IJCRR - 13(16), August, 2021
Pages: 109-112
Date of Publication: 30-Aug-2021
Print Article
Download XML Download PDF
Minimally Invasive Surgery for Pulmonary Spindle Cell Carcinoma - Uncommon Aggressive Variant
Author: Kuppan CT, Balasubramanian VM, Jagadesh CB, Suhaildeen KM
Category: Healthcare
Abstract:Introduction and Importance: Spindle cell carcinoma (SpCC) of the lung is a rare type of lung malignancy with a poor prognosis. Only a limited number of cases have been reported worldwide and no established treatment protocol is available at present. Case Presentation: We report a case of a 71-year-old elderly lady, incidentally detected with a lung mass on routine medical evaluation. Preoperative biopsy was suggestive of non-small cell lung cancer, PET-CT was suggestive of localised disease with no mediastinal lymph node. The patient underwent modified uniportal VATS left lower lobectomy with systemic mediastinal lymph node dissection. Postoperative biopsy was suggestive of spindle cell carcinoma lung (pT3N0). At 6 months follow-up, the patient is doing well. Conclusion: We report the first case of successful modified uniportal VATS assisted surgical resection in this poor prognostic type of lung cancer.
Keywords: Lung cancer, Video-assisted thoracoscopy, Uniportal VATS, Non-small cell lung cancer, Spindle cell carcinoma, Minimal invasive surgery
Full Text:
Introduction:
Pulmonary sarcomatoid carcinoma (PSC) is a very rare variant that accounts for less than 1% of all lung malignancies. Spindle cell carcinoma of the lung is a type of pulmonary sarcomatoid carcinoma.1 It is a very rare entity with only a limited number of cases have been reported worldwide. It presents with diagnostic difficulty and has an aggressive clinical course with no separate established treatment protocol.
Minimally invasive management of lung cancer has become the standard of care, whenever feasible. Uniportal Video-Assisted Thoracoscopic Surgery (VATS) is a minimally invasive modality, which has been increasingly used in the surgical management of lung cancer. Here we describe a case of an elderly female patient with the aggressive spindle cell carcinoma of the lung who was successfully managed surgically with modified Uniportal VATS (left lung lower lobectomy + systematic mediastinal lymph node dissection). This proves the efficacy of uniportal VATS surgery even in aggressive operable lung cancer. Surgical management is an appropriate treatment even for early-stage sarcomatoid variant lung cancer. A minimally invasive approach is a viable option even in this aggressive variant.
Case History:
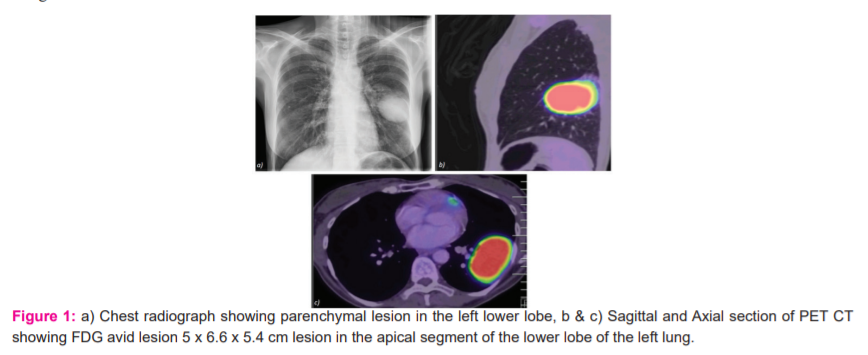
A 71-year-old asymptomatic female, the non-smoker, was incidentally detected with a left lung lower lobe consolidation on routine health evaluation. The patient was a known hypertensive and diabetic with coronary artery disease. General physical examination was unremarkable. On systemic examination, there was decreased air entry on the left side. Chest radiograph revealed a homogenous left parenchymal mass (Fig. 1a). Contrast-Enhanced Computer Tomography (CECT) Thorax revealed a large 5 x 6.6 x 5.4 cm lesion in the apical segment of left lung lower lobe with adjacent focal consolidation. An image-guided core needle biopsy was suggestive of non-small cell lung cancer. Positron Emission Tomography (PET) showed a lesion of the lower lobe of left lung, with no mediastinal lymphadenopathy and distant metastasis (Fig. 1b, c).
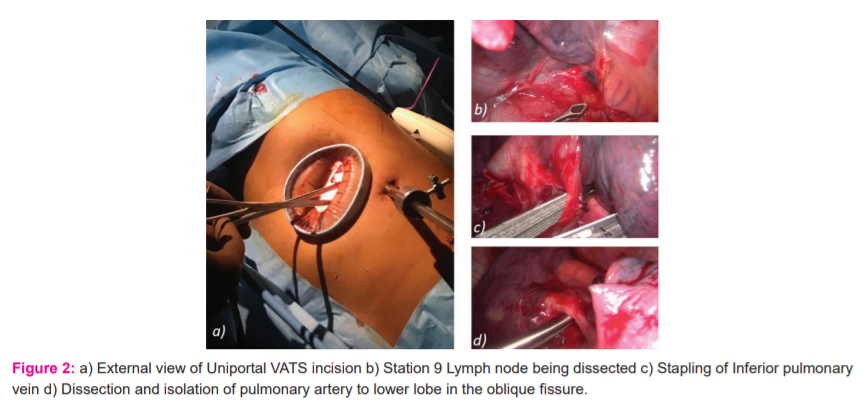
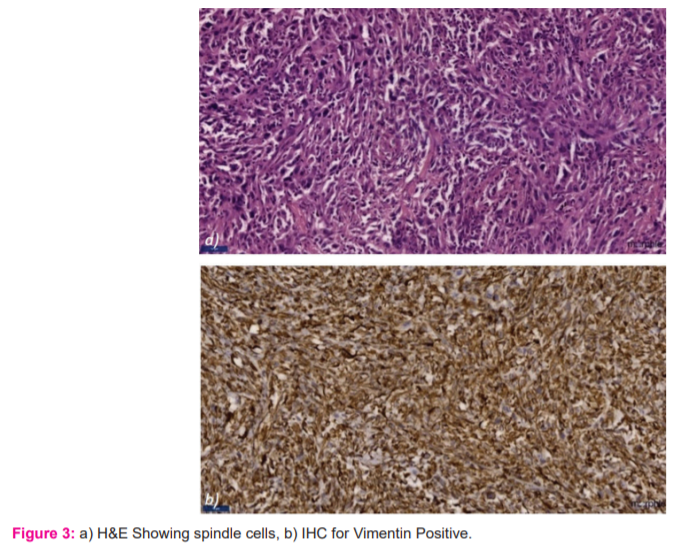
After discussing in the Multidisciplinary Tumour board, the patient was taken up for Uniportal VATS Left lung lower lobectomy with an additional camera port. A single 4 cm long incision was given in the left lateral 5th intercostal space in the anterior axillary line at intercostal space. Skin incision deepened and the pleural cavity entered. A wound protector was used to keep the incision wide open and no rib spreading was done (Fig. 2a). An additional camera port was placed in 7th Intercostal space in the midaxillary line. No pleural deposits or effusion was seen. Tumor of 5 x 6 cm was found in the apical-basal segment of the lower lobe left lung. Pleura was released anteriorly and posteriorly. Inferior pulmonary ligament released and lymph node station 9 removed (Fig. 2b). Inferior pulmonary vein isolated and looped and divided using Endo GIA 45mm-2.5mm stapler (Covidien Articulating reload with Tri-state technology) (Fig. 2c). The branch of the pulmonary artery to the lower lobe was defined in the fissure and the same was looped and divided (Fig. 2d). Bronchus was isolated and clamped. Lung was inflated to check the aeration of the upper lobe of the lung. Bronchus divided using Endo GIA 45mm-4.5mm stapler (Covidien Articulating reload with Tri-state technology). Specimen removed using specimen bag. Lymph node stations 8,7 removed. Pleura over the arch of aorta opened superiorly and station 5, 6 lymph node cleared and sent separately. Hemostasis secured and drains placed. The postoperative stay was uneventful. On a postoperative day one - the patient started on a normal diet and mobilized out of bed. Postoperative day 3 antibiotics were stopped. On postoperative day 5, the intercostal drain was removed and discharged on postoperative day 6. Postoperative pain was scored on visual analog score (ranging from 0-10) and was scored 3 on the first postoperative day and 2 at the time of discharge. Postoperative biopsy was Spindle cell carcinoma of the lung pT3N0 [as per AJCC 8th edition],2 with margins free of tumor and no lymph nodal involvement. On immunohistochemistry, the tumor was positive for Vimentin and CK-7, focally for TTF1 and negative for CK 20, p63, Napsin A, Synaptophysin and Chromogranin (Fig. 3). The patient has advised chemotherapy but the patient was not willing. On follow up patient is asymptomatic, disease-free after 8 months disease-free interval.
Discussion:
Video-Assisted Thoracoscopic Surgery (VATS) has become the standard of care with its oncological efficacy proven compared to conventional thoracotomy. Uniportal VATS is a modification of the multiport VATS surgery introduced about a decade earlier by Diego.3 It involves the use of a single utility incision of ~4 cm length to perform the entire surgery. Instruments are introduced through this single incision along with the camera to perform the surgical procedure. It scores over the multiport vats because it causes lesser injury to the intercostal nerves and thus lesser postoperative pain. However, it is technically demanding to perform. The other advantage is the direct vision of the hilum, which enables the surgeon to take better control of the hilar structures. Many articles have been published confirming the safety and oncological outcomes of uniportal VATS.4 In our study, we also found the patient to have a low postoperative pain score on day one and at the time of discharge. Even with multiple comorbid conditions and elderly age, the patient had an uneventful recovery due to the minimally invasive nature of surgery.
Spindle cell carcinoma of lung, which accounts for only 0.2 - 0.3 % of all lung malignancies, occurs in the elderly age group with a male preponderance, associated more with smokers.5 Based on a PubMed search done on 18/8/2020 with the phrase “pulmonary”, “Spindle cell carcinoma” and “Lung” there were only 28 articles that have been reported so far.
Clinical presentation of Spindle cell carcinoma of the lung is similar to other types of lung cancer, with about 50% of presenting with Cough, hemoptysis, and dyspnoea.6 Preoperative histologic identification of these tumours remains difficult. It requires examination of the resected surgical specimen since these are highly heterogeneous group of tumors which requires a minimum sarcomatoid component of 10% for a positive diagnosis. In light of this mixed multicellularity and the variations in the percentages of the cell types, no preoperative technique permits accurate tumor diagnosis.7 The expression of cytokeratin and epithelial membrane antigen are needed for demonstrating epithelial differentiation of sarcomatoid components.8
Since these are very rare tumors, currently patients with spindle cell carcinoma are managed similarly to Non-small cell lung carcinoma (NSCLC). Patients with localized lesions are treated with surgical resection followed by adjuvant therapy based on the histopathological diagnosis. Chemotherapy is given for patients with advanced or metastatic SpCC. However, the efficacy is poor and the patient's survival is limited to 5 to 6 months.9 A Study done by Roesel C et al. showed an overall 1-, 3- year survival rates were 57.7 and 35.8% of all operated cases respectively which is comparatively lesser/poorer compared to other Non-small cell lung carcinoma.5 UVATS has been proven to be a feasible and optimal treatment approach for patients with early-stage NSCLC by achieving similar results compared to multiportal VATS in terms of oncological efficacy and also providing better postoperative outcomes providing better pulmonary function outcome and reducing postoperative pain by minimizing trauma caused by surgery leading to a lesser hospital stay and faster return to daily activities.10 Our patient had the whole surgery done with modified UVATS and this is to our knowledge is the first report of successful use of this approach in such an aggressive type of lung cancer.
Conclusions:
Pulmonary spindle cell carcinoma is a neoplasm with an unfavorable prognosis through clinical symptoms and imaging findings are similar to other lung cancers. Minimally invasive surgery using uniportal VATS is feasible and safe even for aggressive variants of lung tumors. Spindle cell carcinoma of lung is an aggressive variant of lung cancer that is difficult to diagnose histologically and has a comparatively poor prognosis even after multimodality treatment. As a highly malignant carcinoma, efforts should be made to avoid misdiagnosis. Hence expertise in histopathological diagnosis is required for diagnosis. Even in early-stage tumors, the prognosis is more reserved than in other NSCLC because of their greater aggressiveness, high metastatic potential, and chemoresistance.
Acknowledgment:
The authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to the editors of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Source of Funding:
Nil
Conflict of Interest:
Nil
Authors’ Contribution:
Kuppan C T – Data collection, Writing the manuscript, Study design.
V Balasubramanian – Data collection, Writing the manuscript, Study design, Final draft correction and review
S Jagadesh Chandra Bose– Study design, Final draft correction and review
K Suhaildeen –.Data collection, Writing the manuscript, Study design
References:
1. Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol. 2015 Sep 1;10(9):1243–60.
2. Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, et al. editors. AJCC Cancer Staging Manual [Internet]. 8th ed. Springer International Publishing; 2017 [cited 2020 Sep 12].
3. Gonzalez D, Delgado M, Paradela M, Fernandez R. Uni-incisional video-assisted thoracoscopic left lower lobectomy in a patient with an incomplete fissure. Innovations (Phila). 2011 Jan;6(1):45–7.
4. Bertolaccini L, Batirel H, Brunelli A, Gonzalez-Rivas D, Ismail M, et al. Uniportal video-assisted thoracic surgery lobectomy: a consensus report from the Uniportal VATS Interest Group (UVIG) of the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg. 2019 Aug 1;56(2):224–9.
5. Roesel C, Terjung S, Weinreich G, Hager T, Chalvatzoulis E, et al. Sarcomatoid carcinoma of the lung: a rare histological subtype of non-small cell lung cancer with a poor prognosis even at earlier tumour stages. Interact Cardiovasc Thorac Surg. 2017 Mar 1;24(3):407–13.
6. Higareda Basilio AE, Ceballos Zuñiga CO, Hernandez Rocha FI, Yaurima Ham SS. Pulmonary spindle cell carcinoma: case report and literature review. Pulm Respir Med Int J. 2019 Mar 12;2(1):1–3.
7. Venissac N, Pop D, Lassalle S, Berthier F, Hofman P, et al. Sarcomatoid lung cancer (spindle/giant cells): An aggressive disease? J Thorac Cardiovasc Surg. 2007 Sep 1;134(3):619–23.
8. Nakajima M, Kasai T, Hashimoto H, Iwata Y, Manabe H. Sarcomatoid carcinoma of the lung: a clinicopathologic study of 37 cases. Cancer. 1999 Aug 15;86(4):608–16.
9. Langer CJ, Gadgeel SM, Borghaei H, Papadimitrakopoulou VA, Patnaik A, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomized, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol. 2016 Nov;17(11):1497–508.
10. Park JS, Lee Y, Han J, Kim HK, Choi YS, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the lung. Oncology. 2011;81(3–4):206–13. 3.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License