IJCRR - 13(16), August, 2021
Pages: 175-178
Date of Publication: 30-Aug-2021
Print Article
Download XML Download PDF
Study of Association of Hba1c Levels with RDW and MCV in Patients of Type 2 Diabetes Mellitus in a Tertiary Care Center\"
Author: Singh S, Arora S, Sharma A, Bali IK
Category: Healthcare
Abstract:Introduction: Diabetes mellitus is one of the most common metabolic disorders and the degree and duration of hyperglycemia are related to the risk of macro-vascular and micro-vascular complications which are responsible for the morbidity and mortality associated with the disease. HbA1c (glycosylated haemoglobin) is measured as an index of glycemic control over the past 2-3 months. Red cell distribution width (RDW) and mean corpuscular volume (MCV) are components of routine complete blood counts (CBC). Increased HbA1c levels may cause structural and functional changes in the haemoglobin molecule and the red blood cell because of which RDW and MCV may be altered. This study aims to assess the association of HbA1c levels with RDW and MCV in patients with type 2 diabetes mellitus. Methods: A prospective, hospital-based, observational study of 6 months from March 2020 to August 2020 including 104 patients with type 2 diabetes mellitus (both new and previously diagnosed patients undergoing treatment) was done. Diabetes mellitus was diagnosed according to ADA (American Diabetic Association) guidelines- HbA1c≥6.5% (48 mmol/mol) or FBS≥126 mg/dl (7.0 mmol/L) or 2 hour postprandial glucose≥ 200 mg/dl (11.1 mmol/L) on oral glucose tolerance test or RBS≥ 200 mg/dl (11.1 mmol/L) with symptoms. Results: Out of the 104 patients, 63 were males (60.6%) and 41 were females (39.4%). Most of the patients (30.8%) were in the age group of 41-50 years followed by 51-60 years(29.7) by There was a significant positive correlation between RDW and HbA1c values (p=0.003) while the other parameters did not show any significant correlation. Interpretation & Conclusion: In the present study we found that as the HbA1c values increased there was a concordant increase in RDW values (p=0.003). More studies, with a larger sample size, will further help to explain the correlation between RDW and HbA1c.
Keywords: HbA1c, RDW, MCV, Type 2 diabetes mellitus, Metabolic disorder, Hyperglycemia
Full Text:
INTRODUCTION
Diabetes mellitus is of one of the most common metabolic disorders whose incidence is on the rise globally due to increase in sedentary lifestyle, obesity, and elderly population. The associated macro-vascular and micro-vascular complications are majorly responsible for the morbidity and mortality associated with the disease 1. The degree and duration of hyperglycemia is related to the risk of these complications. HbA1c (glycosylated hemoglobin) is measured as an index of glycemic control over past 2-3 months 2. Hyperglycemia has several effects on RBCs like reduced deformability, increased adhesion and increased osmotic fragility leading to changes in erythrocyte structure apart from glycosylation of hemoglobin 3. Red cell distribution width (RDW) is a component of routine complete blood counts (CBC) and is a measure of variability in size and heterogeneity of erythrocytes. Mean corpuscular volume (MCV) is also a component of routine CBC. Increased HbA1c levels may cause structural and functional changes in the hemoglobin molecule and the red blood cell because of which RDW and MCV may be altered 4,5.
The aim of this study is to assess the association of HbA1c levels with RDW and MCV in patients of type 2 diabetes mellitus.
METHODS
A prospective, observational, hospital-based study was undertaken in the Pathology Laboratory of SGT Hospital for a period of 6 months from March 2020 to August 2020.104 patients with type 2 diabetes mellitus attending the medicine OPD of SGT Hospital were selected for the study. Both new and previously diagnosed patients undergoing treatment were included in the study. Diabetes mellitus was diagnosed according to ADA (American Diabetic Association) guidelines- HbA1c≥6.5% (48 mmol/mol) or FBS≥126 mg/dl (7.0 mmol/L) or 2 hour postprandial glucose≥ 200 mg/dl (11.1 mmol/L) on oral glucose tolerance test or RBS≥ 200 mg/dl (11.1 mmol/L) with symptoms 6.
The vitals of the patients were documented, and venous sample was withdrawn and sent for HbA1c and CBC investigations. RDW and MCV were noted from the CBC done using Automated 6-part Hematology Analyzer by flow cytometry method and HbA1c was measured using Automated Hemoglobin Analyzer using cation-exchange HPLC method. The data was tabulated with details of age, gender, RDW, MCV and HbA1c of each case.
The cases were classified into 3 categories based on HbA1c as good glycemic control (HbA1c ≤7%), poor control (HbA1c between 7.1-9%) and uncontrolled (HbA1c ≥9.1%); 2 categories for RDW (≤14.0 and >14.0) and 3 categories for MCV (<80fl, 80-100fl and >100fl) as per the laboratory reference range.
Approval for waiver of patients consent and patient information sheet was obtained from Institutional Ethical Committee [National Ethical Guidelines by ICMR on biomedical research 2017, chapter 5, Informed consent process Box 5.2 (Conditions for granting waiver of consent)] since the study involved the data available in the record that were anonymized and coded to delink with any identity of patient7.
Inclusion criteria
1. Previously diagnosed cases of type 2 diabetes mellitus
2. Newly diagnosed cases of type 2 diabetes mellitus
Exclusion criteria
-
Patients with any history of anemia of any cause
-
Patients with any haemoglobinopathy
-
Patients with chronic liver disease
-
Patients with type 1 diabetes mellitus
-
Patients with any acute or chronic infections like malaria, tuberculosis or malignancy
Data was analyzed and statistically described in terms of mean and standard deviation. Correlation was done using Chi-square test where a p value≤ 0.05 was considered statistically significant.
RESULTS
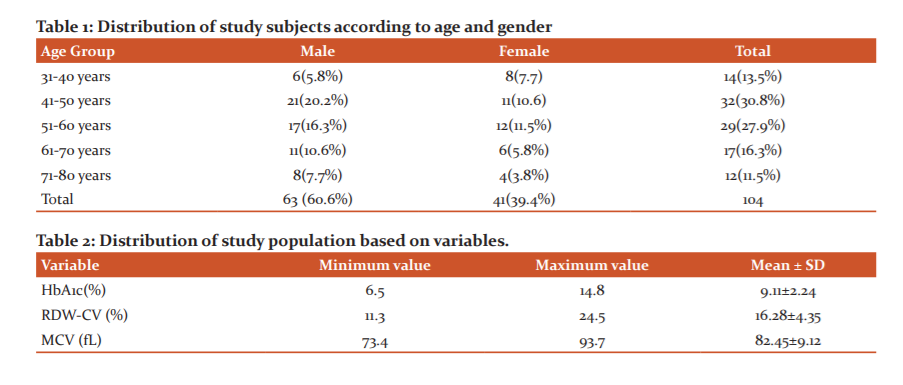
Out of the 104 patients, 63 were males (60.6%) and 41 were females (39.4%). The mean age was 47.24±11.0, the youngest patient being 32 years and the oldest being 78 years. Most of the patients (30.8%) were in the age group of 41-50 years (Table 1).
The mean duration of diabetes mellitus was 4.73±3.75 (range 0-20) years. The HbA1c of the study population was found moderately uncontrolled and the mean HbA1c was 9.11±2.24, the lowest being 6.5 and the highest being 14.8. The mean RDW was 16.28±4.35, the lowest being 11.3 and the highest being 24.5. The mean MCV was 82.45±9.12, the lowest being 73.4 and the highest being 93.7 (Table 2).
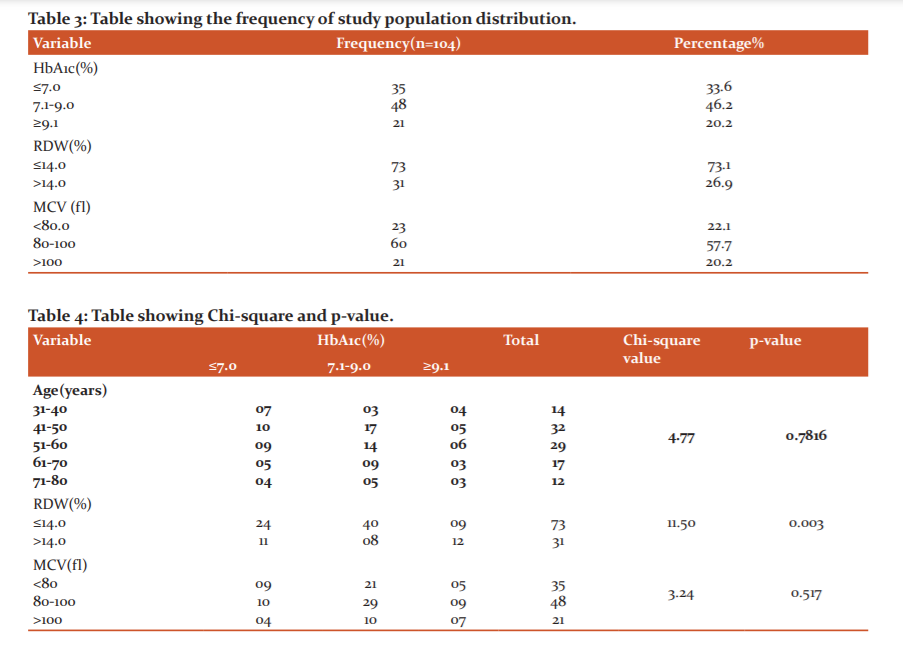
Amongst the study population, 46% patients had HbA1c values between 7.1-9.0, followed by 34% and 20% patients with HbA1c values ≤7.0 and ≥9.1, respectively. RDW was ≤14.0 for 73% patients while >14.0 for 27% patients. Majority of the patients (58%) had MCV value between 80-100 fl (Table 3).
There was a significant positive correlation between RDW and HbA1c values (p=0.003); as the HbA1c values increased there was a rise in RDW values of the patients. The correlation of HbA1c with age (p=0.78) and MCV (p=0.51) did not show any significant correlation (Table4).
DISCUSSION
Diabetes mellitus has become a major contributor to global morbidity as persistent hyperglycemia leads to various life-threatening complications 8. HbA1c measurement is a routine part of standard diabetes diagnosis and management regimes 9. RDW and MCV are reported routinely with CBC.
In this study we found significant correlation of RDW with HbA1c (p=0.003). In a study done by Suryavanshi C et al., 2015 similar observations were documented with a mild inverse correlation (r=-0.235, p=0.001)10 and in a study done by Sherifet al., 2013 positive correlation between HbA1c and RDW was noted which was not statistically significant (p=0.92) 11. Chowta et al., 2013 found in a study that RDW of elderly diabetics (>60 years) was higher than that of the younger patients and was statistically significant (p=0.002) 12 and Yin et al., 2018 also showed in a study the there was an association between RDW and poor glycemic control in established patients of type 2 diabetes mellitus which is in concordance with the results obtained in this study 13.
There was no significant correlation of HbA1c with MCV in this study. Hardikeret al.., 2012 in a study of non-diabetic population showed an inverse correlation between HbA1c and MCV (r=-0.22, p<0.05) 14 and Koga et al.., 2007 showed inverse association of HbA1c with MCV (r=-0.368, p<0.0001) in non-diabetic premenopausal women but no such association in post-menopausal women (r=-0.019, p=0.771) 15. In a study done by Glesbyet al.., 2010 on diabetic women with HIV infection, there was an inverse correlation between HbA1c and MCV 16.
CONCLUSION
Diabetes mellitus is a life- long disease and a major health concern in both developed as well as developing countries, hence early diagnosis and treatment is essential. Our study showed that RDW has a significant correlation with HbA1c (p=0.003) and as the HbA1c values increased there was a concordant increase in RDW values. Hence, RDW along with HbA1c can be used as a cheap, freely available routine diagnostic tool as a predictive marker of glycemic control and more studies, with larger sample size will further help to explain its role in glycemic monitoring in diabetic patients. RDW with HbA1c values when with in normal limit may be considered as a marker of glycemic control and when abnormal, be a prognostic marker for future complications such as cardiovascular disease or diabetic nephropathy in diabetic individuals.
Limitation of the study:This study only included the patients who came to the hospital for treatment. There is a need for evaluation of a greater population suffering but not yet diagnosed from type 2 diabetes mellitus in the community as the population is incognizant to their illness and the morbidity associated with it. Hence, screening programs for type 2 diabetes mellitus needs to be organized at the community level for early diagnosis of the disease so that the associated microvascular and macrovascular complications can be delayed if not avoided.
Acknowledgement - Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of interest: None
Funding information: None
Authors’ contribution: Shivangi Singh was responsible for the conception of the work, data interpretation and drafting the article. Aparajita Sharma was involved in data collection and analysis. Sunil Arora and IrbinderKour Bali supervised the work, provided critical feedback and guidance wherever required. All authors discussed the result and commented on the manuscript.
References:
1. Malandrino N, Wu WC, Taveira TH, Whitlatch HB, Smith RJ. Association between red blood cell distribution width and macrovascular and microvascular complications in diabetes. Diabetologia.2012;55:226-35.
2. Rodriguez-Manas L, Arribas S, Giron C, Villamer J, Sanchez-Ferrer C, Marin J. Interference of glycosylated human hemoglobin with endothelium-dependent responses. Circulation.1993;88(5):2111-6
3. Cho YI, Mooney MP, Cho DJ. Hemorrheological disorders of diabetes mellitus. J Diabetes Sci Technol.2008;2:1130-8
4. Syemeonidis A, Athanassiou G, Psiroyannis A, Kyriazopoulou V, Kapatais-Zoumbos K, Missirlis Y, Zoumbos N. Impairment of erythrocyte viscoelasticity is correlated with levels of glycosylated hemoglobin in diabetic patients. Clin Lab Haematol.2001;23:103-9
5. Livshits L, Srulevich A, Raz I, Cahn A, Barshtein G, Yedgar S, Eldor R. Effect of short-term hyperglycemia on protein kinase C alpha activation in human erythrocytes. Rev Diabet Stud.2012;9:94-103
6. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 2020;43(1):14-31
7.National Ethical Guidelines by ICMR on biomedical research 2017, chapter 5, Informed consent process Box 5.2 (Conditions for granting waiver of consent)
8. Jabeen F, Rizvi HA, Subhan A. Effect of hyperglycemia on superoxide dismutase defense system and erythrocyte indices in diabetic patients. Pak J Biochem Mol Biol.2012;45(2):85-9
9. Nathan DM. International Expert Committee report on the role of A1c assay in the diagnosis of diabetes. Diabetes Care.2009;32:1327-34
10. Suryavanshi C, Manjula SD, Ragini B, Raghavendra RK. Association of increased levels of glycated hemoglobin with variations in red blood cell parameters in diabetes mellitus. Int J Adv Res.2015;3(6):31-7
11. Sherif H, Ramadan N, Radwan M, Hamdy E, Reda R. Red cell distribution width as a marker of inflammation in type 2 diabetes mellitus. Life Sci J.2013;10(3)1501-7
12. Chowta N, Shenoy A, Adhikari P, Chowta M. Analysis of hemogram profile of elderly diabetics in a tertiary care hospital. Pharmacology, Neurological Diseases. International Journal of Nutrition.2013;3(2):126-36
13. Yin Y, Ye S, Wang H, Li B, Wang A, Yan W, Mu Y. Red blood cell distribution width and the risk of being in poor glycemic control among patients with established type 2 diabetes. Theraputics and Clinical Risk Management.2018;14:265-73
14. Hardiker PS, Joshi SM, Bhat DS, Raut DA, Katre PA, Lubree HG et al.. Spuriously high prevalence of prediabetes diagnosed by HbA1c in young Indians partly explained by hematological factors and iron deficiency anemia. Diabetes CARE.2012;35(4):797-802
15. Koga M, Morita S, Saito H, Mukai M, Kasayama S. Association of erythrocyte indices with glycated hemoglobin in pre-menopausal women. Diabetic medicine: A journal of the British Diabetic Association.2007;24(8):843-7
16. Glesby MJ, Hoover DR, Shi Q, Danoff A, Howard A, Tien P, Merenstein D et al.. Glycylated hemoglobin in diabetic women with and without HIV infection: data from the Women’s Interagency HIV Study. Antivir Ther.2010;15(4):571-7
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License