IJCRR - 13(5), March, 2021
Pages: 179-182
Date of Publication: 03-Mar-2021
Print Article
Download XML Download PDF
Efficacy of BISAP & APACHAE2 Scoring System in Early Prediction of Severity in Acute Pancreatitis: A Prospective Study
Author: Rahul Ranjan, Tushar Parmeshwar, Sharaddendu Bali, Akhilesh Yadav
Category: Healthcare
Abstract:Introduction: Different methods, including the Ranson criteria, Acute Physiology & Chronic Health Assessment (APACHE) II, Computed Tomography (CT) Severity Index (CTSI), Glasgow & Imrie scoring systems, have been used over the years to predict the severity and outcome of acute pancreatitis. Each has benefits & drawbacks & none of them is currently accepted as a standard criterion. An early, easy, clear, reliable & reproducible definition of disease severity could promise an ideal scoring system. Objective: To evaluate the efficacy of BISAP & APACHAE2 Scoring System in early prediction of severity in Acute Pancreatitis. Methods: A total of 50 consecutive cases fulfilling the eligibility criteria were taken for study after informed consent. Results: The BISAP score's sensitivity & specificity was 75% & 76.2%, with a positive & negative predictive value of 37.5% & 94.1%. The overall accuracy of the BISAP score for extreme acute pancreatitis prediction was 76%. The APACHE II score's sensitivity & specificity was 62.5% & 85.7%, with a positive & negative predictive value of 45.5% & 92.3%. In predicting extreme acute pancreatitis, the overall accuracy of the BISAP score is 82%. Conclusion: Current research shows that the scoring systems, i.e., all In the prediction of serious acute pancreatitis, APACHE II & BISAP were comparable & fine (SAP). The BISAP score was outperformed in precision, but with a good sensitivity & negative predictive value compared to the APACHE II score.
Keywords: Acute pancreatitis, BISAP score, APACHE II score, SAP and abdominal catastrophes.
Full Text:
Introduction
In the diagnosis of acute pancreatitis, the clinical & biochemical parameters form the main factor. However the history and clinical presentation may be deceptive and the biochemical parameters (serum amylase values in particular) may be normal, particularly if the test is performed a few days after the initial attack.1 Conventional radiograph have been used to exclude other abdominal catastrophes and help the clinical presumption of acute pancreatitis. In patients suspected of having acute pancreatitis, radiographic studies are of minimal use in both promoting and excluding their diagnosis.2,3 The abdomen's supine, lateral decubitus and erect films help to exclude other diagnoses, such as a perforated viscus. Nonspecific findings in patients with acute pancreatitis, including adynamic ileus or sentinel loop, are found on radiographs.4 Moreover in patients with chronic pancreatitis, pancreatic calcifications may be observed and peripancreatic gas is seen uncommonly in patients with pancreatic abscess. Such exams are very insensitive & unspecific. In serious pancreatitis, mortality can range from 1% to up to 26% in acute pancreatitis. A significant step in improving the outcome is to classify patients at risk for mortality early in the course of acute pancreatitis. Acute pancreatitis treatment is also a problem that the clinician faces.5,6 Yet some guiding principles have evolved over the years, which have also been borne out by the present research. In mild cases, conservative steps such as fasting & vigorous intravenous fluid rehydration are often successfully treated, and extreme cases may require admission to the intensive care unit or even surgery to cope with complications of the disease process.7A very important technique is to be able to predict the prognosis of a patient with acute pancreatitis at admission, given that this would enable them to practice patient management standardization guidelines, such as the use of antibiotics, computed tomography scan timings, the use of Endoscopic retrograde cholangiopancreatography (ERCP) and operative intervention. This will translate into enhanced performance in turn.8
Materials and Methods
At the Department of Surgery of a tertiary healthcare facility, the latest research was performed on diagnosed cases of Acute Pancreatitis coming to our hospital. This was a prospective, retrospective clinical study conducted over a two-year duration after informed consent on a total of 50 consecutive cases meeting the eligibility requirements for the study.
Inclusion/Exclusion Criteria
All adults of both sexes (>18 years). Acute pancreatitis cases with elevated serum lipase/amylase levels & confirmed by USG/CT scan. Gut-perforated pancreatitis and pregnancy pancreatitis patients were excluded.
Procedure
Valid informed consent for inclusion in the study was obtained from patients or associated patients. Medical, laboratory and radiological data were obtained within 24 hours of presentation from each patient diagnosed with acute pancreatitis. Using the data collected, BISAP & APACHE II SCORE was determined for each patient. During their hospital admission, these patients were then followed and reviewed for the development of complications, organ failure, death or before the patient was released. The BISAP & APACHE II score of all patients was then compared with their outcome and statistically evaluated as prognostic indicators of acute pancreatitis for the assessment of these scores.
Results
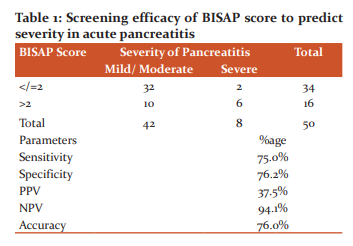
Sensitivity & specificity of BISAP score was 75% & 76.2% with positive & negative predictive value being 37.5% & 94.1% respectively. The overall accuracy of the BISAP score in the prediction of severe acute pancreatitis was 76% (Table 1).
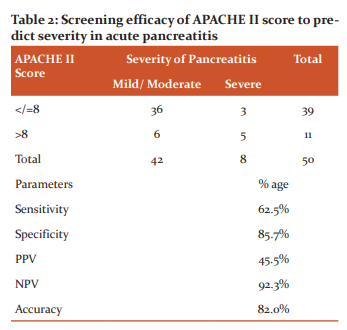
Sensitivity & specificity of APACHE II score was 62.5% & 85.7% with positive & negative predictive value being 45.5% & 92.3% respectively. The overall accuracy of the BISAP score in prediction of severe acute pancreatitis is 82% (Table 2).
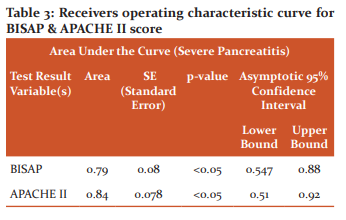
Screening efficacy of BISAP & APACHE II scores in predicting severe acute pancreatitis cases was computed by Receivers operating characteristic curve (Table 3). Screening efficacy as measured by area under the curve was slightly more for APACHE II than BISAP (AUC – 0.84 & 0.79; p<0.05 for both).
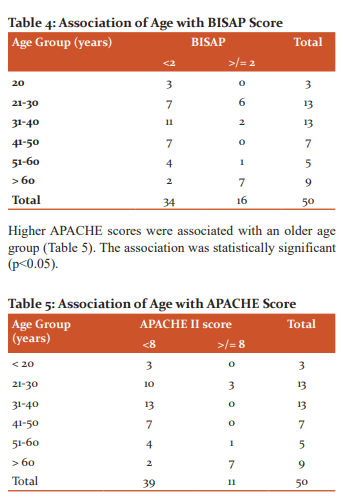
Higher BISAP scores were associated with an older age group. The association was statistically significant (p<0.05). Few of the cases where complications were seen in BISAP score of <2, can thus be attributed to higher age among such cases (Table 4).
Discussion
Traditionally used severity indices such as the parameters of APACHE &Ranson have not been clinically useful as they are cumbersome, require large quantities of clinical & laboratory data over time to be obtained and do not have reasonable positive & negative predictive value for extreme acute pancreatitis. Besides, these ratings are used after 48 hours of entry. BISAP is a basic bedside method that can be used within the first 24 hours of admission and can identify complications for patients at risk, requiring close monitoring and more intensive therapy. The present hospital-based screening test study was thus conducted to evaluate the efficacy of BISAP & APACHAE2 Scoring System in early prediction of severity in Acute Pancreatitis cases. A total of 50 consecutive cases fulfilling the eligibility criteria were taken for study after informed consent. The clinical, laboratory & radiological data were collected from each patient diagnosed as acute pancreatitis within 24 hours of presentation. BISAP & APACHE II SCORE was calculated for each patient using the data obtained. These patients were then followed & reviewed in their course of admission in hospital for development of complications, organ failure, and mortality or till the patient was discharged. BISAP & APACHE II score of all patients were then correlated with their outcome & it was then analysed statistically for the evaluation of these scores as prognostic markers of severe acute pancreatitis (SAP).
Sensitivity & specificity of BISAP score was 75% & 76.2% with positive & negative predictive value being 37.5% & 94.1% respectively. The overall accuracy of the BISAP score in the prediction of severe acute pancreatitis was 76%. Sensitivity & specificity of APACHE II score was 62.5% & 85.7% with positive & negative predictive value being 45.5% & 92.3% respectively. The overall accuracy of the BISAP score in the prediction of severe acute pancreatitis is 82%. The sensitivity of BISAP in our study (75%) is higher than Papachristou et al9 study (37.5%) &Macherla R et al10 (50%); comparable to Cho JH et al11 (62%) & Park JY et al12 (71%) & lower than observed by Senapati D et al13 (92%) & Yadav J et al14 (97.6%). The specificity of BISAP in our study (76.2%) is comparable to Cho JH et al (72%), Senapati D et al (76%) & Park JY et al (85%) while it was lower than observed by Papachristou et al study (92%). The sensitivity of APACHE II in our study (62.5%) is comparable to LarvinM et al15 (65%), Morappanavar16 (70%), Papachristou et al (70%), Macherla R et al (70%) & Park JY et al (71%) studies while it was lower than that of Cho JH et al (81%) & Zhang J et al (85%) studies. The specificity of APACHE II in our study (85.7%) is higher than Macherla R et al (70%), Papachristou et al (70.3%), Cho JH et al (66%), Zhang J et al17 (63%) &Morappanavar (73.9%); while it was comparable to Park JY et al (85%) &Larvin et al (86%).
Screening efficacy of BISAP & APACHE II scores in predicting severe acute pancreatitis cases was computed by Receivers operating characteristic curve. Screening efficacy as measured by area under the curve was slightly more for APACHE II than BISAP (AUC – 0.84 & 0.79; p<0.05 for both). Thus, the present study showed that both APACHE II & BISAP were comparable & good in the prediction of severe acute pancreatitis (SAP). Compared with the APACHE II score, the BISAP score was outperformed in specificity, but have a good sensitivity & negative predictive value. We thus recommend the use of BISAP score in all cases of pancreatitis especially in resource-limited settings as it is a simple bedside tool which can be applied within first 24 hours of admission & can predict patients at risk of development of severe acute pancreatitis.
Conclusion
Identification of patients at risk for mortality early in the course of acute pancreatitis is an important step in improving outcome. The present study shows that both the scoring systems i.e. APACHE II & BISAP were comparable & good in the prediction of severe acute pancreatitis (SAP). Compared with the APACHE II score, the BISAP score was outperformed in specificity, but having a good sensitivity & negative predictive value. We thus recommend the use of BISAP score in all cases of pancreatitis especially in resource-limited settings, as it is a simple bedside tool which can be applied within first 24 hours of admission & can predict patients at risk of development of SAP, who require careful monitoring & more aggressive treatment.
Acknowledgement
The author acknowledges the immense help received from the scholars whose articles are cited and included in references to this manuscript. The author is also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Source of Funding: Nil
Conflict Of Interest: Nil
References:
-
Wang R, Wu H, Tang CW, Chen XZ. Etiology, clinical features and management of acute recurrent pancreatitis. J Dig Dis 2014;15(10):570-577.
-
Ranson J,Rifkind KM, Roses DF, Fink SD, Eng K, Spencer FC.Prognostic signs and the role of operative management in acute pancreatitis. Surg GynecolObstet 1974;139(1):69-81.
-
Knaus W, Draper EA, Wagner DP, Zimmerman JE.APACHE II: a severity of disease classification system. Crit Care Med 1985 Oct; 13(10):818-29.
-
Balthazar E, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: the value of CT in establishing prognosis. Radiology 1990 Feb; 174(2):331-6.
-
Bota S, Sporea I, Sirli R, Popescu A, Strain M, Focsa M, et al. Predictive factors for severe evolution in acute pancreatitis and a new score for predicting a severe outcome. Ann Gastroenterol 2013;26(2):156-162.
-
Khanna AK, Meher S, Prakash S, Tiwary SK, Singh U, Srivastava A, et al. Comparison of Ranson, Glasgow, MOSS, SIRS, BISAP, APACHE-II, CTSI Scores, IL-6, CRP, and procalcitonin in predicting severity, organ failure, pancreatic necrosis, and mortality in acute pancreatitis. HPB Surg 2013;2013:367581.
-
Wu B, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut 2008;57(12):1698–1703.
-
Fitz R. Acute pancreatitis: a consideration of pancreatic haemorrhage, hemorrhagic, suppurative, and gangrenous pancreatitis, and of disseminated fat-necrosis. Boston MedSurg J 1889;120(8):181-187.
-
Papachristou G, Papachristou DJ, Avula H, Slivka A, Whitcomb DC. Obesity increases the severity of acute pancreatitis: performance of APACHE-O score and correlation with the inflammatory response. Pancreatology 2006; 6:279-285.
-
Papachristou GI, Muddana V, Yadav D, O'Connell M, Sanders MK, Slivka A, et al. Comparison of BISAP, Ranson's, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis. Am J Gastroenterol 2010;105(2):435-441.
-
Cho JH, Kim TN, Chung HH, Kim KH. Comparison of scoring systems in predicting the severity of acute pancreatitis. World J Gastroenterol2015;21(8):2387.
-
Park J, Jeon TJ, Ha TH, Hwang JT, Sinn DH, Oh TH, et al. Bedside index for severity in acute pancreatitis: comparison with other scoring systems in predicting severity and organ failure. Hepatobiliary Pancreat Dis Int 2013;12(6):645-650.
-
Senapati D, Debata PK, Jenasamant SS, Nayak AK, Gowda M, Swain NN. A prospective study of the Bedside Index for Severity in Acute Pancreatitis (BISAP) score in acute pancreatitis: an Indian perspective. Pancreatology 2014;14(5):335-339.
-
Yadav J, Yadav SK, Kumar S, Baxla RG, Sinha DK, Bodra P. Predicting morbidity and mortality in acute pancreatitis in an Indian population: a comparative study of the BISAP score, Ranson’s score and CT severity index. Gastroenterol Rep2015;4(3):216-220.
-
Cho JH, Kim TN, Chung HH, Kim KH. Comparison of scoring systems in predicting the severity of acute pancreatitis. World J Gastroenterol 2015; 21(8):2387-2394.
-
Zhang J, Shahbaz M, Fang R, Liang B, Gao C, Gao H, et al. Comparison of the BISAP scores for predicting the severity of acute pancreatitis in Chinese patients according to the latest Atlanta classification. J Hepatobiliary Pancreat Sci 2014;21(9):689-694.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License