IJCRR - 13(6), March, 2021
Pages: 135-137
Date of Publication: 20-Mar-2021
Print Article
Download XML Download PDF
Thalassemia in Children: A Case Report
Author: Laltanpuii, Maurya A
Category: Healthcare
Abstract:Introduction: Thalassemia which is also called Cooley's anaemia or Mediterranean anaemia is a group of hereditary hemolytic anaemia characterized by a reduction in the synthesis of haemoglobin. The word 'thalassemia' is derived from the Greek word 'Thalassa' which means the great sea. Clinical observations: Abdominal pain, fever (Temperature - 101?F), Anemia (Hb \? 6.4gm%). Diagnostic evaluation: Hb% \? 6.4gm%, Total RBC count \? 2.3 millions/cu.mm, RDW \? 18.2%, HCT \? 20.2%, Total WBC count \? 3200/cu.mm, Monocytes \? 02%, Granulocytes \? 20%, Lymphocytes \? 77%, AST(SGOT) \? 112 U/L. Peripheral Smear: RBC \? mild hypochromic with mild cystosis which show few microcytic and mildly hypochromic. Platelets \? Reduced on smear, APC \? 62,000 cells. Ultrasonography: Splenomegaly. Therapeutic interventions: Blood transfusion, Inj. Cefotaxime 750mg IV x BD, Syr. Azee 4ml x OD, Tab. Folic Acid 5mg x OD, Tab. Udiliv 150mg x BD, Cap. Hydra 500mg x OD, Tab. Prednisolone 10mg x BD. Outcome: After treatment, the child show improvement. His fever and abdominal pain were relieved and his Hb% increased from 6.4gm% to 11gm% after blood transfusion. Conclusion: My patient was admitted to Pediatric Ward No \? 14, AVBRH with a known case of Thalassemia and he had a com�plaint of fever and abdominal pain. After getting appropriate treatment his condition was improved.
Keywords: Thalassemia, Cooley’s anaemia, Mediterranean anaemia, Hereditary, Hepatosplenomegaly
Full Text:
Introduction
Thalassemia produces hypochromic microcytic anaemia due to defective haemoglobin of RBCs, hemolysis and ineffective erythropoiesis. It can be considered as hemolytic and hypo - proliferative anaemia related to abnormal haemoglobin. It was first noticed in patients, originating from the littoral countries of the Mediterranean Sea. At present, the disease has been found in several countries all over the world. The prevalence of the disease in India is high among Gujaratis, Sindhis and Punjabis. Millions of people are found to be carriers of the thalassemia gene and every year thousands of thalassemic children are born in our country.1
Progressive pallor, anaemia, fatigue or weakness, jaundice, hepatosplenomegaly, recurrent respiratory infection, failure to thrive, facial bone deformities are common symptoms of thalassemia.2 Blood examination, Bone marrow study, Osmotic fragility test, radiological screening are common investigations done in thalassemia.1 Mild thalassemia might not be needed to be treated but severe thalassemia required regular blood transfusions along with symptomatic treatment.2
Thalassemia is classified into three main types, the classification depends on the number of gene mutation and the part of haemoglobin molecules which are affected either alpha or beta.3 The different types are Thalassemia major – Here thalassemia genes (beta) are inherited from both the parents and it is associated with the homozygous state. Synthesis of the beta chain is markedly reduced. Thalassemia intermedia: It is chronic hemolytic anaemia caused by alpha or beta chain synthesis. It is also a homozygous form. Thalassemia minor: It is a mild form of illness and produced by heterozygosity of either alpha or beta chain.1
Management of thalassemia is mostly done by Repeated blood transfusion, iron chelation therapy, splenectomy, folic acid supplementation, bone marrow transplantation, gene therapy and gene mutation, supportive management.1
Patient Identification:
A male child of 8 years from Shirajgamwas admitted to pediatric ward no. 14, AVBRH on 23rd January 2020 with a known case of Thalassemia major. He was 25 kg and his height was 126 cm on admission.
Present medical history:
A male child of 8 years old was brought to AVBRH on 23rd January 2020 by his parents with a complaint of abdominal pain (left hypochondriac region) and fever and he was admitted to Pediatric ward no 14. He is a known case of Thalassemia Major and his Hemoglobin level at the time of admission was 6.4gm%. The child was weak and not cooperative on admission.
Past medical history:
My patient was diagnosed to have thalassemia at the age of 8 months when he was admitted to the hospital due to fever. From that time onwards, he was admitted to the hospital from time to time for blood transfusion.
Family history:
There are four members of the family. My patient was diagnosed to have a Thalassemia major and his parents were the carrier of thalassemia. The type of marriage of the parents is non – consanguineous marriage. All other members of the family were not having complaints about their health except for my patient who was being admitted to the hospital.
Past interventions and outcome:
My patient got diagnosed with thalassemia when he was 8 months old, from that time onwards he was admitted to hospital from time to time for treatment of the disease mostly blood transfusion. It was found effective as the patient does not develop complications till then.
Clinical findings:
Abdominal pain, fever (Temperature - 101?F), Anemia (Hb – 6.4gm%)
Aetiology:
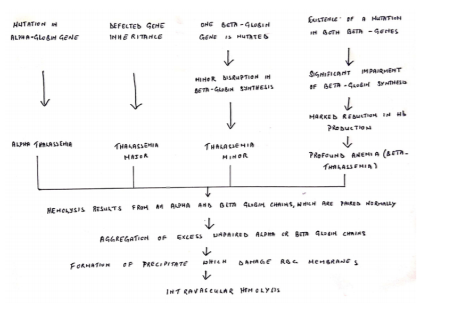
Thalassemia occurs when there is a mutation or any abnormality in any one of the genes which take part in producing haemoglobin. When there is a genetic abnormality, it can be pass – on from parents to children. When only one of the parents is a carrier, there is the chance of developing a mild form of thalassemia that is thalassemia minor where symptoms might not be seen but the person will be a carrier. When both the parents are the carrier, there is a great chance of developing a severe form of thalassemias like thalassemia major or thalassemia intermedia.4
Pathophysiology
Physical examination
There was not many abnormalities found in head to toe examination, the child is lean and thin. He is weak and not so cooperative. Though it was found that the child is having splenomegaly from ultrasonography, it is not palpable.
Diagnostic assessment
Pathology:
HB% – 6.4gm%, Total RBC count – 2.3 millions/cu.mm, RDW – 18.2%, HCT – 20.2%, Total WBC count – 3200/cu.mm, Monocytes – 02%, Granulocytes – 20%, Lymphocytes – 77%.
Biochemistry:
AST(SGOT) – 112 U/L.
Peripheral Smear: RBC – mild hypochromic with mild cystosis which show few microcytic. Platelets – Reduced on smear, APC – 62,000 cells.
Ultrasonography: Splenomegaly.
Management
Medical management:
Blood transfusion, Inj. Cefotaxime 750mg IV x BD, Syr. Azee 4ml x OD, Tab. Folic Acid 5mg x OD, Tab. Udiliv 150mg x BD, Cap. Hydra 500mg x OD, Tab. Prednisolone 10mg x BD
Nursing Management:
My patient’s Hb% was 6.4gm% on admission and doctors prescribed blood transfusion, I have started blood transfusion according to prescription and during a blood transfusion, I have assessed the condition of the patient, monitor vital signs and there was no complication due to blood transfusion. The child also complained of abdominal pain and fever, for abdominal pain I gave a comfortable position according to the child’s preference and for fever I gave cold sponging. I have provided medications according to prescriptions of the physicians and evaluate for therapeutic response. Give health teaching to both the child and parents related to disease condition and treatments.
Discussion
A male child of 8 years old from Shirajgam was admitted to pediatric ward no 14, AVBRH on 23rd January 2020 with a complaint of abdominal pain, fever and Hb% less than the normal limit. He is a known case of thalassemia major which was diagnosed when he was 8 months old. As soon as he was admitted to the hospital investigations were done and appropriate treatment was started. After getting treatment, he shows great improvement and the treatment was still going on till my last date of care. Among inheritable diseases, thalassemia is one of the most common diseases in the world. It needs long – term treatment so it is better to take preventive measures.5 Mostly, screening for carrier and counselling are done voluntarily.
A study was done on, “A clinical – epidemiological study of thalassemia cases in India”. It was done to assess the clinical presentation and management practices in thalassemia. For the study, patients case sheets were collected between 2005 – 2014 which is 10 years. These case sheets were being examined and recorded in a specially made proforma for the study. The result from the study was – a total of 183 cases are recorded and among those, 179 (97.8%) were beta-thalassemia major, 3 (1.6%) were beta-thalassemia intermedia and 1 (0.6%) was beta-thalassemia minor. Most of the case was diagnosed at age of 1 year, and one-fourth of the case was diagnosed in the first 6 months. Fever present in 34 patients (18.6%), pallor found in 179 patients (97.8%), hepatomegaly seen in 172 patients (94%) and bone deformity found in 13 patients (7.1%). One-third of the under-five patients were found to be underweight and more than half of the patients were found to be stunted. The mean post-transfusion value of haemoglobin after 1 year of transfusion among cases was 10±1.6g%, 51 patients (27.9%) were given desferrioxamine as iron chelation therapy and the mean age of starting this therapy was 11.1±8.2 years. In 4 cases of beta-thalassemia, major splenectomy was done at a mean age of 10.7±4.8 years. On the treatment of thalassemia with desferrioxamine lenticular opacity was found in greater proportion. The study concluded that among thalassemic patient different kinds of complications were found so it is important to involve different specialization in the care of thalassemia patient to control the problems.6
Conclusion
Thalassemia is one of the most common cases found among children, it is very important to diagnose in the early stage and start treatment so that the child will not develop complications. It is also very important to take preventive measures like antenatal screening and genetic counselling. My patient shows great improvement after getting the treatment and the treatment was still going on till my last date of care.
Ethical approval: Not applicable
Patient Inform consent: Informed consent has been taken from the patient’s parents.
Conflict of Interest: The author declares that there are no conflicts of interest.
Funding: Not applicable
References:
-
Parul D. Pediatric Nursing. 4th Edition. New Delhi: Jaypee Brothers Medical Publishers; 2018. Page 300-303
-
Thalassemia. Mayo Clinic. Available from https://www.mayoclinic.org/diseases-conditions/thalassemia/symptoms-causes/syc-20354995
-
Shilpa A. Everything you need to know about thalassemia. August, 2019. Healthline. Available from https://www.healthline.com/health/thalassemia
-
Yolanda S. Thalassemia Pathophysiology. News Medical Life Sciences. Available from https://www.news-medical.net/health/thalassemia-pathophysiology.aspx
-
Antonio C, Kan YW. The Prevention of Thalassemia. Perspect Med 2013;3(2):a011775.
-
Nitin J, Pai S, Sengupta S. A clinico – epidemiological study of thalassemia cases in India. J Nat Sci Biol Med 2018;9(2):236-241.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License