IJCRR - 13(13), July, 2021
Pages: 184-189
Date of Publication: 05-Jul-2021
Print Article
Download XML Download PDF
A Cross-Sectional Study on Brain Lesions Diagnosed Through Magnetic Resonance Spectroscopy in Patients from South Kerala
Author: Smitha H, Meena Devi V N, Jacob Vinoo, Sreekanth K S
Category: Healthcare
Abstract:Introduction: A hospital-based study is conducted to find out the frequency, types, and aetiology and gender differences in brain lesions in patients diagnosed through Magnetic Resonance Spectroscopy (MRS) from South Kerala. Objectives: The study aims to assess the socio-demographic characteristics with the increasing incidence of brain lesions in patients attending a tertiary care hospital in South Kerala. Materials and Methods: In this study, there were 81 patients, both males and females, who underwent MRS for the diagnosis of brain lesions and studied for their socio-demographic characteristics which were recorded and compared. Results: The present study revealed that brain lesions were more common in males (57%) as compared to females (43%) (46:35). The frequency of brain lesions was higher in the middle aged group (52%) when compared to the younger age (6%) and old age group (42%). It is found that out of the 81cases, Meningioma is the most common types of brain lesions and also found that the symptoms are well correlating with clinical conditions as indicators for intervention. Conclusion: The analysis of the study indicates the need for special attention of such patients who come with early symptoms suggestive of brain lesions for the correct diagnosis through MRS and for further treatments.
Keywords: Age, Gender, Headache, Meningioma, Magnetic resonance spectroscopy, Vomiting
Full Text:
INTRODUCTION
There is an increasing prevalence of brain lesions in recent years and the underlying diseases associated with lesions are also drastically increasing. In most cases since there are tissue damages involved it is very difficult to treat, however, an early diagnosis may help to lead a quality life with proper treatment and medication.
In the UK, the annual incidence of brain tumour is approximately 0.06-0.01%. In which 72 % of people with a brain tumour are above the age of 50 years.1The prevalence of the previous history varies depending on location, type of tumour and age of the patient.2 After a head injury at any age, vomiting is another common symptom noticed.3 Another risk factor of brain injury is high and low blood pressure. The incidence of the infarct is higher in patients with high blood pressure.4
Brain lesions include brain abscess, tuberculoma, neurocysticercosis, tumours and sarcoidosis.5 The studies revealed that per year the incidence of Central Nervous System (CNS) tumours varies from 10-17 per lakh persons for intracranial and 1-2 per lakh persons for intraspinal tumours.6 With the help of newer advanced techniques like Diffusion-weighted Magnetic Resonance imaging, Perfusion weighted Magnetic Resonance, Magnetic Resonance Spectroscopy etc, Neoplastic lesions can be distinguished from non-neoplastic lesions.7 Magnetic Resonance Spectroscopy (MRS) is a specialized in vivo technique that is used to differentiate the lesions by distinct patterns for the specific disease process to offer quality treatments.8, 9 To our knowledge literature is scarce regarding history like headache, vomiting, nausea, dizziness etc in patients with a brain lesion. The current study was undertaken to investigate the incidence of brain lesions in patients with characteristic risk factors involved including headache, vomiting, dizziness etc to assess the diagnostic significance.
MATERIALS AND METHODS
This is a retrospective study, conducted in the Radiology Department of one of the major tertiary health care centres in South Kerala. All the patients suspected of brain lesions and who underwent MRS for the diagnosis were included in the study from January 2018 to December 2018. The study was approved by the Institutional Ethics Committee. Only patients with proven MRS diagnosis for brain lesion were included as study subjects. In addition to the types of brain lesions, patient’s demographics including age and gender were also taken for analysis and interpretation. Both males and females were included in the study. Patients with implants, aneurysm clips, pacemakers, heart valves and those who are not willing to participate in the study and patients with age below 20 years were excluded from this study.
The ethical clearance number is SGMC-IEC NO: /383/11/2018(F)
The patients were categorised according to the age as patients with 20-40 years, patients with 40-60 years and patients with > 60 years. There were 81 patients, both males and females, who underwent MRS for the diagnosis of brain lesions and studied for their age, gender, types of lesions and history and were recorded to get the distribution and pattern of brain lesions.MRI scans of three different planes- Axial, Coronal and Sagittal were performed by using MRI scans of 1.5 T with sequences like FLAIR T2 weighted imaging and diffusion-weighted imaging (DWI). For analysing the spectra, Spectroscopy-2D Brain software was used. MRS requires radiofrequency (RF) coils and a software package. For the spectrum acquisition, different spatial localization techniques like Single-voxel and Multi-voxel imaging were used. The Single-voxel technique records spectra from one region of the brain at a time. 10 Multi-voxel technique simultaneously recorded spectra from multiple regions.11
RESULTS
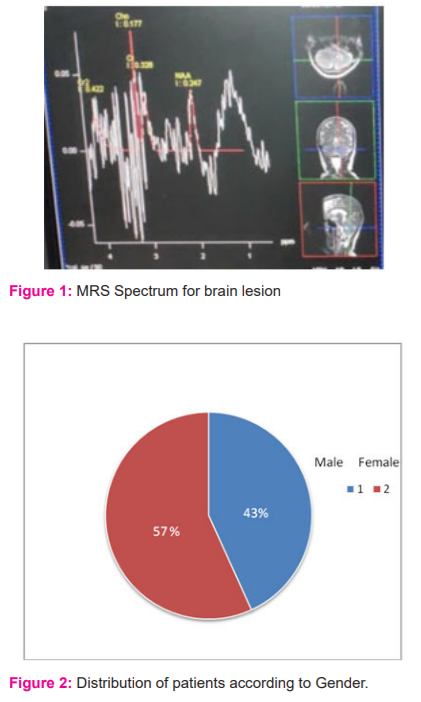
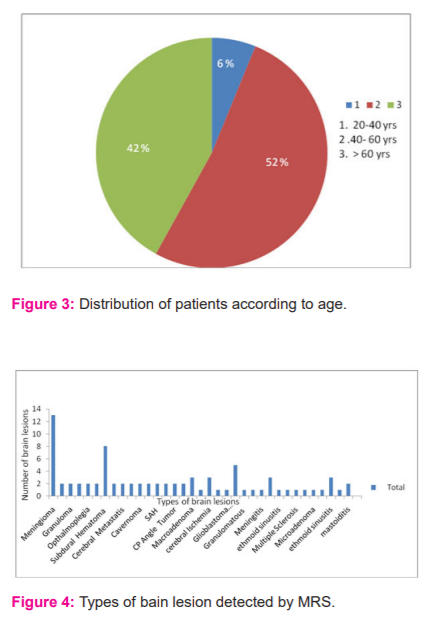
The brain tissue concentrations of metabolites (Figure 1) like N-acetyl aspartate (NAA), choline (Cho), creatine (Cr), lactate (Lac), Myo-Inositol (mI) etc and measured as spectral peaks through MRS. A raised Cho or decreased NAA combined with a rise in Cho/Cr and Cho/NAA ratios indicated a tumour. Additionally, lipid and lactate peaks were observed in infections. The relation between types of lesions and gender are represented in figure 2. From this study it was observed that out of 81 patients analysed for the study, 46 patients (57%) were males and 35 (43%) were females. The present study indicates that brain lesions were more common in males (57%) when compared to females (43%) with a male to female ratio of (46: 35). Figure.3 represents the frequency of brain lesions concerning age. Among these 81 cases, age varied from 20 years to 60 years. It was revealed that the frequency of brain lesions was higher in the middle aged group (52%) when compared to younger age (6%) and old age groups (42%). Patients with age 20-40 years accounted for 5 cases (6%), 40- 60years accounted for 42 cases (52%) and >60 years accounted for 34 cases (42%).
The types of lesion detected by Magnetic Resonance Spectroscopy in these patients are represented in figure 4. It was found that out of the 81 cases, meningioma was the most common types of brain lesions affecting the South Kerala population as diagnosed through MRS. Other types of brain lesions observed were glioma, granuloma, seizure, ophthalmoplegia, cranioplasty, oligodendroglioma, cerebral metastasis, tuberculoma, cavernoma, 6th nerve palsy, subarachnoid haemorrhage (SAH), peripheral vertigo, cerebellopontine angle (CPA) tumour, migraines, macroadenoma, amyotrophic lateral sclerosis, cerebral ischemia, fazeka’s grade II, glioblastoma multiforme, cerebral atrophy, granulomatous, cystic lesion, meningitis, Fazekas's grade I, ethmoid sinusitis, Tolosa hunt syndrome, multiple sclerosis, Rathke's cleft cyst, microadenoma, encephalomalacia, tubercular granuloma, mastoiditis, glomus tympanum.
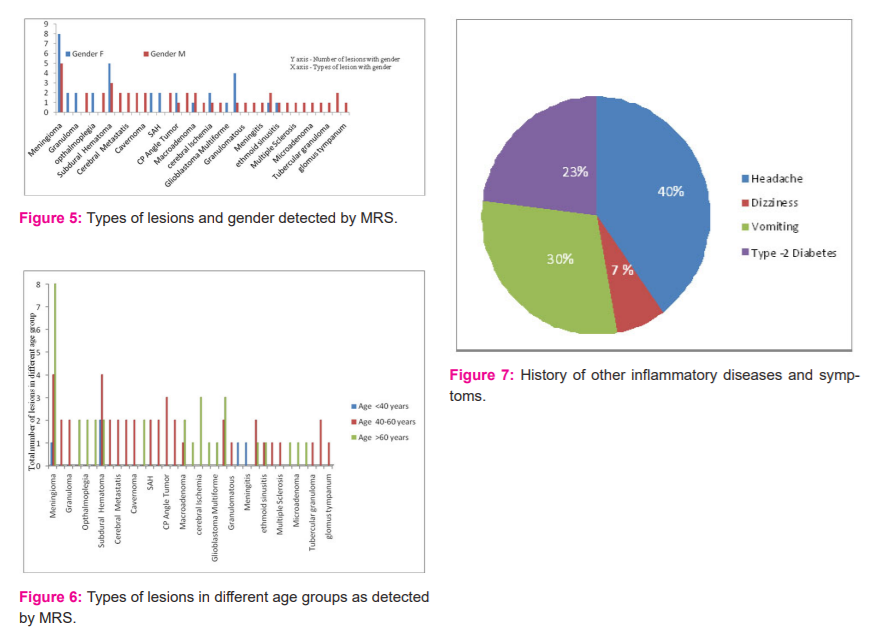
As per the study, it was observed that out of 34 types of brain lesions, meningioma is the most common type of lesion affecting females as compared to males (figure 5). Figure: 6 show the types of lesions in three different age groups of 20-40 years,40-60 years and > 60 years. It was observed that meningioma is more common in people age >60 years.
The history of other inflammatory diseases and symptoms were represented in figure 7. It was found that out of 81 patients, 39 % had a headache, 30 % had vomiting, 23 % had Type-2 diabetes mellitus and 7% had dizziness. Further, it was observed that in most of the brain lesions the blood pressure was high for the subjects. Based on the clinical examination, the main symptom observed was vomiting in patients with meningioma, glioma, seizure, oligodendroglioma, tuberculoma, CP angle tumour, amyotrophic lateral sclerosis, fazeka’s gradeII, meningitis, Tolosa hunt syndrome, Rathke's cleft cyst, encephalomalacia and tubercular granuloma. Similarly, it was also found that patients suffering from lesions like glioma, seizure, cerebral metastasis, tuberculoma, cavernoma, CP angle tumour, migraines, macroadenoma, cerebral ischemia, fazeka’s grade II were also presented with headache. It was noted that the dizziness was there in patients with CP angle tumour, granulomatous and glomus tympanum. It was also observed that there was a history of type -2 Diabetes mellitus for patients affected with meningioma, cerebral metastasis, tuberculoma, nerve palsy, peripheral vertigo, migrainosus, macroadenoma, cysticlesion, tubercular granuloma and mastoiditis. Another history like hemiparesis was found in lesion granuloma.
DISCUSSION
Nowadays clinician takes a keen interest in the management of brain lesions due to their high incidence. In this study, we retrospectively analyzed the data regarding incidence, medical history and the symptoms associated with different types of brain lesions presented in patients who attended a major tertiary health care centre in South Kerala over 12 months. This information may help to predict the need for a specific diagnosis to confirm the lesions as early as possible to get better treatment.
In this study, it was observed that the middle-aged group is more affected with brain lesions unlike in other studies from developed countries. Previous studies indicate that the incidence of brain lesions in developed and developing countries are common in the elderly population.12 In England, about 1.5 % -1.9% of all cancers, Central Nervous System (CNS) tumours are predominant in old age.13 Present study shows that males are more prone to brain lesions as compared to females in South Kerala indicating gender has a major role in disease risk and prognosis. Earlier study it was also found that there is a measurable difference in the prevalence, mortality and progression of cancer in men and women.14 Earlier studies show that there is a higher incidence of CNS tumours in females in the United States compared to England.13 But a study conducted in Asia revealed that brain metastases were more common in males as compared to female.12 Another study also revealed that males are more proponent with seizures compared to females, which were supporting our findings.15
The present study also found that one of the common types of lesions detected is meningioma. Similarly, it was found to be more in females compared to males. A previous study also revealed that meningioma is asymptomatic and was found that it is the more frequent type of lesion observed in people.16 According to World Health Organization (WHO) meningioma are more common in women.17 Similarly in one of the studies it was mentioned that females are more prone to meningioma than male, in the ratio 2:1.18 It was observed that in developed countries the meningioma is more common in children.13 In another study it was reported that women are more susceptible to develop meningioma than men.18 It was also detected that females are prone to low-grade meningioma while males are more susceptible to malignant type.14 In one of the study conducted in the US it was found that of all primary central nervous system tumours, 37% were of meningioma. Also, the incidence increases with twice as common in females as in males.19 In our present study it was also found that the meningioma is more in old age group (›60yrs). Previous studies revealed that there is an increase in the incidence of meningioma with the increase in age.20
This study shows that the lesions like cerebral metastases were presented with headache. In one of the study, it was also found that headache was the presenting symptom in intracranial metastases.21 Present study also shows that for the brain lesions including tumours like meningioma, glioma, tuberculoma, CP angle tumour and other lesions like seizure and cerebral metastasis there was a symptom of vomiting. In this study, it was found that the lesion like glioma, the main history was vomiting and headache. Earlier studies also confirmed that vomiting is a common symptom after a head injury at any age.3
In the present study, it was observed that lesion like subdural hematoma was presented with intracranial bleed. The previous study shows that acute subdural hematoma was a reason for intracranial haemorrhage.22 Present study revealed that nerve palsy was associated with diplopia. Earlier studies revealed that there is a clinical history of uncrossed diplopia associated with eye pain in nerve palsy lesions.23 In this study it was found out that SAH was presented with a history of bleed from the nose and mouth. Studies also found that SAH is associated with ruptured intracranial aneurysms.24 In this study it was observed that peripheral vertigo was presented with a history of nephropathy and retinopathy. From one of the study, it was concluded that the complications of diabetes like retinopathy and neuropathy may affect the vestibular system .25
The current study shows that the lesion including tumours like meningioma, tuberculoma, nerve palsy, peripheral vertigo, migraines, macroadenoma, cystic lesion, tubercular granuloma and mastoiditis were diagnosed with type -2 diabetes mellitus (DM). Earlier studies also reported that DM is a significant risk factor for several types of cancer, including cancer of the breast. In the previous study, it was also found that diabetic individuals had a risk of brain tumours.26 In this study, it was found that individuals with other lesions like cerebral metastasis were also diagnosed with DM. In earlier studies also it was confirmed that DM was a significant predictor in patients treated for brain metastasis.27
Conclusion
Meningioma is the most common types of Brain Lesions which are detected through Magnetic Resonance Spectroscopy (MRS) among the old aged group of patients from South Kerala. It is also found that meningioma is predominant in females. This indicates the need for special attention from the clinicians to take care of female patients in the old aged group who comes with early symptoms suggestive of brain lesions and to impart correct diagnosis through Magnetic Resonance Spectroscopy for time management. This may lead to an improved understanding of the mechanisms of advanced diagnostic modalities, better categorization of symptom constructs, and prospective trials for the management of the symptoms in patients with brain lesions.
Acknowledgement
The authors are greatly thankful to the hospital management of Sree Gokulam Medical College & Research Foundation for their help and support in the patient's study and facility provided. The authors are also thankful to the Department of Physics, Noorul Islam Centre for Higher Education for their technical support for the study.
Conflict of Interest
All authors declared that they have no conflict of interest and no source of funding.
Authors Contribution
Mrs. H Smitha – First author
Is the principal investigator involved in the study. Done in the design, data acquisition, data analysis and manuscript preparation, manuscript editing and literature search.
Dr. VN Meena Devi – Second author
She is involved in coordinating the work and giving valuable suggestions for modifications as the corresponding author.
Dr. Jacob Vinoo
Provided the patients for the study and helped in the interpretation of the report of MRS.
Dr. K S Sreekanth - Fourth author
Contributed to the preparation of the manuscript. Involved in the data analysis especially for the analysis and interpretation of the biochemical changes in MRS.
References:
1.Kernick D P, Ahmed F, Bahra A, Dowson A, Elrington G, Fontebasso M, et.al. Imaging patients with suspected brain tumour: guidance for primary care. Bri J of Gen Pract. 2008 Dec; 58 (557): 880–885. DOI: https://doi.org/10.3399/bjgp08X376203
2.Kirby S, Purdy R A . Headache and brain tumours. Curr Neurol Neurosci Rep . 2007 April; 7(2):110-116.DOI : https://doi.org/10.1007/s11910-007-0005-7
3. Borland ML, Dalziel SR, Phillips N, Dalton S, Lyttle MD, Bressan S ,et al . Vomiting With Head Trauma and Risk of Traumatic Brain Injury. Paedia. 2018 Apr;141(4): 1 -12. doi: 10.1542/peds.2017-3123.
4.Jain V, Choudhary J, Pandit R. Blood Pressure Target in Acute Brain Injury. Indian J Crit Care Med. 2019 Jun;23(Suppl 2): S136-S139. doi:10.5005/jp-journals-10071-23191
5.Sharma V, Prabhash K, Noronha V, Tandon N, Joshi A. A systematic approach to the diagnosis of cystic brain lesions. South Asian J Cancer. 2013 Apr; 2(2):98-101. doi: 10.4103/2278-330X.110509.
6.Acharya S, Azad S, Kishore S, Kumar R, Arora P. Squash Smear Cytology, CNS Lesions – Strengths and Limitations. Nat J Lab Med. 2016 Jul; 5(3): PO01-PO07. DOI: 10.7860/NJLM/2016/18686.2125
7.Garg R, Sinha M.Multiple ring-enhancing lesions of the brain, J Postgraduate Med 2010Oct;56(4):307-316. https://www.jpgmonline.com/text.asp ?2010/56/4/307/70939
8.Salih M, Yousef M, Abukonna A, Elnour A, Elamin A. Evaluation of Brain Lesions Using MagneticResonanceSpectroscopy. J Am Med Res. 2016Sep;18(2):1-6 https://doi.org/10.9734/BJMMR/2016/28984
9.Cecil K M. Proton magnetic resonance spectroscopy technique for the neurologist .Neuroim Clin N Am. 2013 Jan: ; 23 (3) : 381-392 . doi:10.1016/j.nic.2012.10.003
10.Bertholdo D, Watcharakorn A, Castillo M. Brain proton magnetic resonance spectroscopy: introduction and overview. Neuroimaging Clin N Am. 2013 Aug;23(3):359-80. doi: 10.1016/j.nic.2012.10.002.
11.Horská A, Barker PB. Imaging of brain tumours: MR spectroscopy and metabolic imaging. Neuroimaging Clin N Am. 2010 Aug; 20(3):293-310. doi: 10.1016/j.nic.2010.04.003.
12.Saha A, Ghosh SK, Roy C, Choudhury KB, Chakrabarty B, Sarkar R. Demographic and clinical profile of patients with brain metastases: A retrospective study. Asian J Neurosurg. 2013 Jul; 8(3):157-61. doi: 10.4103/1793-5482.121688.
13.Arora RS, Alston RD, Eden TO, Estlin EJ, Moran A, Birch JM. Age-incidence patterns of primary CNS tumours in children, adolescents, and adults in England. Neuro Oncol. 2009; 11(4):403-413. doi:10.1215/15228517-2008-097
14. Sun T, Plutynski A, Ward S, Rubin JB. An integrative view on sex differences in brain tumours. Cell Mol Life Sci. 2015 Sep;72(17):3323-42. doi: 10.1007/s00018-015-1930-2.
15.Rudresh K, Krishna M V, Sebastian K J . Clinical and Aetiological Profile of Ring-enhancing Lesions on CT Brain. Journal, Indian Academy of Clinical Medicine journal.2008 April; 9(2):100-102.
16. Shaikh N, Dixit K, Raizer J. Recent advances in managing/understanding meningioma F1000Res. Clin Cancer Res. 2018 Apr; 490(7): 1-8. DOI: 10.12688/f1000research.13674.1
17.Asgharian B, Chen YJ, Patronas NJ, Peghini PL, Reynolds JC, Vortmeyer A, et. al. Meningiomas may be a component tumour of multiple endocrine neoplasia type 1. Clin Cancer Res. 2004 Feb 1;10(3):869-80. DOI : 10.1158/1078-0432.
18. Shah S, Gonsai R N, Makwana R. Histopathological Study of Meningioma in Civil Hospital, Ahmedabad. Int J Cur Res Rev. 2013 Feb ; 05 (03) 76-82 .
19.Fogh SE, Johnson DR, Barker FG, Brastianos P K, Clarke JL, Kaufmann TJ,et al . Case-BasedReview:meningioma.NeurooncolPract.2016Jun;3(2):120-134.doi: 10.1093/nop/npv063.
20.Wiemels J, Wrensch M, Claus EB. Epidemiology and aetiology of meningioma. J Neurooncol. 2010 Sep; 99(3):307-14. doi: 10.1007/s11060-010-0386-3.
21.Kaul D, Budach V, Graaf L, Gollrad J, Badakhshi H. Outcome of Elderly Patients with Meningioma after Image-Guided Stereotactic Radiotherapy: A Study of 100 Cases. Biomed Res Int. 2015 May 2015: 1-6. doi: 10.1155/2015/868401.
22.Christiaans MH, Kelder JC, Arnoldus EP, Tijssen CC. Prediction of intracranial metastases in cancer patients with headache. Cancer. 2002 Apr 1;94(7):2063-8. doi: 10.1002/cncr.10379.
23.Patel PV, FitzMaurice E, Nandigam RN, Auluck P, Viswanathan A, Goldstein JN, et al. Association of subdural hematoma with increased mortality in lobar intracerebral haemorrhage. Arch Neurol. 2009 Jan;66(1):79-84. doi: 10.1001/archneur.66.1.79.
24 Hussaindeen, J. R., Mani, R., Rakshit, A., Ramasubramanian, S., Vittal Praveen, S. Natural history of idiopathic abducens nerve paresis in a young adult. J Opt. 2016 Feb: 9(4), 264–268. https://doi.org/10.1016/j.optom.2016.02.002
25.Nomani, A. Z., Rajput, H. M., Iqbal, M., Jan, Z., Irshad, M., Badshah, M, et al. Subarachnoid hemorrhage secondary to forceful sneeze. Case Rep Neur Med. 2015 Dec; 1-5. https://doi.org/10.1155/2015/896732.
26..D'Silva LJ, Lin J, Staecker H, Whitney SL, Kluding PM. Impact of Diabetic Complications on Balance and Falls: Contribution of the Vestibular System. Phys Ther. 2016 Mar; 96(3):400-9. https:// doi: 10.2522/ptj.20140604.
27.Tong JJ, Tao H, Hui OT, Jian, C. Diabetes mellitus and risk of brain tumors: A meta-analysis. Expt Therap Med. 2019; 4(5), 877–882. https://doi.org/10.3892/etm.2012.698
28. LeCompte MC, McTyre ER, Strowd RE, Lanier C, Soike MH, Hughes RT, et al. Impact of diabetes mellitus on outcomes in patients with brain metastasis treated with stereotactic radiosurgery. J Radiosurg SBRT. 2018; 5(4):285-291. PMID: 30538889; PMCID: PMC6255719.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License