IJCRR - 7(21), November, 2015
Pages: 29-32
Date of Publication: 11-Nov-2015
Print Article
Download XML Download PDF
KNOWLEDGE AND AWARENESS OF CERVICAL CANCER AMONG WOMEN IN RURAL INDIA
Author: Arunadevi V., Geetha Prasad
Category: Healthcare
Abstract:Objectives: To assess knowledge and attitudes about HPV, cervical cancer and its screening among women using a structured questionnaire to obtain information. Methods: A cross: Section interview based survey was conducted in May 2015. Two hundred women attending a well women clinic were asked to complete a questionnaire assessing cervical cancer awareness and specific knowledge about prevention of the disease. Settings: Karpaga Vinayaga Institute of Medical Science and Research Centre. Results: Only 38% of the respondents were aware that cervical cancer is the most common cause of gynecological cancers. 63% were aware that infection is the most common cause of cervical cancer of these 49% said that virus is the cause and 16% of the respondents knew that the virus is Human Papilloma virus(HPV). 78% recognized pap smear as a screening test. In total only 13 out of 200 respondents were aware of HPV Vaccine. Conclusion: The low screening participation among Indian women may be due to limited awareness and knowledge about cervical cancer screening examinations. The universal application of Pap smears in western communities has lead to drastic decline in the number of invasive cancers of the cervix and higher detection of preinvasive lesions . Identification of factors determining participation, incorporating a comprehensive health education programme prior to screening, personal invitations, proximity of clinics to the target women all help in increasing the compliance.
Keywords: Conventional cytology, Chronic infection, Sophisticated equipment
Full Text:
INTRODUCTION
Cancer of the uterine cervix is the second most common cancer among women globally. An estimated 550,700 new cases and 286,823 deaths due to cervix cancer are estimated to have occurred in the year 2010. India alone accounts for one-fourth of the global cervix cancer burden.1 . Several tests have been developed to screen women for cervix pre-cancers and cancers. The choice of the test will depend on its technical performance, cost-effectiveness, the available resources and the socio cultural settings in which it is to be used.2 Conventional cytology based screening with pap smear test developed by George Papanicolaou has been the mainstay of cervical cancer prevention worldwide since the 1950’s. Pap test has repeatedly demonstrated good specificity ranging from 86% to 100%.3 . Cytology based screening programmes are labor intensive and logistically burdensome. They require multiple visits by the women for various reasons like screening, obtaining the results follow up investigations and treatment in case of abnormal smears. Thus, despite the low consumable cost, high quality cytology is expensive in absolute terms and may not necessarily be the most cost-effective option for screening.4 Chronic infection with oncogenic HPV is a necessary, but insufficient cause for the development of cervical cancer. Presence of Co-factors such as high parity smoking nutritional deficiency, hormonal contraceptive use and presence of other sexually transmitted infections increases the risk.5 Even today millions of women in the developing countries are never screened for cervical cancer in their entire lifetime. Routine cytological screening should be offered to all women above the age of 21 years who are active for atleast 3 years Screening combined with vaccination can substantially reduce the worldwide cervical cancer mortality. Effective implementation of sustainable cervical cancer screening programmes using sufficiently sensitive and specific tests that covers minimum 70% of the targeted population through screening atleast once in a lifetime along with effective treatment is vital in reducing the burden of cervix cancers.6 The purpose of the study was to assess the level and accuracy of public understanding about cervical cancer and its screening in India.
METHODS
The study was conducted in May 2015. A questionnaire based on the study objectives was designed and administered to 200 women attending a public clinic. The questionnaire consisted of the questions regarding the knowedge and awareness about different aspects of cervical cancer . Open ended questions were asked about the etiology, clinical features and prevention of cervical cancer with multiple responses. This study was approved by ethical committee.
RESULTS AND ANALYSIS
1 KNOWLEDGE ABOUT THE EPIDEMIOLOGY OF CERVICAL CANCER.
The result showed that 38% of the respondents recognized that cervical cancer is the most common malignancy in gynecological cancers, while 28% thought that it is moderately common and 34% thought that it is least common, 36% were aware that it is the second most common gynecological cancer leading to death.

2. Knowledge about the etiology of cervical cancer
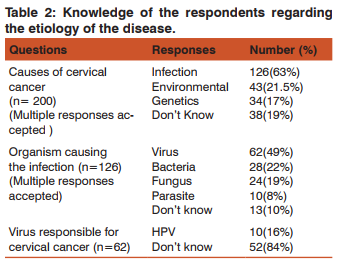
63% were aware that infection is one of the causes of cervical cancer, 21.5% said environment and 17% opted for genetics. 19% of the sample said that they “don’t know” the cause of cervical cancer. Of all the respondents who opted for infection 49% said virus is the cause of that infection, Other responses were bacteria (22%), fungus (19%) and parasite (8%). 16% of the study population who opted for virus were aware that HPV is that virus. None of the respondents were aware of the correct technique to detect HPV, which is PCR.
3. Knowledge about the risk factors and clinical features of cervical cancer.
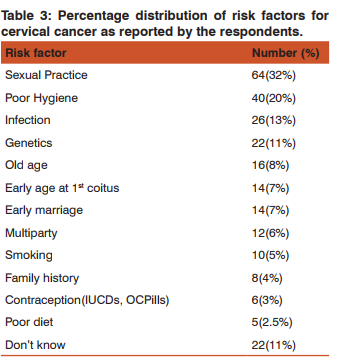
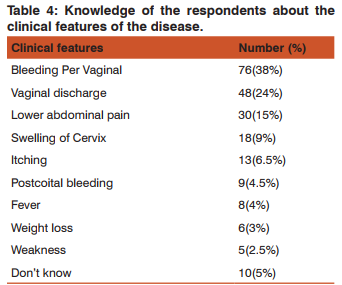
Sexual practice which included unprotected sex was the most common risk factors observed (32%). Most common presenting complaint reported was vaginal bleeding (38%) and vaginal discharge (24%). While few thought lower abdominal pain (15%), swelling of cervix (9%), itching (6.5%) could also be the initial symptoms patients with cervical cancer present with.
4. Knowledge about the treatment of cervical cancer
21% answered the correct treatment option which was “to treat according to the stage of the disease”. 34% were of the opinion that radiotherapy is required to cure cervical cancer, whereas 26% were in favour of surgery and 19% for chemotherapy
5. Knowledge about prevention of cervical cancer
78% of respondents were aware that pap smear is the screening test for cervical cancer. Ultrasonogram (14%), Biopsy(5%), Radiological scans (3%) were few of the incorrect responses observed. Majority of respondents were aware of the correct time to start screening which is after first coitus (62%). In total only 13 out of 200 were aware of the vaccine against HPV Majority of the respondents opted for health professionals (48%) and mass media (41%) as a source through which knowledge concerning cervical cancer, 11% found special lectures and conferences to be a good source to obtain information.
DISCUSSION
In India cancer of the cervix is number one killer cancer among women. It is estimated that during 2008, 134,420 new cases of cancer cervix occured in the country (incidence rate of 7 per lac population) and about 72,825 women died of the disease (mortality rate of 15.2 per lac population). It comes to 23.3 percent of all cancer deaths in women and about 11.4 percent of total cancer deaths in the country.7 . Liquid based cytology (LBC) is more expensive than conventional cytology and requires additional supplies and sophisticated equipment. In a meta-analysis comparing conventional pap with LBC no difference was found in the relative sensitivity. But, a lower pooled specificity was found for LBC when presence of atypical squamous cells of undetermined significance (ASCUS) and above were included (ratio 0.91, 95% CI: 0.84-0.98).8 . The evidence base in support of visual based screening methods has emerged from several studies conducted in different developing countries demonstrating comparable or greater sensitivity of visual inspection of the cervix with naked eye (after application of acetic acid (VIA) or lugol, s iodine (VILI) than that of cytology. The test characteristics of VIA have been evaluated from several cross sectional studies in India, Africa and china, wherein the sensitivity range from 67% to 79% and the specificity range from 49-86% 9 . The sensitivity and specificity in a pooled analysis of eleven cross – sectional studies were 76.8%(range, 56.1-93.9%) and 85.5% (range 74.2-93.8%) for VIA and 91.7% (range, 76.0-97.0%) and 85.4% (range, 73.0-91.3%) for VILI respectively.10 VIAM (performing VIA under low magnification) has similar sensitivity and specificity as compared with VIA and does not have any added benefit over VIA.11. The results of cluster randomised controlled trial in southern India, after a single round of screening using VIA followed by treatment in the same visit, when appropriate, show a significant 25% reduction in cervical cancer incidence and a significant 35% reduction in cervical cancer mortality at the end of seven years of follow up.12 Another cluster randomised controlled trial of cervix cancer screening in Mumbai, India, demonstrated a significant down staging of cervix cancers in the intervention arm.13 Though a single round of VIA screening did not show decrease in the incidence of advanced cervical cancer and significant mortality reduction after eight years of initiation of the osmanabad trial14, the same may be evident after few more years of follow-up. The Mumbai cross-sectional study concludes that parallel testing with both VIA and VILI should be considered where good quality cytology is not feasible and that the sensitivity of cytology and HPV testing can be significantly increased by adding the visual test.15. Visual tests are not reliable in postmenopausal women because of changes in the transformation zone of the cervix the area in which precursors of cervical cancer arise.16,17. Genital HPV infection is the most common viral sexually transmitted infection (STI) and affects roughly 80% of sexually active people. In most cases HPV infection is cleared by the cell mediated immune system within 1-2 years of exposure.18. The median time of clearance of HPV infections detected during screening studies is 6-18 months.19. The small proportion (about 10%) of carcinogenic infections persisting for several years is strongly linked to a high absolute risk of diagnosis of precancer.20.
CONCLUSION
More than 85% cases and 88% deaths from cervix cancer occur in developing countries, where women often lack access to cervical cancer screening and treatment. Choosing a suitable screening test with good efficacy and one which is replicable, affordable, feasible for implementation with respect to available technical expertise and manpower is an important aspect of a screening program . Highly effective HPV prophylactic vaccines are now available for prevention of cervix cancers. Hence, early detection and treatment needs to be continued for millions of women who are already infected and who may not receive vaccination in the near future.
ABBREVIATIONS:
HPV- Human Papilloma Virus
STI- Sexually Transmitted Infections
VIA- Visual Inspection of Acetic acid
VILI-Visual Inspection of Lugol’s Iodine
VIAM- Visual Inspection of Acetic acid under low Magnification
ICUD-Intra Uterine contraceptive Device
OCP- Oral contraceptive Pills
LBC- Liquid Based Cytology
ASCUS- Atypical Squamous Cells of Undetermined Significance
ACKNOWLEDGEMENT
Author acknowledges the enormous help received from the scholars whose articles have been cited and incorporated in references. Author is also grateful to authors/editors/publishers of all those articles journals and books from where the literature for this articles has been reviewed and discussed.
References:
1. Farley J, Shin HR, Bray F, Forman D, Mathers C and Parkin DM. GLOBOCAN 2008, Cancer Incidence and Mortality Worldwide: Lyon, France,: International Agency for Research on Cancer ; 2010.
2. Kitchener HC, Castle PE, Cox JT. Chapter 7: Achievements and limitations of cervical cytology screening, Vaccine 2006; 24,3: S63-S70.
3. Nanda K, McCrory D, Myers E et al. Accuracy of the papanicolaou test in screening for and follow up of cervical cytological abnormalities: a systematic review. Ann Intern Med 2000 ; 132:810-9.
4. Goldie SJ, Gaffikin L, Gold haber – Fiebert JD, et al. Cost – effectiveness of cervical , cancer screening in five developing countries. N Eng J Med 2005:353:2158-68.
5. Munoz N. Castellsague X, de Gonzalez AB, Gissmann L, Chapter 1: HPV in the aetiology of human cancer. Vaccine 2006 ; 24,3:S3/1-10. Epub 2006 Jun 23.
6. Gravitt PE, Belinson JL , Salmeron J ,et al. Looking ahead a case for human papillomavirus testing of self sampled vaginal specimens as a cervical cancer screening strategy, Int J cancer 2011:129:517-27.
7. GLOBOCAN 2008, India Fact sheet, 2010 Section of Cancer Information International angency for Research on cancer, Lyon, France.
8. Arbyn M , Bergeron C, Klinkhamer P, etal. Liquid compared with conventional cervical cytology; a systematic review and meta analysis. Obstet Gynecol 2008:111:167-77.
9. Sankaranarayanan R, Gaffikin L, Jacob M, et al. A critical assessment of screening methods for cervical neoplasia. Int J Gynaecol obstet. 2005:89:84-12.
10. Sankarnarayanan R, Basu P, Wesley RS, et al . Accuracy of visual screening for cervical neoplasia. Results from an IARC multicentre study in India and Africa. Int J cancer 2004:110:907- 13.
11. Sankaranarayanan R, Shastri SS , Basu P, et al. The role of low level magnification in visual inspection with acetic acid for the early detection of cervical neoplasia, Cancer Detect Prev 2004 :28:345-51.
12. Sankaranarayanan R, Esmy PO, Raj Kumar R, et al, Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu , India :a cluster-randomised trial, Lancet 2007;370;398-406.
13. Mittra I , Mishra GA, Singh S, et al A Cluster Randomized controlled Trial of Cervix and Breast Cancer Screening in Mumbai, India; Methodology and Interim Analysis after Three round of Screening. Int J Cancer 2010; 126; 976-84.
14. Sankaranarayanan R, Nence BM , Shastri SS, et al HPV screening for cervical cancer in rural India , N Engl J Med 2009; 306;1385-94.
15. Shastri SS, Dinshaw KA, Amin G, et al Concurrent evaluation of visual , Cytological and HPV testing as screening methods for the early detection of cervical neoplasia in Mumbai , India. Bull world Health organ 2005; 83; 186-94.
16. Colposcopy and Treatment of cervical Intraepithelial Neoplasia : A Beginner, s Manual , Edited by sellors JW and Sankaranarayanan R. IARC 2003-04.
17. Sherris J, Wittet S, Kleine A, et al Evidence – Based, Alternative cervical Cancer Screening Approaches in Low – Resource settings. Int. Perspect Sex Reprod Health 2009;35;147-52.
18. Stanley M. Immune responses to Human Papillomavirus, Vaccine 2006; 24 ;S16-22
19. Plummer M, Schiffman M, Castle PE, et al A 2-Year Prospective study of HPV persistence among women with ASCUS or LSIL cytology, J Infect Dis 2007; 195; 1582-9
20. Schiffman M, Herrero R, Desalle R et al The carcinogenicity of human papilloma virus types reflects viral evolution, Virology 2005; 337; 76-84.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License