IJCRR - 13(19), October, 2021
Pages: 70-75
Date of Publication: 11-Oct-2021
Print Article
Download XML Download PDF
Study of Ocular Manifestations in Systemic Malignancies
Author: Khochikar Nilima M., Karambelkar VH
Category: Healthcare
Abstract:Introduction: Primary ophthalmic tumours are well known, but the eye is a rare site for disseminated malignancy. The eye and orbit can get affected by cancer due to the direct effect of metastatic neoplastic infiltration or compression or by circulating anti-bodies involving paraneoplastic retinal degeneration. Aim: The present study aims to objectify the ocular manifestations in systemic malignancies. Methodology: This cross-sectional study was conducted on patients presenting with systemic malignancies to the out-patient department of Krishna Hospital Karad, Maharashtra, from December 2018 to May 2020. Result: Ophthalmic manifestations were seen in 21.77% of patients with systemic malignancies. Conclusion: All patients with systemic malignancies (primary and metastatic) should undergo a thorough ophthalmic examination regularly to prevent visual loss.
Keywords: Ocular manifestations, Systemic malignancies, Metastatic, Visual loss, Ophthalmic, Antibodies
Full Text:
INTRODUCTION:
Primary ophthalmic tumours are well known, but the eye is a rare site for disseminated malignancy. The eye and orbit can get affected by cancer due to the direct effect of metastatic neoplastic infiltration or compression or by circulating antibodies involving paraneoplastic retinal degeneration. Hematogenous and direct spread also do account for the ocular manifestations of systemic malignancies.1
Metastatic tumour to the uvea is the most common form of presentation. The choroid is the most common site for uveal metastasis. Iris and ciliary body metastases are present in 10% of cases. Retina, optic disc, vitreous, and conjunctiva are affected when there is already uveal tract involvement. Choroidal metastases are associated with an unusually large amount of subretinal ?uid presenting as complete retinal detachment and or a mass on ocular ultrasound.1 In cases of space-occupying lesions, papilledema, abducent nerve palsy, nystagmus and optic atrophy are the most common presenting signs.2
Breast and lung carcinomas for women and lung and gastrointestinal (GI) carcinomas for men most commonly metastasize to the eye and orbit. The incidence of metastasis to the eye from breast cancer is around 47%, from lung cancer is around 21%, and that from the GI tract is around 4%. Melanoma, urological malignancies also manifest with ocular metastasis. Most patients presenting with ocular metastases already have a history of treated primary cancer. However, approximately 1/3rd of patients has no history of primary cancer viz. primary adenocarcinoma of the lung, which can present for the ?rst time with ocular metastases in up to 50% of cases.1,3,4 Metastasis to the eye and orbit and paraneoplastic disorders represent a very bad prognostic sign. The average survival following a diagnosis of uveal metastases is 7 months.3
As the incidence of malignancy is on the rise in India, it is important to study the ocular manifestation of these non-ocular malignancies especially when there is sparse literature on this. The majority of the studies conducted in the past were autopsy studies. Early and prompt diagnosis with appropriate investigations and apt treatment can restore the vision and improve the quality of life in these unfortunate patients. Therefore, this research was conducted to study the occurrence and clinical features of ocular manifestations in systemic malignancies.
METHODOLOGY:
This cross-sectional study was conducted on patients presenting with systemic malignancies to the out-patient department of Krishna Hospital Karad, Maharashtra, from December 2018 to May 2020. According to a study “ocular-metastases”,5 the proportion of ocular manifestations in systemic malignancies is 10%. Therefore, by using formula – N=4PQ/L,2 where P=10%, Q= 100-P (90%), L=4%, at 95% confidence interval, the sample size comes up to 225. Patients with primary ophthalmic tumours and malignancies arising from radiation were excluded. Data entry was done in Microsoft excel 2019 and imported to SPSS version 21.0 for data analysis. The p-values were considered statistically significant if and when p > 0.05. The ethical clearance has been given and by protocol number 0236/2018-2019).
RESULTS:
This cross-sectional study including 225 participants with systemic malignancies yielded the following results.
Baseline characteristics: The mean age of patients in the study population was 52.32 ± 20.26 years. The majority of 113 (50.2%) patients were in the age group of 51-75 years. Ophthalmic manifestations were seen in 49 patients (21.77%) of which, 31(63%) were males and 18(37%) were females.
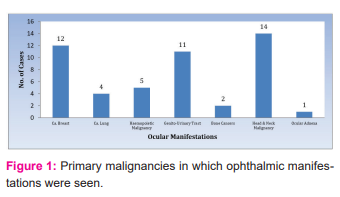
The primary malignancies in which ophthalmic manifestations were seen are depicted in Figure 1. The most common primary malignancy was Head and Neck malignancy (28.57%), followed by breast (24.48%), genitourinary tract (20.40%), hematopoietic (10.20%), lung (8.16%), bone (4.08%), skin and endometrium (2.04%). Table 1 shows the list of ophthalmic manifestations in the patients.
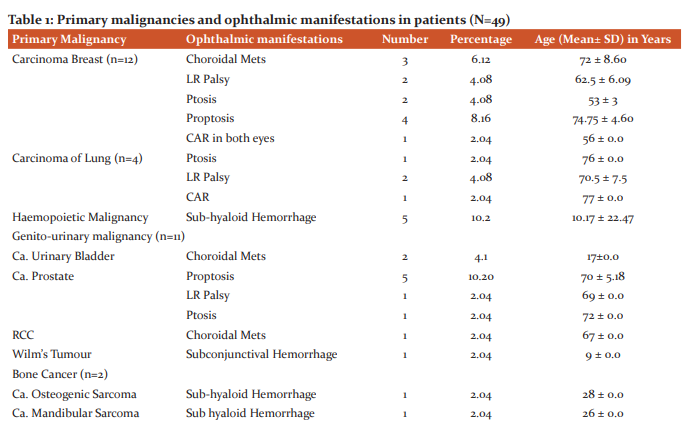

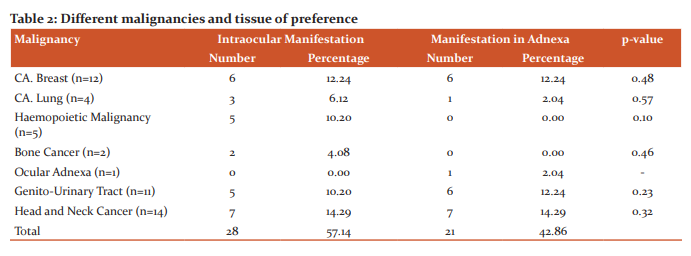
The different primary malignancies have different tissues of preference in the eye. The details are depicted in Table 2. More cases in the intraocular group 28 (57.14%) as compared to adnexa group 21(42.86%) respectively. There was no significant difference among any of the study variables (malignancies) with ocular manifestation (p>0.05).
Various malignancies affect different structures in the eye. Ca. the breast had ocular manifestation in the posterior segment (8.16%), adnexa (8.16%) and CNS manifestation (8.16%), but no manifestation in the anterior segment. Ca. Lung had ocular manifestation in the posterior segment (2.04%) and CNS manifestation (6.12%), but no manifestations in the anterior segment and adnexa. Haemopoietic malignancies (10.20%) and Bone cancers (2.04%) had ocular manifestation only in the posterior segment. The genitourinary tract had ocular manifestations in the anterior segment (2.04%), posterior segment (6.12%), adnexa (10.20%) and CNS manifestations (4.08%). Head neck cancers manifested in the adnexa (10.20%) and had CNS manifestations (18.37).
DISCUSSION:
This observational study was conducted on 225 patients. Ocular manifestations were seen in 49 (21.77%) patients. The mean age of these patients was 54.2 ± 22.39 years, of which 61% were males and 39% were females. Ocular metastasis is often detected late because the patients may not have any visual symptoms or the systemic symptoms may be too severe.5 Even in our study the majority of our patients, i.e., 41% presented within 6 months to two years of being diagnosed with malignancy. Around 37% presented later than two years. Shah et al., in their study of 187 patients with uveal metastasis from lung cancer reported that the mean age at presentation was 62 years. The mean interval between the diagnoses of lung cancer and uveal metastases was around 2.5 years.6
In our study, most of the ocular metastasis was from head and neck malignancy (28.57%), followed by breast (24.48%), genitourinary tract (20.40%), hematopoietic (10.20%), lung (8.16%), bone (4.08%), skin and endometrium (2.04%).
Among the head and neck cancers like Ca larynx presented with LR palsy (6.1%) and ptosis (4.1%), Ca Maxilla presented with proptosis (8.2%), Ca Ethmoid also presented with proptosis (2.04%), Temporal Lobe Glioblastoma presented with LR Palsy (2.04%), astrocytoma of the temporal lobe (R) and left parietal lobe astrocytoma presented with Papilledema (2.04% each), and left temporal lobe astrocytoma presented with optic atrophy (2.04%). Similar to our study, Yan and Gao in their retrospective study of 35 males and 11 females with a mean age of 47 years, also reported head and neck cancers (nasopharyngeal carcinoma, 30.34%) as the most common malignancy with ocular manifestations. Other head and neck cancers were medullary thyroid carcinoma (2.17%) and lacrimal gland carcinoma (2.17%). The most common ocular presentations were abnormal eye position (65.22%), followed by proptosis (63.04%), increased orbital pressure (54.35%), diplopia (54.35%), and decreased ocular motility (52.17%).7
The incidence of ocular metastasis with primary breast cancer ranges between 5 and 30%.8,9 In our study it was 24.48%. The most common ocular manifestation in breast carcinoma was proptosis, followed by choroidal METS, Lateral rectus palsy, ptosis, and retinopathy. Kreusel et al. reported intraocular metastasis in 4.6% of patients with breast cancer with the choroid being the most common site.9 Supriya and Lokesh reported a case of Exudative Retinal Detachment in a 38-year-old female with adenocarcinoma of the breast. It was characterized by the collection of sub-retinal fluid with no retinal breaks or traction. 10 Madanagopalan et al. reported a rare case of CRVO in a case of breast carcinoma where the retina showed extensive haemorrhages and dilated retinal veins. 11 Francone et al. 12 and Maliepaard et al. 13 reported cases where ocular metastases were the primary presentation of breast cancer.
The incidence of ocular metastasis with primary lung cancer is reported to be 0.2% to 7%.6,14 In our study it was 8.16%. Similar to our study, Yan and Gao reported an incidence of that 8.6%.7 In a review of 950 uveal metastases by Shields et al. the incidence of ocular metastasis with primary in the lung was reported in 21% cases.15 The most common ocular manifestations seen in our study were LR Palsy, Ptosis, and Carcinoma Associated with Retinopathy (CAR). They are more common in men. Contradictory to our study, Shah et al. reported that choroid was the commonest involvement (88%), followed by iris (10%) and ciliary body (2%).6 Hoang et al. and Hernández-Da Mota et al. reported ocular metastasis as first presentation in older male patients due to metastatic lung adenocarcinoma.16,17 Many case studies are reported where the first clinical presentation was ocular in case of primary in lung. 18,19
Ocular manifestations in haematological malignancies are well documented now. In our study, sub-hyaloid haemorrhage (10.2%) was the only ocular manifestation that was seen in such malignancies. Similar to our findings, Koshy et al. reported a prevalence of 10.4% for sub hyaloid haemorrhages in patients of acute/chronic leukaemia.20
Carcinoma of the Genito-urinary tract can also present with ocular metastasis. In our study, Ca Prostate presented with proptosis (10.20%), LR Palsy and ptosis (2.04% each), Ca Urinary Bladder presented with Choroidal Mets (4.1%), and RCC presented with Choroidal Mets (2.04%) too. Uluocak et al. reported a metastatic orbital cancer secondary to prostatic adenocarcinoma in a 73-year-old man presenting with a history of ipsilateral visual loss and one-sided proptosis, periorbital swelling, and pain. 21 Lefresne et al. also reported an 81-year-old man with poorly differentiated carcinoma prostate who presented with pain, proptosis, and blindness.22 Pompeu et al. reported two cases where one patient presented with a mass in the eye and another with an ulcerated lesion on the inferior tarsal conjunctiva both of whom had primary RCC. 23 Hart et al. reported a 70-year-old man with persistent lateral rectus mass and orbital haemorrhage after retrobulbar anaesthesia. On biopsy, the lesion was found to be metastatic RCC. 24 Patil et al. reported a case of a 43-year-old male with sudden onset of binocular diplopia on lateral gazes. The patient showed features of ipsilateral one?and?a?half syndrome and investigations further revealed primary RCC. 25 Mitsui et al. reported a case of a 43-year-old bladder cancer patient, 17 months post radical cystectomy with a choroidal disorder and multiple nodules in the abdomen and head. On biopsy, it was revealed as a metastasis from the bladder cancer. 26 In another case report by Wiltshire et al. an 88-year-old man presented with acute loss of vision due to choroidal metastasis. A diagnosis of primary urothelial carcinoma of the bladder was later made.27 Therefore, it is necessary that in an older male with visual and urinary symptoms, the genitourinary system should be evaluated as a potential primary site.
In our study, a case of Osteogenic Sarcoma and Mandibular Sarcoma presented with Sub hyaloid Hemorrhage (2.04% each). Very few case reports are published in this area. Agarwal A. reported a case of orbital metastasis presenting as proptosis in osteosarcoma.28 Rajabi et al. reported a case of a 55-year-old male known case of scapular bone osteosarcoma presenting with pain, decreased vision, proptosis, conjunctival injection, and chemosis.29
Other systemic malignancies that can present as ocular metastasis are the Gastrointestinal tract30 and skin. 31 In our study a patient presented with ocular symptoms like ptosis, exposure keratopathy, and optic atrophy whose primary was squamous cell Carcinoma of the lid. We found no ocular manifestation in Gastrointestinal malignancies.
CONCLUSION:
Ophthalmic manifestations were seen in 21.77% of patients with systemic malignancies. So, to conclude, the authors believe that all patients with systemic malignancies (primary and metastatic) should undergo a thorough ophthalmic examination regularly in a time framed manner to diagnose asymptomatic patients with ocular involvement at the earliest and prevent visual loss.
Acknowledgement: We acknowledge the contribution of our university and department for the unending support.
Conflict of Interest: There is no conflict of Interest
Source of Funding: No Source of Funding
Authors Contribution: This is a collaborative work among all authors. Khochikar Nilima .M. & Karambelkar V.H., performed the statistical analysis, wrote the protocol, and wrote the first draft of the manuscript. Khochikar Nilima M. managed the literature searches too. Both the authors read and approved the final manuscript.
References:
1. Bloch RS, Gartner S. The incidence of ocular metastatic carcinoma. Arch. Ophthalmol.. 1971 Jun 1;85(6):673-5.
2. Alswaina N, Elkhamary SM, Shammari MA, Khan AO. Ophthalmic features of outpatient children diagnosed with intracranial space-occupying lesions by ophthalmologists. Middle East Afr. J. Ophthalmol. 2015 Jul;22(3):327.
3. De Potter P. Ocular manifestations of cancer. Curr Opin Ophthalmol. 1998 Dec 1;9(6):100-4.
4. Georgalas I, Paraskevopoulos T, Koutsandrea C, Kardara E, Malamos P, Ladas D, Papaconstantinou D. Ophthalmic metastasis of breast cancer and ocular side effects from breast cancer treatment and management: mini-review. BioMed Res. Int.. 2015 May 11;2015.
5. Cohen VM. Ocular metastases. Eye. 2013 Feb;27(2):137-41.
6. Shah SU, Mashayekhi A, Shields CL, Walia HS, Hubbard III GB, Zhang J, Shields JA. Uveal metastasis from lung cancer: clinical features, treatment, and outcome in 194 patients. Ophthalmology. 2014 Jan 1;121(1):352-7.
7. Yan J, Gao S. Metastatic orbital tumors in southern China during an 18-year period. Graefe’s Arch Clin Exp Ophthalmol. 2011 Sep;249(9):1387–93.
8. Nelson CC, Hertzberg BS, Klintworth GK. A histopathologic study of 716 unselected eyes in patients with cancer at the time of death. Am. J. Ophthalmol. 1983 Jun 1;95(6):788-93.
9. Kreusel KM, Wiegel T, Stange M, Bornfeld N, Foerster MH. Intraocular metastases of metastatic breast carcinoma in the woman. Incidence, risk factors and therapy. Der Ophthalmologe: Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2000 May 1;97(5):342-6.
10. Supriya BN, Lokesh HM. A rare case of unilateral carcinoma of breast manifesting as an exudative retinal detachment-A case report. Res J Med Allied Heal Sci. 2019 2(2):28–9.
11. Madanagopalan VG, Selvam VP, Sivan NS, Govindaraju NV. Central retinal vein occlusion in a patient with breast carcinoma. GMS ophthalmology cases. 2019;9.
12. Francone E, Murelli F, Paroldi A, Margarine C, Friedman D. Orbital swelling as the first symptom in breast carcinoma diagnosis: a case report. J. Med. Case Rep. 2010 Dec;4(1):1-2.
13. Maliepaard M, Mesham M, Aleksic Z, Scholtz R, Edge J. Ocular metastasis as initial presentation in breast cancer. South African Med J. 2017 Aug 1;107(8):694–6.
14. Kreusel KM, Bechrakis NE, Krause L, Wiegel T, Foerster MH. Incidence and clinical characteristics of symptomatic choroidal metastasis from breast cancer. Acta ophthalmologica Scandinavica. 2007 May;85(3):298-302.
15. Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997 Aug 1;104(8):1265-76.
16. Hoang A, Khine KT, O’Rese JK, Tesser RA, Chesnutt DA. A rare ocular presentation of metastatic lung cancer: unilateral anterior chamber angle, bilateral choroidal, and multiple intracranial metastases. J. Glaucoma. 2017 Feb 1;26(2):e93-5.
17. Hernández-Da Mota SE, Ulaje-Nuñez JM, Salinas-Gallegos JL, Rodríguez-Reyes A. Iris metastasis as a first manifestation of lung adenocarcinoma. Archivos de la Sociedad Española de Oftalmología (English Edition). 2018 Jul 1;93(7):357-9.
18. Maturu VN, Singh N, Bansal P, Mittal BR, Gupta N, Behera D, Gupta A. Combination of intravitreal bevacizumab and systemic therapy for choroidal metastases from lung cancer: report of two cases and a systematic review of the literature. Medical Oncology. 2014 Apr 1;31(4):901.
19. Jiang K, Brownstein S, Sekhon HS, Laurie SA, Lam K, Gilberg S, Britton W. Ocular metastasis of lung adenocarcinoma with ELM4-ALK translocation: A case report with a review of the literature. Saudi J Ophthalmol. 2013 Jul 1;27(3):187-92.
20. Koshy J, John MJ, Thomas S, Kaur G, Batra N, Xavier WJ. Ophthalmic manifestations of acute and chronic leukaemias presenting to a tertiary care centre in India. Indian J. Ophthalmol. 2015 Aug;63(8):659.
21. Uluocak N, Suha Parlaktas B, Ersay Deniz F, Erdemir F, Dogan Koseoglu R, Gedar MO. Orbital metastasis of prostate cancer: a case report. Kaohsiung J Med Sci. 2007 Apr;23(4):199-202.
22. Lefresne S, Fairchild A, Johnson R, Deschenes J, Russell L, Pederson J. Genitourinary malignancy presenting as an ocular metastasis: a case report and review of the literature. Can Urol Assoc J . 2012 Apr;6(2):E67.
23. Pompeu AC, Arap S, Silva MN, Monteiro DS. Ocular metastasis as the first presentation of renal cell carcinoma: report of 2 cases. Clinics. 2005 Feb;60(1):75-8.
24. Hart RH, Luthert PJ, Rose GE. Renal cell carcinoma metastasis masquerading as a recurrent orbital haematoma. Orbit. 2005 Dec 1;24(4):281–4.
25. Patil M, Ganger A, Sharma S, Saxena R. Metastatic renal cell carcinoma presenting as a one-and-a-half syndrome. Indian J Ophthalmol. 2017 Sep;65(9):895.
26. Mitsui Y, Arichi N, Inoue K, Hiraki M, Nakamura S, Hiraoka T, et al. Choroidal and Cutaneous Metastasis from Urothelial Carcinoma of the Bladder after Radical Cystectomy: A Case Report and Literature Review. Case Rep Urol. 2014;2014:1–4.
27. Wiltshire KL, Laperriere N, Bristow RG. Prolonged survival in a patient with choroidal metastases from urothelial bladder cancer. Can J Urol. 2009 Aug;3(4): E36.
28. Agrawal A. Osteosarcoma metastasis to the orbit presenting as severe proptosis following trivial trauma. J Clin Ophthalmol Res. 2014 Sep 1;2(3):155.
29. Rajabi MT, Jafari H, Hosseini SS, Tabatabaie SZ, Rajabi MB, Amoli FA. Orbital metastasis: a rare manifestation of scapular bone osteosarcoma. J Ophthalmic Vis Res.. 2014 Oct;9(4):517.
30. Siddiqui MR, Hussain SZ, Mubarak M. Iris metastasis as the initial presentation of upper gastrointestinal tract carcinoma: a case report. J. Med. Case Rep. 2019 Dec;13(1):1-4.
31. Fishman ML, Tomaszewski MM, Kuwabara T. Malignant melanoma of the skin metastatic to the eye: frequency in autopsy series. Arch. Ophthalmol.. 1976 Aug 1;94(8):1309-11.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License