality in acute pancreatitis in an Indian population: a comparative study of the BISAP score, Ranson’s score and CT severity index, Gastroenterology Report, 2016 Aug;4(2):216-220.
-
Lalithkumar J, Chitra T, Kodieswaran N. Comparative study between BISAP and Ranson’s score in predicting the severity of acute pancreatitis. IAIM, 2016; 3(9): 23-33.
-
Karki S, Karki B, Thapa S, Shrestha R, Poudel BN, Shrestha R. Accuracy of bedside index for severity in acute pancreatitis ‘BISAP’ score in predicting the outcome of acute pancreatitis. JPAHS 2020Aug;7(2):70-76.
-
Cho JH, Kim TN, Chung HH, Kim KH. Comparison of scoring systems in predicting the severity of acute pancreatitis. World J Gastroenterol. 2015 Feb 28;21(8):2387-94.
-
Garg PK, Madan K, Pande GK, Khanna S, Sathyanarayan G, Bohidar NP et al. Association of extent and infection of pancreatic necrosis with organ failure and death in acute necrotizing pancreatitis. Clin Gastroenterol Hepatol. 2005 Feb;3(2):159-66.
-
Simoes M, Alves P, Esperto H, Canha C, Meira E, Ferreira E et al. Predicting Acute Pancreatitis Severity: Comparison of Prognostic Scores. Gastroenterology Res. 2011 Oct;4(5):216-222.
-
Chatterjee R, Parab N, Sajjan B, Nagar VS. Comparison of Acute Physiology and Chronic Health Evaluation II, Modified Computed Tomography Severity Index, and Bedside Index for Severity in Acute Pancreatitis Score in Predicting the Severity of Acute Pancreatitis. Indian J Crit Care Med. 2020 Feb;24(2):99-103.
-
Zhang J, Shahbaz M, Fang R, Liang B, Gao C, Gao H et al. Comparison of the BISAP scores for predicting the severity of acute pancreatitis in Chinese patients according to the latest Atlanta classification. J Hepatobiliary Pancreat Sci. 2014 Sep;21(9):689-94.
-
Kim BG, Noh MH, Ryu CH, Nam HS, Woo SM, Ryu SH et al. A comparison of the BISAP score and serum procalcitonin for predicting the severity of acute pancreatitis. Korean J Intern Med. 2013 May;28(3):322-9.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License