IJCRR - 13(8), April, 2021
Pages: 22-25
Date of Publication: 25-Apr-2021
Print Article
Download XML Download PDF
Evaluation of Non-resolving Consolidation by Computerized Tomography (CT) Guided Biopsy: An Etiological and Diagnostic Perspective
Author: Imran Nazir Salroo, Javvid Muzamil, Musharaf Bashir, Amir Shafi, Haseeb Mohammad Khandwaw, Abdul Ahad Wani
Category: Healthcare
Abstract:Background: Pulmonary consolidation is a common clinical entity that may arise due to infections or malignancy. Objective: To determine the clinical role, safety, diagnostic accuracy and complications of CT guided lung biopsy in the evalua�tion of non-resolving lung consolidation. Methods: A retrospective review of all CT guided PTNB (percutaneous transthoracic needle biopsy) at a tertiary care hospital was performed from February 2018 to January 2020 for non-resolving consolidations. Radiologic, Histopathologic and Microbio�logical results were obtained and clinical follow up was performed. Results: Over 2 years, twenty-one out of 475 consolidations (4.4%) were subjected to PTNB. The mean age was 64.04 \? 5.12 years. Male: Female ratio was 4:1. The final diagnosis was established in 20 out of 21 (95.23%). Malignancy was detected in 15 out of 21 (71.42%). Tuberculosis was detected in 2/21 (9.52%). Lymphoma was detected in (14.28%). Procedure-related complications were rare and no procedure-related death was noted. Pneumothorax was seen in 2/21 (9.5%) patients. Mild hem�optysis was seen in 3/21 (14.2%) patients. Conclusion: Non-resolving lung consolidation can be safely and effectively evaluated with CT guided percutaneous needle biopsy. The diagnostic yield is high and the procedure is safe.
Keywords: Percutaneous, Transthoracic, Needle biopsy, Consolidation, CT, Non-resolving
Full Text:
Introduction
Pulmonary consolidation is a common clinical entity characterized by signs and symptoms of pneumonia and presence of lung infiltrate on plain chest radiograph in which radiological appearance of pneumonia may include lobar consolidation due to typical bacteria, interstitial infiltrates due to atypical organisms, or cavitation.1 Clinical signs and symptoms in presence of infiltrates on plain radiograph is the gold standard for diagnosis of pneumonia whereas microbiological features are supportive.2 ForaRadiologist, it is not possible to reliably differentiate between bacterial and non-bacterial pneumonia based on radiological appearance alone.3 Nevertheless, a chest radiograph (posterior-anterior view and lateral view) is generally adequate for clinical care of most patients with pneumonia.4 However, there is marked and substantial variation (inter-observer) in the interpretation of chest radiograph in patients of possible pneumonia between different radiologists.5 High-resolution computerized tomography (HRCT) is superior to chest radiograph in detecting lesions and defining anatomical changes.6 Consolidation is considered to be persistent when it fails to resolve by 50% in 2 weeks or completely in 4 weeks.7 Persistent consolidation may be due to inadequately treated infection, atypical infections, malignancy, organizing pneumonia, sarcoidosis, tuberculosis or vasculitis.8 Slow or the incomplete resolution of pneumonia despite treatment is a common clinical problem, estimated to be responsible for approximately 15% of inpatients of pulmonary consolidation and 8% of bronchoscopies.7 Approximately 20% of non-resolving pneumonia are due to noninfectious causes.9 This broad difference creates a clinical situation that frequently demands further testing including bronchoscopy and tissue biopsy.
While no consensus guidelines exist, bronchoscopy, broncho-alveolar lavage (BAL) and transbronchial tissue biopsy are usually preferred methods for evaluation of non-resolving consolidations.10 Chest CT, particularly HRCT is the primary radiographic tool for assessing treatment failure in non-resolving pneumonia. Bronchoscopy, BAL and transbronchial lung biopsy can be used successfully to diagnose the aetiology in approximately90% of patients with non-resolving consolidations.10 Transbronchial or open lung biopsy is nowadays very well included in the diagnostic algorithm of non-resolving pneumonia. In cases where bronchoscopic evaluation is non-diagnostic, additional tissue sampling is included especially in peripheral lesions.11 Traditionally surgical biopsy was preferred in such cases; however, CT guided biopsy is a promising alternative as it is less invasive and is associated with fever complications.10PTNB is a well-established and safe for diagnosis of pulmonary nodules, masses and non-resolving consolidation.10 Role for obtaining tissue for molecular testing of lung cancer continues to grow.12 To the best of our knowledge few studies are reporting diagnostic accuracy and safety of PTNB in pulmonary consolidation. Therefore, we aimed the study and determine the clinical role, safety and diagnostic accuracy of CT guided PTNB for etiological and diagnostic perspective.
Materials and Methods
This double centre retrospective study was conducted from February 2018 to January 2020in SKIMS Medical College, Bemina, Srinagar, J&K, India and Khyber Medical Centre, Srinagar, J&K, India. This study was designed and conducted according to the Standards of Reporting of Diagnostic Accuracy Studies [STARD 2015].13 Complications were categorized following the Society of International Radiology Clinical Practice Guidelines.14Written consent was taken from each patient before taking the biopsy. All biopsies were performed by an experienced Radiologist under CT guidance using a 16 slice-Multi Detector CT scanner (MDCT). Whenever possible the densest part of consolidation was targeted rather than an area of ground glass. Fine needle aspirate obtained was submitted to a histopathologist for interpretation. Microbiology of the aspirate was also done to rule out pneumonia, tuberculosis, fungal infections, vasculitis and malignancy.
The sensitivity and specificity of PTNB for infections were calculated. A positive result was considered to be true positive when there was a specific infection or organism detected by PTNB and the patient developed a response after treatment. Those who had a positive PTNB result but were not on therapy had no clinical signs of infection and showed a progressive decline of lesions on follow up CT was taken as false positives. Malignancy, suspected malignancy, nonspecific benign or non-diagnostic lesions were considered to be negative results. True negatives were defined as those who had a clinical diagnosis of non-infectious disease. PTNB result was considered to be falsely negative when there was evidence of infections.
To ascertain risk factors for diagnostic failure of PTNB, patients were categorized into two groups. success-group and failure-group. The success group included truly diagnosed cases whereas the failure group included non-diagnostic, nonspecific benign and falsely diagnosed cases.
Statistical Analysis
All statistical testing was performed using Stata software (version14, StataCorp LLC, Texas, USA). A P-value of 0.05% or less was considered significant.
Results
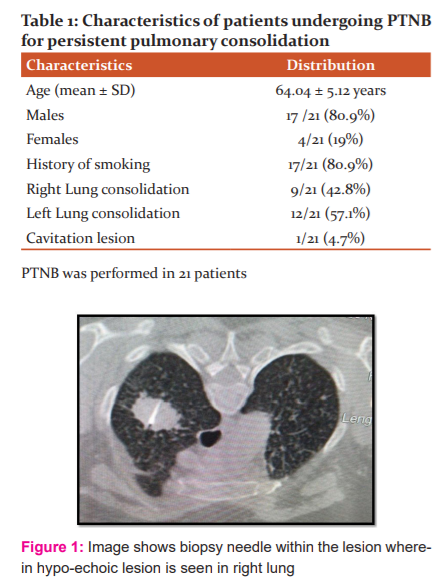
Over 2 years 475 patients were diagnosed as having consolidation. Out of 475 consolidations, only 21 failed to resolve (4.45%). These 21 patients were subjected to PTNB for confirmation of diagnosis [Figure 1]. The majority of patients were males who had a history of smoking 17/21. The mean age of these patients was 64.04 ± 5.12 years. The male-female ratio was approximately 4:1. The consolidation involved the right lung in 9/21(42.85%), left lung in 12/21(57.15%). only 1/21 patients had a cavitation lesion [Table 1].
Out of 21 patients, PTNB accurately established diagnosis in 20/21 (95.23%) patients. Malignancy was detected in 15/21 patients (71.42%). Tuberculosis was found in 2/21 patients (9.52%). Lymphoma was found in 3/21 patients (14.28%). Biopsy was inconclusive in 1/21 (4.76%) patient of non-resolving consolidation. 3/21 (14.28%) patients had metastasis lung with primaries in kidney, uterus and ovary respectively [Figure 2].
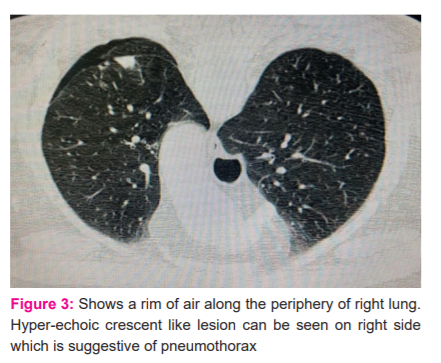
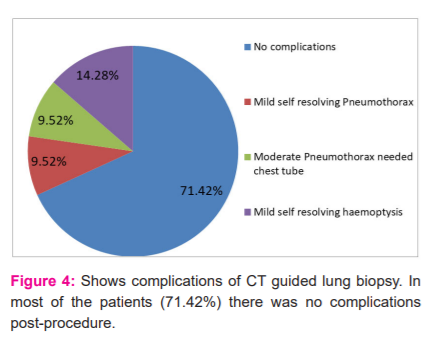
No death or major complication was resulting from PTNB. There were no complications in15/21 (71.42%) patients. Minor complications occurred in 5/21 (23.8%). Pneumothorax [Figure 3] was seen in 2/21 (9.52%) patients and mild self-limited hemoptysis in 3/21 (14.2%) patients. The chest tube was needed in 2/21 (9.52%) patients with pneumothorax and they were discharged after two days [Figure 4]. All other patients were discharged after 4 hours. The pain was minimal in all patients as none of them required any form of analgesic.
Discussion
In this study, the diagnostic yield of PTNB in non-resolving consolidation was high 97 %. Diagnostic failure was found in only 1 out of 21 patients whose biopsy came inconclusive. This study did not observe greater diagnostic failure or complications. It was found that CT guided PTNB provided a definite diagnosis in most of the cases, both malignant and infectious. Kirantawat et al.10 found that CT-guided PTNB gave conclusive diagnoses in all cases of consolidation, both in cases of malignancy and infection, with inconclusive bronchoscopic results even if antibiotics had been started before taking a biopsy. In another study by Ozun C et al.15 in which they analyzed 442 patients who underwent CT guided lung biopsy, they found that the diagnostic accuracy, sensitivity and specificity were 97.6%, 97.3%, and 100% respectively. They concluded that CT guided biopsy is a safe and reliable technique with high diagnostic accuracy. Similar findings were observed in our study. Our findings were much higher than reported earlier by Hur et al.16 who found that CT guided aspiration has sensitivity, specificity and accuracy of 84.100 and 91% respectively in patients of non-resolving consolidation after indeterminate transbronchial biopsy.
In this study, immune-histochemistry was also done in 16 /23 samples. With rapid advances in targeted cancer therapies, the role of PTNB for molecular testing of non-small cell carcinoma continuous to increase.10 Several studies have found that PTNB provides sufficient tissue for molecular testing of non-small cell lung carcinoma.10 Our study confirmed that molecular testing can be safely performed when lung carcinoma presents as consolidation. We found that PTNB is a safe technique to take the sample from consolidations. Previous studies of PTNB of the pulmonary lesion have reported 17 to 37% incidence of pneumothorax and 1 to 14% incidence of chest tube replacement.17 The incidence of chest tube insertion in this study was 2/21 (9.5%).15 Mild hemoptysis was seen in 3/21 (14.28%) which is close to the reported incidence0.2-8.4%.18
This study has a few limitations. The retrospective nature of the study may have introduced a selection bias. Another limitation is the small number of cases included. Our results are based on experience at two academic medical centres and may not be widely applicable to centres that are not experienced enough in PTNB.
Conclusion
It may be concluded that pulmonary lesion can be safely evaluated by CT-guided percutaneous needle biopsy. PTNB may be used for tissue sampling from pulmonary consolidations and accurate diagnosis of malignancy. Our results support the important diagnostic role of PTNB in the evaluation of persistent pulmonary consolidation.
Acknowledgement: We acknowledge the great help received from the researchers whose articles are cited and included in references to this manuscript.
Author contribution
Imran Nazir Salroo: Data collection, Manuscript preparation.
Javid Muzzamil: Data collection.
Musharaf Bashir: Manuscript preparation
Amir Shafi: Data analysis
Haseeb Mohammad Khandwaw: Data analysis
Abdul AhadWani: Manuscript revision, Data analysis.
Funding: None
Conflict of interest: None

References:
-
Walker CM, Abbott GF, Greene RE. Imaging pulmonary infections: Classic signs and patterns. Am J Roentgenol 2014; 202 (3): 479-92.
-
Stadler JAM, Andronikou S, Zar HJ. Lung ultrasound for the diagnosis of community acquired pneumoniain children. Pediatr Radiol 2017;47(11);412-19.
-
Beigelman-Aubry C, Godet C, Caumes E. Lung infections: the radiologist’s perspective. Diagn Interv Imaging 2012; 93(6):431-40.
-
Wootton D, Feldman C. The diagnosis of pneumonia requires a chest radiograph (x-ray)- yes, no or sometimes? Pneumonia 2014;5:1-7.
-
Neuman MI, Lee EY, Bixby S. Reliability of CXR for pneumonia. J Hosp Med 2012; 4: 294-98.
-
Kang M, Deoghuria D, Varma S. Role of HRCT in detection and characterization of pulmonary abnormalities in patients with febrile neutropenia. Lung India 2013;30(2):124-30.
-
Chaudhary AD, Mukherjee S, Nandi S, BhuniyaS, Tapadar SR, Saha M. A study on non-resolving pneumonia with special reference to the role of fibreoptic bronchoscopy. Lung India 2013; 30(1): 27-32.
-
Bajaj SK, Tombach B. Respiratory infections in immunocompromised patients: Lung findings using chest computed tomography. Radiol Infect Dis 2017; 4: 29-37.
-
Palkar AV, Rapose A. Non-resolving pneumonia. BMJ Case Rep 2012; bcr2012006861.
-
Kiranantawat N, McDermott S, Fintelmann FJ. The clinical role, safety and diagnostic accuracy of percutaneous transthoracic needle biopsy in the evaluation of pulmonary consolidation. Respir Res 2019; 20 (23):145-48
-
Lentz RJ, Argento AC, Colby TV, Rickman OB, Maldonado F. Transbronchial cryobiopsy for diffuse parenchymal lung disease: a state-of-the-art review of procedural techniques, current evidence, and future challenges. J Thorac Dis 2017;9(7): 2186-203.
-
Lim C, Sekhon HS, CutzJC, Hwang DM. Improving molecular testing and personalized medicine in non-small-cell lung cancer in Ontario. Curr Oncol 2017;24(2):103-10.
-
Cohen JF, Korevaar DA, Altman DG. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open 2016;6:e012799.
-
Cardella JF, Kundu S, Miller DL, Millward SF, Sacks D. Society of Interventional Radiology Clinical Practise Guidelines. J Vasc Interv Radiol 2009;20(7):189-91.
-
Uzun C, Akkaya Z, Atman ED. Diagnostic accuracy and safety of CT-guided fine-needle aspiration biopsy of pulmonary lesions with non-coaxial technique: a single centre experience with 442 biopsies. Diagn Interv Radiol 2017;23(2):137-43.
-
Hur J, Lee HJ, Byun MK. Computed tomographic fluoroscopy-guided needle aspiration biopsy as a second biopsy technique after indeterminate transbronchial biopsy results for pulmonary lesions: comparison with second transbronchial biopsy. J Comput Assisst Tomogr 2010;34(2):290-95.
-
Bossuyt PM, Reitsma JB, Bruns DE. STARD 2015; an updated list of essential items for reporting diagnostic accuracy studies. Radiology 2015;351: h5527.
-
Tai R, Dunne RM, Trotman-Dickenson B, Jacobson F. Frequency and severity of pulmonary haemorrhage in patients undergoing percutaneous CT-guided transthoracic lung biopsy: singleinstitution experience of 1175 cases. Radiology 2016;279(1):287-96.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License