IJCRR - 8(4), February, 2016
Pages: 47-49
Date of Publication: 21-Feb-2016
Print Article
Download XML Download PDF
ISOLATION OF CRYPTOCOCCUS NEOFORMANS FROM ABSCESS ASPIRATE IN A PULMONARY TUBERCULOSIS PATIENT
Author: Charmi N. Shah, Mannu R. Jain, Manish G. Patel, Parul Vadgama
Category: Healthcare
Abstract:Cryptococcus neoformans is ubiquitous encapsulated yeast found throughout the world. It predominantly causes significant infections in immunocompromised individuals, of which 80-90% occur in people with human immunodeficiency virus(HIV) infection. Disseminated disease, especially cryptococcal abscess is exceedingly rare. We report a case of disseminated cryptococcosis with abscess in a tuberculosis patient. A case of Cryptococcus neoformans and Mycobacterium tuberculosis (pulmonary) coinfection in an otherwise healthy young man is reported.
Keywords: Cryptococcosis, Abscess, TB
Full Text:
INTRODUCTION
Cryptococcus neoformans is opportunistic yeast commonly found in soil contaminated with pigeon droppings throughout the world.[1,2] Cryptococcosis continues to cause significant morbidity and mortality in immunocompromised as well as immunocompetent persons.[1] The predisposing factors are advanced stage of human immunodeficiency virus (HIV) and other conditions like prolonged use of corticosteroid, lymphomas, solid organ transplant recipients and patients with immune suppressive disease or receiving such drugs.[2,5,8,9] Noncutaneous cryptococcal abscess without osseous involvement is exceedingly rare around 10-15%.[1]
The mainstay of host defence against this pathogen is innate and T-cell-mediated immunity, likely explaining its high incidence among immunosuppressed patients. There is evidence that both M tuberculosis and C neoformans may have suppressive effects on the host immune system. This suggests a mechanism by which an otherwise healthy individual developed these two infections.[[3] A case of Cryptococcus neoformans and Mycobacterium tuberculosis (pulmonary) coinfection in an otherwise healthy young man is reported.
Case description A 30 years old male with history of pulmonary TB presenting with chief complaint of painful swelling over left site of chest since 10 days and fever since 5 days. There was history of anorexia and significant weight loss over last 3 months. There was no history of dyspnoea, chest pain and hemoptysis, abnormal behavior or movements. Patient is on antituberculosis treatment since 3/3/2014 (cat 1 TB).His TB was confirmed by sputum smear AFB examination. The montoux test was positive (>10 mm) with dose of 5 TU PPD after 48 hours. On local examination, tender oval swelling of 11cmx8cmx2cm in size, red in colour and hot on palpation present on left lateral site of chest wall. Systemic examination is normal.
In routine investigation, his ESR was found raised(112mm/hr).All other investigations such as liver function test and renal function tests are found normal. His HIV testing was also non-reactive. He had the history of right frontal bone depressed fracture 2 years back and also had the history of an eviscerated right eye due to injury which was corrected by prosthetic implantation 1 year back. He had steroid administration at that time which could contribute to his immunosuppressed condition. Direct microscopy of aspirate revealed 6-8 pus cells/hpf and very few gram-positive yeast cells.
Inoculation on Sabouraud's Dextrose Agar revealed small opaque creamy white colonies. Gram’s stain from colony showed gram positive budding yeast cells of varying size. India ink preparation of colony showed round, budding halos of varying size. Urease test was positive after 48 hours of incubation. Antifungal Sensitivity done with fluconazole, nystatin, itraconazole, amphotericin B in which only amphotericin B showed sensitivity which was also confirmed by vitek.
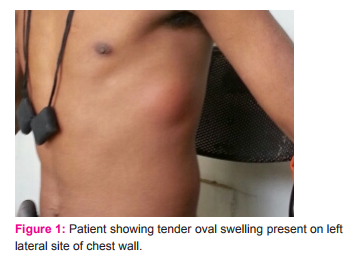
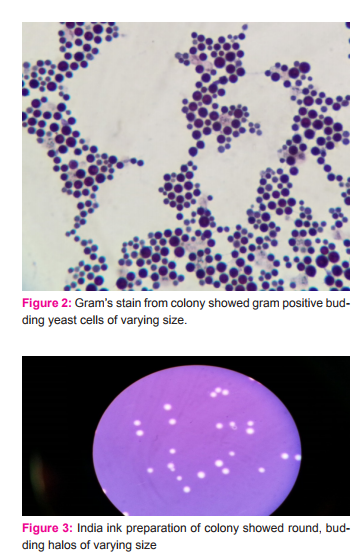
Case discussion The patient came to our hospital for his antituberculosis treatment. Meanwhile he was referred to surgery OPD because of swelling which was suspected as cold abscess on the basis of clinical presentation .Direct microscopy (Gram’s stain, India ink preparation) of the aspirate showed round, budding, capsulated yeast cells resembling Cryptococcus. Patient was initially started empirically with itraconazole but no improvement observed. The isolate was susceptible only to amphotericin B, which was started at a dose of 1 mg/kg/ day in 2 divided doses slowly over 2 hours for 2 weeks followed by capsule fluconazole 400 mg for 8 weeks. After that, the patient’s condition was improved.
CONCLUSION Cryptococcal infection is the most common opportunistic fungal infection in immunocompromised individuals. A high index of suspicion is needed for early diagnosis and it is a good clinical practice to use India ink stain in all cases of cryptococcal infections. Early diagnosis and adequate treatment may save the lives of these unfortunate patients. It is thus recommended that all the body fluids should be subjected to fungal culture and sensitivity even if there is a rarest possibility of fungal infection.
ACKNOWLEDGMENT
To the Department of TB and Chest for continuous support and valuable help. Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Suchitha S., Sheeladevi C.S., Sunila R., Manjunath G.V., Disseminated cryptococcosis in an immunocompetent patient, Hindawi Journal 2012;652351
2. G Serrano Ocana, J.Ortiz Sablon,I Ochoa Tamayo, Disseminated Cryptococcosis :case report, The IntJ of Neurology Jan 2009,vol.10 Issue 2,p5
3. Van Tongeren L, Shaipanich T, Fleetham JA., Coinfection with Cryptococcus gattii and Mycobacteriumtuberculosis in an otherwise healthy 18-year-old woman, Can Respir J 2011 JulAug;18(4): e62-e63.
4. Manfredi R, Calza L., Severe brain coinfection with Cryptococcus neoformans and Mycobacterium tuberculosis in a young, otherwise healthy student recently immigrated from China,Int J Infect Dis 2008; 12(4): 438-441.
5. Sasisopin K., Sirirat W., Roongnapa P.,Somnuck S., Cryptococcosis in human immunodeficiency virus-negative patients, Int J of Inf Dis Jan.2006,vol.10(1):72-78
6. M.capoor,D.nair,M.deb,B.Gupta,P.Aggarwal,Clinical and mycological profile of cryptococcosis in a tertiary care hospital, Ind J of Med Micro., vol 25,no.4,pg. 401-404,2007
7. B.R.Yehia,M.Eberlein,S.D. siscon, D.N. Hager, Disseminated cryptococcosis with meningitis, peritonitis and cryptococcemia in a HIV negative patient with cirrhosis, Cases J,vol 2,no.10,article 170,2009
8. Aoi Kuroda et al., A Case of Disseminated Cryptococcal Infection and Concurrent Lung Tuberculosis in a Patient under Steroid Therapy for Interstitial Pneumonia, Hindawi Case Reports in Pulmonology Volume 2015 (2015), Article ID 358926, 6 pages
9. P Satishchandra1, T Mathew1, G Gadre1, S Nagarathna1, A Chandramukhi2, A Mahadevan3, SK Shankar3,Cryptococcal meningitis: Clinical, diagnostic and therapeutic overviews, Publication of the Neurological society of India Year : 2007 | Volume : 55 | Issue : 3 | Page : 226-232
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License