IJCRR - 13(5), March, 2021
Pages: 36-41
Date of Publication: 03-Mar-2021
Print Article
Download XML Download PDF
Spectrum Analysis of Thyroid Lesions on Histopathology
Author: Sheema Sheikh, Rohi Wani, Farzana Manzoor, Sabiha Ashraf
Category: Healthcare
Abstract:Introduction: Thyroid gland is an endocrine organ with two lobes and connecting isthmus, located below and anterior to the larynx. Histologically, the thyroid gland is comprised of follicles lined by follicular epithelial cells with eosinophilic colloid in the lumen. Objective: This study aimed to analyse thyroid lesions histopathologically. Methods: Specimens of thyroid lesions received at Department of Pathology, Government Medical College, Srinagar from January 2018 to December 2019 were studied retrospectively. Results: Among the 180 specimens of thyroid lesions, 145 were from female patients and 35 from male patients. Age of the patients ranged from 4 years to 66 years. 31 cases (17%) were found to be non-neoplastic and 149 cases (83%) were neoplastic. Of the non-neoplastic lesions, 28 cases were documented as colloid goitre, 2 cases as a thyroglossal cyst and 1 case as Hashimoto thyroiditis. Of the neoplastic category, benign neoplasms(n=49) included 34 cases of follicular adenoma, 12 cases of Hurthle cell adenoma and 3 cases of non-invasive follicular thyroid neoplasm with papillary like nuclear features malignant category (n=100) included 90 cases of papillary thyroid carcinoma, 2 cases of follicular thyroid carcinoma and 8 cases of medullary thyroid carcinoma. Conclusion: In our study, only 17% of thyroid surgeries were done for non-neoplastic lesions. Further reduction in the number of thyroidectomies for non-neoplastic lesions is expected with improved applicability of preoperative imaging and fine-needle aspiration cytology.
Keywords: Thyroid, Histopathology, Neoplastic, Papillary Thyroid carcinoma
Full Text:
INTRODUCTION
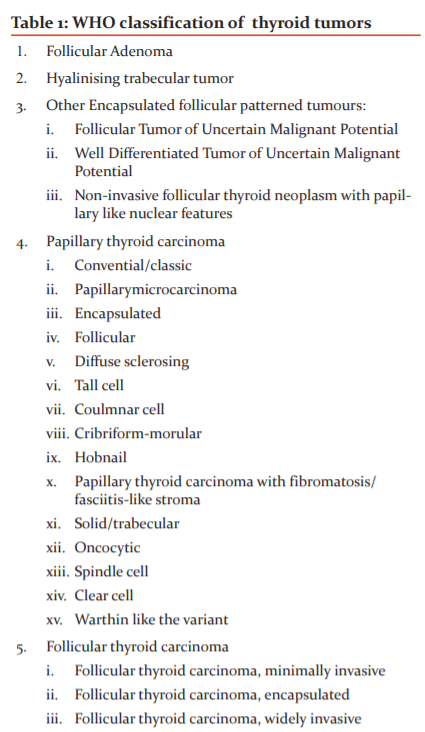
Thyroid gland is an endocrine organ with two lobes and connecting isthmus, located below and anterior to the larynx. Histologically, the thyroid gland is comprised of follicles lined by follicular epithelial cells with eosinophilic colloid in the lumen.1 C-cells are interspersed within the follicular epithelium with basement membrane investing both follicular as well as C-cells. Common diseases of thyroid encountered in histopathological specimens include developmental (pyramidal lobe, thyroglossal duct cyst, lingual thyroid), inflammation (thyroiditis), thyroid hyperplasia (goitre), and neoplasms.2 The updated classification of thyroid neoplasms (Table 1) has been introduced in the 4th Edition of the WHO classification of endocrine organs in 2011.3 The precise classification of thyroid neoplasms has always been onerous owing to the evolution of molecular/genetic characterisation of these tumours, introduction of new entities, reclassification of previous entities and updates in diagnostic criteria. This study was undertaken to thoroughly analyse thyroid lesions and thereby establishing the histopathological spectrum.
MATERIALS AND METHODS
This was a retrospective study conducted at the department of pathology, Government Medical College, Srinagar. The records of all thyroid specimens received in the department over 2 years (January 2018 to December 2019) were acquired from departmental registry and histopathology requisition forms. The clinical history including age, gender, symptoms, radiological and cytologic findings were noted. The slides were retrieved from the departmental gallery and wherever necessary, fresh 4-5micron sections were cut on a microtome and stained by Hematoxylin and Eosin stain. All the cases were studied by more than one pathologist. The data were entered in Microsoft Excel spreadsheet and was then imported into statistical package for social science (SPSS) version 20 for statistical analysis.
RESULTS
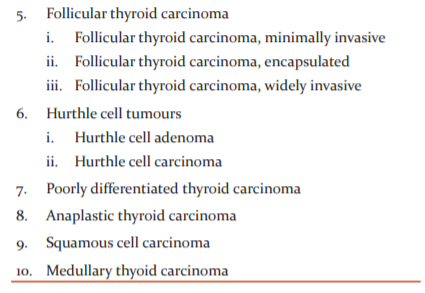
In the two years from January 2018 to December 2019, a total of 180 specimens of thyroid lesions designated thyroidectomy, lobectomy, partial excision and Sistrunk operation have been received in our department. Overall female patients outnumbered male with F: M ratio of 4.14:1 (Figure 1, Table 2). The maximum lesions predominated in the age group of 21-40 years (n=102) (Table 3).
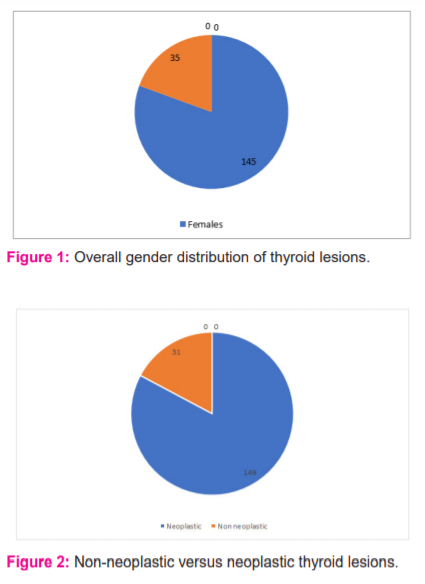
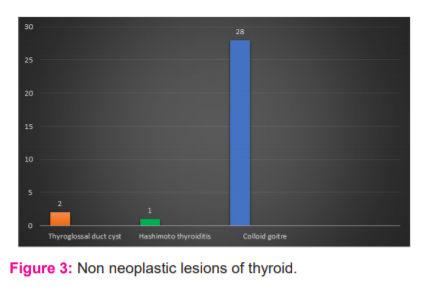
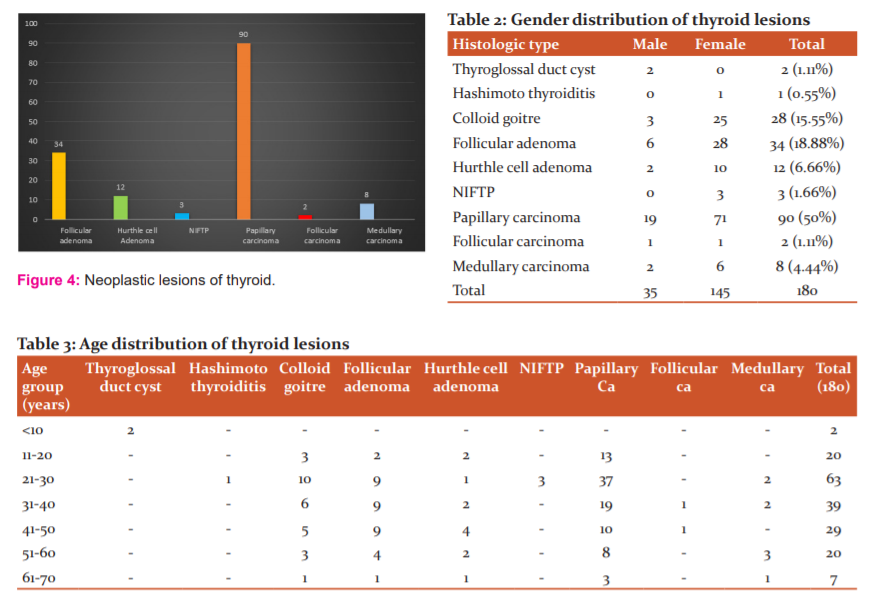
The non-neoplastic lesions constituted 17% (31 cases) of all thyroid lesions (Figure 2). Colloid goitre was the most common non-neoplastic lesion (28/31, 90.32%). Of these cases, 25 were female (89.28%) and 3 were male (10.71%). Two cases(6.45%) of the thyroglossal cyst and 1 case (3.22%) of Hashimoto thyroiditis were found (Figure 3). In this study, 149 cases (83%) belonged to the neoplastic category. Of these cases, 49 (32.88%) were benign and 100 (67.11%) were malignant. In the benign category,34 cases of follicular adenoma, 12 cases of hurthle cell adenoma and 3 cases of Non-Invasive Follicular Thyroid neoplasm with Papillary like nuclear features (NIFTP)were found. The female to male ratio was 5.1:1 and the majority cases were in the age group of 21-50 years (Figure 4, 5).
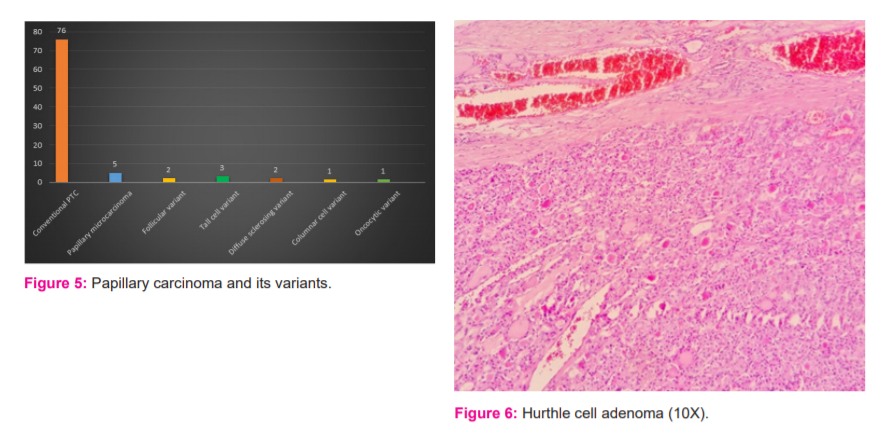
Among the malignant thyroid neoplasms, papillary thyroid carcinoma, PTC was found to be the most common malignant thyroid lesion (90 cases). Of these cases, 71 were female and 19 were male with F: M ratio of 3.7:1 and most of the patients was in 21-40 years of age group (n=56). Two cases of follicular carcinoma (minimally invasive) and 8 cases of medullary carcinoma were documented (Figure 4). Conventional/classic type percutaneous tranhepatic cholangiography (PTC) constituted 84.44% (76/90) of PTC cases. Also, 6 variants were identified including papillary microcarcinoma (5 cases), invasive follicular variant (2 cases), tall cell variant (3 cases), diffuse sclerosing variant (2 cases), columnar cell variant (1 case) and oncocytic variant (1 case) (Figure 5). One of the two cases of the diffuse sclerosing variant was found in association with the thyroglossal cyst.
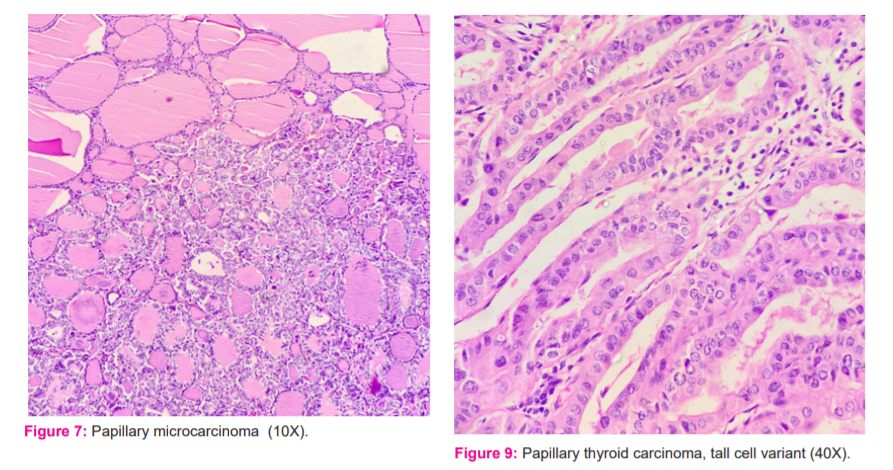
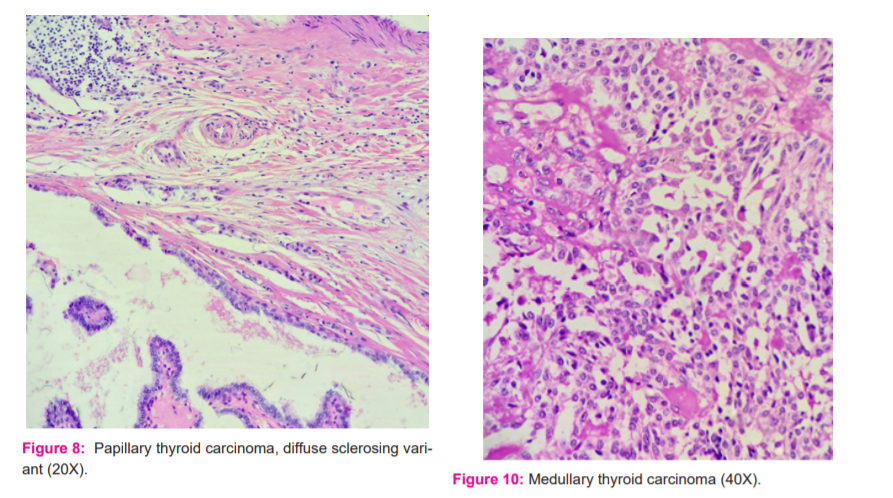
Photomicrographs of some of the thyroid lesions are shown as hurthle cell adenoma (Figure 6), papillary microcarcinoma (Figure 7), a diffuse sclerosing variant of PTC (Figure 8), a tall cell variant of PTC (Figure 9) and medullary thyroid carcinoma (Figure 10).
DISCUSSION
Thyroid lesions are common all over the world and the histopathological spectrum of these lesions vary according to the geographical region, race, age and gender of the studied population. In concordance with the previously published literature,4-9 our study demonstrated that females are more commonly affected than males with the majority of the lesions documented in the age group of 21-40 years.
Both neoplastic and non-neoplastic lesions of thyroid are found in this part of the world and we found that neoplastic lesions are more common than non-neoplastic ones in the thyroid specimens sent for histopathological examination. Majority of other authors reported a higher percentage of non-neoplastic lesions, constituting 72.3%, 82%, 83.3% and 84% of thyroid lesions respectively in the studies by Albasri et al.10 Sreedevi et al.11, Fatima et al.5 and Prabha et al.7 In a study by Ramesh12, neoplastic lesions (52.5%) marginally exceeded the non-neoplastic lesions (47.5%). This deviation from the previously published literature could be because of the applicability of fine-needle aspiration cytology and increased expertise of cytopathologists7-9 in accurately diagnosing thyroid lesions, thereby reducing the burden of unnecessary surgeries for non-neoplastic lesions. Also, the increased detection of malignant lesions with the introduction of high-resolution imaging techniques may be responsible for the increased incidence of neoplastic lesions in our study.
Among the non-neoplastic lesions, colloid goitre was the most common lesion in our study similar to the previous studies.10-12 The low frequency of Hashimoto thyroiditis in our study was also noted by other authors.13-15 Of the neoplastic lesions, the most common benign tumour reported was follicular adenoma, in consonance with literature.10,12,16 All cases of follicular adenoma showed a single lesion except for one where multiple lesions were identified in right lobe and isthmus. Malignant lesions were found to be more common than benign paralleling the earlier studies.10,17
The most common malignant thyroid tumour is PTC, constituting 85-90% of all differentiated thyroid cancers and females are affected four times than males.1,2,22 PTC was the commonest malignant lesion (91.83%) in our study supporting the increasing trend of this carcinoma documented in studies by other author.12,17-21 The F: M ratio for PTC in our study was 3.7. Similar to earlier studies,11,12,17,18 majority of the PTC were of conventional type (84.44%). Tall cell variant, diffuse sclerosing variant and columnar cell variant are acknowledged by WHO classification of thyroid tumours as biologically aggressive variants, all of which showed up in our study with the frequency of 3.33% (n=3), 2.22% (n=2) and 1.11 % (n=1) respectively. The newly described hobnail cell variant is also proposed to have probably more aggressive biological behaviour.23 Tall cell variant is one of the more common aggressive types of PTC, seen in a slightly older age group than conventional variant.18,24,25 In our study, all three cases were older than 40 years of age.
Oncocytic papillary carcinoma is a rare variant characterised by papillary structures with thin fibrovascular cores covered by oncocytic cells.18 This type was first reported in 1995.26 It accounts for less than 10% of all papillary carcinomas 27and less than 0.5% when purely oncocytic without admixture of other patterns3. In our study, only one case (1.11%) of pure oncocytic papillary carcinoma was documented. Follicular thyroid carcinoma, FTC and medullary thyroid carcinoma, MTC account for 6-10 % and 2-3% of all thyroid carcinomas.3 In the current study, there were two cases of follicular carcinoma both were minimally invasive, accounting for 2% of thyroid carcinoma. MTC was the second most common type of malignancy in our study (8%, n=8) and no case of anaplastic carcinoma was found. This retrospective study was of shorter duration (two years), thereby explaining the disparity in the percentages of less common thyroid cancers.
CONCLUSION
This study points to the evolving histopathological spectrum of thyroid diseases with neoplastic lesions showing up as major chunk in thyroidectomy specimens. Females constituted the majority of thyroid lesions and more than half cases were in the age group of 21-40 years. Colloid goitre was the most common non-neoplastic lesion, follicular adenoma, the most common benign tumour and papillary thyroid carcinoma, the most common malignant lesion.
CONFLICT OF INTEREST: Nil
SOURCE OF FUNDING: Nil
ACKNOWLEDGEMENT: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references to this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed
References:
-
Kumar V, Abbas AK, Aster JC. Robbins and Cotran Pathologic Basis of Disease. 9th Edition. Philadelphia: Elsevier Saunders; 2015.
-
Pfeifer JD, Dehner LP, Humphrey PA. The Washington Manual of Surgical Pathology. 3rd ed. Philadelphia, PA: Wolters Kluwer, 2019.
-
Lloyd RV, Osamura RY, Kloppel G, et al. WHO Classification of Tumors: Pathology and Genetics of Endocrine Organs. 4th ed. Lyon, France: IARC;2017.
-
Haque WS, Yasmin S, Islam SMJ, et al. Histomorphologic spectrum of thyroid lesions in surgically treated thyroid specimens. Br Dem Med J 2020;10(1):54-59
-
Fatima A, Tolnur RA, Patil BV, et al. Histopathologic spectrum of thyroid lesions. Ind J Path Oncol 2018;5(2):298-301.
-
Abboud B, Ghorra CS, Rassy M. Epidemiologic Study of Thyroid Pathology in a University Hospital. Acta Chir Belg 2015;115:414-417.
-
Prabha V, Bhuvaneswari MG. A study of the histopathological spectrum of thyroid lesions. Int J Sci Stud 2019;7(1):1-4.
-
Negro R, Gharib H, Savoldi L, et al. A longitudinal study of thyroidectomised patients in a region of north Italy: Benign versus malignant disease. Endocr Pract J 2013;19(2):145.
-
Antony J, Celine TM, Chacko M. Spectrum of thyroid disorders: A retrospective study at a medical college hospital. Thyroid Res Pract 2014;11(2):261-264.
-
Albasri AK, Sawaf Z, Hussany AS, et al. Histopathological pattern of thyroid disease in Al-Madinah region of Saudi Arabia. Asian Pac J Cancer Prev 2014;15(14):5565-5570.
-
Sreedevi AR, Sheela KM. Histopathological spectrum of non-neoplastic and neoplastic lesions of thyroid- a 2-year study in a tertiary care teaching hospital. J Med Sci Clin Res 2018;6(6):145-149.
-
Ramesh VL, Ramu S. Study of distribution of Thyroid lesions in a hospital. Int J Sci Res 2014;3(12):541-545.
-
Maechim G, Young MH. De Quervain's subacute granulomatous thyroiditis: Histologic identification and incidence. J Clin Pathol 1963;16:189-199.
-
Arora HL, Gupta DP. Geographic pathology of thyroid diseases in Rajasthan. J Ind Med Assoc 1967;48:424-428.
-
Jagadale K, Srivastava H and Nimbargi R. Recent trends in the distribution of thyroid lesions in a tertiary care hospital in India. Int J Leps 2016;3(4):234-239.
-
Ariyibi OO, Duduyemi BM, Akang EE. Histopathological patterns of thyroid neoplasms in Ibadan Nigeria: a twenty-year retrospective study. Int J Trop Dis 2013;3:148-156.
-
Beigh A, Amin J, Junaid S. Histopathological study of thyroid neoplastic lesions in a tertiary care hospital – A 5-year study. Int J Cont Med Rea 2018;5(4): D4-D7.
-
Lam AKY, Lo CY, Lam KS. Papillary carcinoma of the thyroid: A 30-yr clinicopathologic review of the histologic variants. Endo Path 2005;16(4):323-330.
-
Yang L, Sun TT, Yuan YN. Time trends and pathological characteristics of thyroid cancer in urban Beijing. Endo Path 2013;47:109-112.
-
Yildiz SY, Berkem H, Yuksel BC. The rising trend of papillary carcinoma in thyroidectomies: 14 years of experience in a referral centre of Turkey. World J Surg Oncol 2014;12:34.
-
Amphlett B, Lawson Z, Abdul Rehman GO. Recent trends in the incidence, geographical distribution and survival from thyroid cancer in Wales. J Thyroid 2013;23:1470-80.
-
Goldblum JR, Lamps LW, McKenney JK, Myers JL. Rosai and Ackerman’s Surgical Pathology. 11th edition. Philadelphia: Elsevier;2018; 283-331.
-
Asioli S, Erickson LA, Sebo TJ. Papillary thyroid carcinoma with prominent hobnail features a new aggressive variant of moderately differentiated papillary carcinoma. A clinicopathologic, immunohistochemical and molecular study of eight cases. Am J Surg Pathol 2010;34:44-52.
-
Prendiville S, Burman KD, Ringel MD, et al. Tall cell variant: an aggressive form of papillary thyroid carcinoma. Otol Head Neck Surg 2000; 122:352-357.
-
Khanafshar E, Lloyd RV. The Spectrum of Papillary Thyroid Carcinoma Variants. Adv Anat Pathol 2011;18(1):90-97.
-
Apel RL, Asa SL, LiVolsi VA, Papillary Hurthle cell carcinoma with lymphocytic stroma. “within-like tumour” of the thyroid. Am J Surg Pathol 1995;19:810-814.
-
Carr AA, Yen TWF, Diana LO. Patients with oncocytic variant papillary thyroid carcinoma have a similar prognosis to matched classic papillary thyroid carcinoma controls. Thyroid 2018;28:1462-1467.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License