IJCRR - 12(20), October, 2020
Pages: 61-65
Date of Publication: 27-Oct-2020
Print Article
Download XML Download PDF
A Clinical Case Report on Extra Pyramidal Symptoms
Author: Jaya Pranoykumar Gawai
Category: Healthcare
Abstract:Background: Extrapyramidal signs are side effects of antipsychotic medications when the patient is receiving Schizophrenia treatment. Such signs include dystonia (continuous spasms and muscle contractions), akathisia (may manifest as muscular restlessness), Parkinsonism (characteristic signs such as stiffness), bradykinesia (slow motion), tremor, and intermittent dyskinesia (irregular, jerky motion). Aim: This case report aims to identify extrapyramidal symptoms at the earliest, prevent potential harm and to provide quality of nursing care to the patients. Objectives: 1. To identify extrapyramidal symptoms by the nurses and to report immediately. 2. To take action immediately and to prevent adverse effects. Results: The patient was taking Tab. Olanzapine 20mg for 25 years, abruptly stopped the medicine without consulting to the psychiatrist and the patient started with abnormal movements of lips, head and neck for two days. The patient was treated with Tab.Pacitone12 mg, movements were minimized. Conclusion: The nurses play a vital role at the bedside and take care of psychiatric patients when they receive antipsychotic drugs.
Keywords: Extrapyramidal symptoms, Dystonia, Antipsychotic drugs, Parkinsonism, Olanzapine, Haloperidol MESH TERMS Antipsychotic agents Hypokinesia Dystonia in Parkinson’s disease Dystonia and related activity Benzadiazepines Psychomotor agitation
Full Text:
Introduction
There is evidence that Olanzapine is more effective than Divalproex, causing less nausea but more weight gain, drowsiness and movement disorders. When compared with haloperidol ineffectiveness, Olanzapine induces fewer movement disturbances, but there will be greater weight gain in the individuals treated by the above drugs.1
Olanzapine increases the patient sleepiness more and if the psychiatrist prescribes the dosage of Tab. Olanzapine5mgs may be the likelihood of being reduced sleep of the patient without any harm to the patient. Whereas Tab. Olanzapine 20 mg was prescribed for this particular case, the patient had good sleep and the side effects should be more concerned. There is evidence the patient one who is taking Olanzapine with combined standard treatment might be having improved quality of life than with any one of the treatment alone and still it is not sure.
Extrapyramidal side effects and dyskinesias, as well as in the ECG prolongation of QT interval, the time between the Q and T waves, the time is taken for the heart to repolarise and is corrected to take account of the heart rate. Prolongation of the QT interval may lead to sudden death due to the increased potential of malignant ventricular tachyarrhythmias.2
Case history
This case report has been taken DMIMS (Deemed to be University), Sawangi (Meghe), Wardha where lack of mental health services for the remote population and underprivileged population, Acharya Vinobha Bhave Rural Hospital provides mental health care services for all the needy people.
Patient Information
One of the female patient, 55 years old, got admitted in the psychiatric ward, Acharya Vinobha Bhave Rural Hospital with a known case of Schizophrenia for the past 25 years. Since then she was taking several antipsychotic drugs and regular visit to the psychiatrist. Past two years she was prescribed to take Tab.Olanzapine 20 mg and Tab. Haloperidol 5mgs by the psychiatrist. Her husband understood the cost of Tab. Olanzapine 20 mg is expensive and he stopped the medicine abruptly without consulting to the psychiatrist, continued with the only Tab. Haloperidol 5 mg for two weeks and then the patient herself skipping Tab. Haloperidol 5mgs a week before she comes to the hospital because she claims that the medications had given her chest pain, breathlessness and mouth ulcers. Patient started to develop paranoid spells, believing that her son had pinched her and her husband drained her blood and selling it secretly. She also thinks that her family members were trying to kill her for her property, suspiciousness, aggressive, sleep disturbance, irritabilities and muttering to self and abnormal movements of lips, head and neck since 2 Days. She was taken to AVBRH Psychiatric OPD by her husband and was admitted on 19/1/2020 for further evaluation.
Precipitating factors
According to family history, she is the only daughter and another sibling of an elder brother for their parents. Her parents had special emotional attachment towards her because she is the only daughter, after getting married she started having the symptoms of Paranoid schizophrenia and on regular treatment. Another reason one of her cousins told her that her husband is having extramarital relationships with someone in the year of 1995 since then she started doubting her husband.
Perpetuating factors
The patient is poor compliance to medication for the past week, developed delusional thinking towards her family.
Past psychiatric history
Since 1995 the first episode, she was taken to a psychiatrist and taken treatment for a while. Since then, she always develops suspiciousness towards her husband and even with her relatives when she was on medications. In 2009, after being on antipsychotics for several years, developed muscle spasms, neck rigidity, and headache and then taken to a psychiatrist, she was diagnosed as suffering from the extrapyramidal syndrome.
Signs and symptoms were:
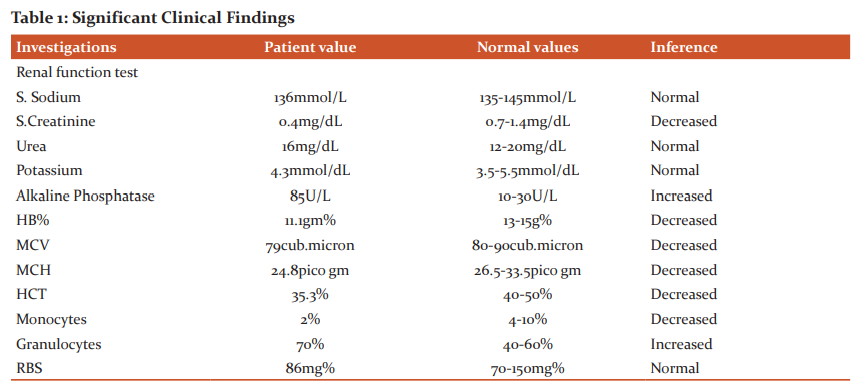
This patient presented with typical symptoms of Bradykinesia, eye spasms or blinking, twisting head, protruding tongue, extended neck, physical discomfort, agitation, anxiety, shaking legs, Repetitive, involuntary facial movements, such as tongue-twisting, chewing motions and lip-smacking, cheek puffing, and grimacing. Changes in gait, jerky limb movements, or shrugging, Rigid muscles and fever, drowsiness and confusion shown in Table 1
Timeline
The patient was admitted for three weeks and the nursing care has been rendered along with the psychopharmacological interventions. The patient discharged from the hospital in a good condition and follow up has been taken regularly in the psychiatric OPD every week.
Diagnostic Assessment
Physical examination: Unstable gait, abnormal facial movements, smacking lips, abnormal neck movements.
Mental status examination: Abnormal speech, inappropriate affect, delusional thought
Presented with Thanatophobia and Pistanthrophobia, Obsessional compulsive phenomena, perceptional abnormalities, attention, concentration, recent and remote memory, intelligence, and judgment was found to be affected and impaired. Disturbed sleeping pattern and anorexia were present in the patient.
Data extraction
Data extracted from PUB MED, Medline, and Cochrane database library.
Follow-up and outcomes
Follow up has been taken regularly, the patient visits psychiatric OPD every week and there were no side effects have been reported.
Primary Outcome
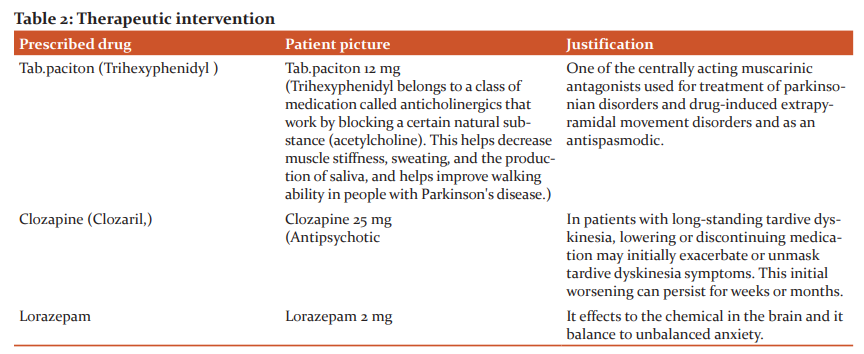
The evidence of extrapyramidal symptoms was minimized by anticholinergic drugs and adjunct with other psychosocial therapies.
Secondary outcome
Regular follow up will prevent adverse effects of newly prescribed antipsychotic drug.
Discussion
Amisulprideequally effective as olanzapine and risperidone, Olanzapine induces a higher increase of glucose. There is no difference in terms of cardiac effects and extrapyramidal symptoms (EPS) compared with olanzapine, risperidone and compared with Ziprasidone.3
Aripiprazole is typical antipsychotics and safer for children having Schizophrenia, this drug induces fewer occurrences of extrapyramidal symptom, and particularly akathisia. There is evidence through RCT it induces hyperprolactinaemia, lesser risk of sinus tachycardia, blurred vision but causes dizziness and nausea.4
The trials compared oral Zuclopenthixol dihydrochloride to placebo, Zuclopenthixol dihydrochloride might be causing more movement disorders than Clozapine, Risperidone or perphenazine, other drug comparisons or placebo.5
One of the animal studies revealed, Haloperidol was administered orally at a dose of 0.2 mg/rat/day in rats for 5 weeks and the rats developed dull chewing movements after 2 weeks but the treatment continued for 5 weeks. Motor coordination observed after 3 weeks and tolerance for the Haloperidol-induced motor impairment after 5 weeks of treatment. Motor activity observed by administration of IMI (intraperitoneally, for 5 weeks) did not have a motor activity or motor coordination.6
Another trial reported Tab. Haloperidolingesting with water is recommended dose by the psychiatrist exhibited reduced exploratory activity without producing akinesia. Motor coordination was impaired at the maximum after 3 weeks treatment and tolerance were developed in the drug-induced motor impairment after 5 weeks of treatment. The intensity of vacuous chewing movements (VCMs) and tardive VCMs was greater by oral administration than intraperitoneal injections of haloperidol. The results show that oral administration of haloperidol produces constant effect thus resulting intolerance in the case of acute parkinsonian but more intensity of tardive dyskinesia. Oral Haloperidol may help alleviate tardive dyskinesia.7
Tardive dyskinesia is a disturbance in the human balance between stimulation of the dopamine receptor and blockage of the dopamine receptor in the motor striatum, with hypothetically too much stimulation of the supersensitive D2 receptor resulting in "don't stop" signalling for motor output.8
There is evidence; dysphagia may be resulted by first- and second-generation of antipsychotics and this may be an extrapyramidal adverse reaction or related to anticholinergic effects of antipsychotics. Management of dysphagia includes discontinue the antipsychotic, reduce the dose, divide the dose, or switching to another antipsychotic drug. Dysphagia may be causing the immediate effect of airway obstruction like choking, asphyxia, aspiration pneumonia, and longer effect of weight loss, dehydration, malnutrition, and poor compliance to an oral antipsychotic drug.9
There is the evidence: olanzapine induces metabolic syndrome and dyslipidemias but less risk of developing extrapyramidal syndromes (EPS) other tardive syndromes are more concern, tardive dyskinesia, tardive akathisia, and tardive dystonia are the commonest tardive syndromes, the others are less common. Tardive oculogyric crises (TOC) are an uncommon form of tardive dystonia. The present patient also had TOC with unsupervised treatment with olanzapine and no report of weight gain. In the case, the low dose of trihexyphenidyl can be started and stopping of Olanzapine and also aripiprazole can be initiated, the present patient also Olanzapine has stopped now.10
Atypical antipsychotics are first-line treatment for schizophrenia because of less risk of EPS compared with conventional antipsychotics. EPS can occur when antipsychotic drugs are prescribed in a higher dose. A typical antipsychotics should balance with other side effects also.11
Intramuscular Midazolam found more effective sedation in agitated patients at 15 minutes than haloperidol, ziprasidone, and perhaps olanzapine. Olanzapine provides more effective sedation than haloperidol.12
The evidence found that olanzapine treatment is associated with a normalization of brain activity in schizophrenia patients. Typical functional changes were found in the frontal cortex and cingulate cortex activity during both cognitive and emotional tasks. During emotional processing, olanzapine treatment seems to be specific it regulates the activity of the striatum and limbic system and it is called emotional brain.13
Recent research evidence supports the use of olanzapine, to treat anorexia nervosa and chemotherapy-induced nausea in cancer patients. The evidence for high dose olanzapine dosages >20 mg remains limited.14
There may be an incident of olanzapine-induced thrombocytopenia and neutropenia when the patient takes for the first time. One of the cases reported the patient developed biochemical neutropenia and thrombocytopenia without any clinical symptoms, the symptoms resolved after complete stoppage of the drug. Although its comparative uncommonness, case report to a growing corpus suggests that Clinicians and Psychiatrists should maintain keen observation of patients when they prescribe Olanzapine and regular monitoring of haematological counts to find out any abnormalities or immunosuppression.15
The rise of liver enzymes is slightly more frequent with Clozapine and Olanzapine than Risperidone, Perazine and Haloperidol.16
The main complication of the anti-psychotic drug is Neuroleptic Malignant Syndrome arise from renal failure because of the presence of myoglobin in the urine produced by rhabdomyolysis; respiratory insufficiency due to aspiration pneumonia due to the promise of conscience and dysphagia; myocardial infarction which causes heart insufficiency and arrhythmias. There is evidence, Neuroleptic Malignant Syndrome can occur because of the dose of neuroleptics was increased. However, this syndrome can also be precipitated by the withdrawal of drugs, since they cause a sudden interruption of the dopamine availability in the brain.17 Olanzapine is a better choice of drug for schizophrenic patients, it causes less Extra Pyramidal Symptoms.18
One of the RCT, olanzapine is statistically significant superiority to the haloperidol group on the primary analysis (p<0.001). In secondary analyses also confirmed olanzapine's superiority in DIEPSS total, Parkinsonism, akathisia and overall severity scores (all p< or =0.014). Categorical analysis of treatment-emergent akathisia and Parkinsonism syndromes at endpoint shows improvement in the olanzapine group but the deterioration in the haloperidol group.19
To determine the effective antipsychotic drug doses the comparison between olanzapine and haloperidol, Olanzapine exhibited a statistically significantly lower extrapyramidal symptom profile than the conventional antipsychotic of haloperidol. The lower extrapyramidal symptom with olanzapine is marked despite statistically significant more frequently the uses of anticholinergic drugs are prescribed with haloperidol to prevent EPS. Few patients received haloperidol discontinued because of EPS than olanzapine and better adherence to the drug for a long time with negligible anticholinergic-associated events.20
Olanzapine give better clinical results than haloperidol measured through Brief psychiatric rating scale significantly compared between olanzapine and haloperidol.21
Conclusion: Nurses should understand the adverse effects of antipsychotic drugs when they are administering to the patients, timely information to the psychiatrist will prevent potential harm of the patients and educate the family members to come for the follow up regularly after discharge.
Informed Consent
The patient was informed and taken written consent before the initiation of the case report.
Conflict of interest
Nil
Financial resource of the study
Nil
Acknowledgement
I am indebted to express my appreciation to my postgraduate students and reviewers for sharing his pearls of wisdom with me during the course of time. I am also immensely grateful to the editor and publishers for their comments and contribution for the success.
References:
-
Rendell. Olanzapine alone or in combination for acute mania. JM-2003;http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004040.[Cited 2020 May 26].
-
Olanzapine for the prevention and treatment of cancer- related nausea and vomiting in adults.2018;http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012555.[Cited 2020 May26].
-
Komossa. Amisulpride versus other atypical antipsychotics for schizophrenia. K-2010: http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006624.[Cited 2020 May26].
-
Bhattacharjee. Arpiprazole versus typical antipsychotic drugs for schizophrenia. J-2008; http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006617.[Cited 2020 May26].
-
Bryan EJ, Purcell MA, Kumar A. Zuclopenthixol dihydrochloride for schizophrenia. Cochrane Database Syst Rev [Internet]. 2017 [cited 2020 May 26] ;( 11). Available from:https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005474.
-
Samad N, Haleem DJ. Haloperidol-induced extrapyramidal symptoms attenuated by imipramine in rats. Pak J Pharm Sci. 2014 Sep; 27(5):1497–501.
-
Qu I, Dj H. OralAdministration of Haloperidol at Clinically Recommended Doses Elicits Smaller Parkinsonian Effects but More Tardive Dyskinesia in Rats. Vol. 26, Pakistan Journal of pharmaceutical sciences. Pak J Pharm Sci; 2013 [cited 2020 May 28].
-
Stahl SM. Neuronal traffic signals in tardive dyskinesia: not enough “stop” in the motor striatum. CNS Spectr. 2017; 22(6):427–34.
-
Crouse EL, Alastanos JN, Bozymski KM, Toscano RA. Dysphagia with second-generation antipsychotics: A case report and review of the literature. Ment Health Clin. 2017 Mar; 7(2):56–64.
-
Bavle AD, Kumar GMN. Olanzapine-induced Tardive Oculogyric Crises. Indian J Psychol Med. 2013 Oct; 35(4):423–4.
-
Jm P. Extrapyramidal Symptoms with Atypical Antipsychotics?: Incidence, Prevention and Management.Vol. 28, Drug safety. Drug Saf; 2005 [cited 2020 May 28].
-
Klein LR, Driver BE, Miner JR, Martel ML, Hessel M, Collins JD, et al. Intramuscular Midazolam, Olanzapine, Ziprasidone, or Haloperidol for Treating Acute Agitation in the Emergency Department. Ann Emerg Med. 2018; 72(4):374–85.
-
LDF, GD, AD, PB. Effects of Olanzapine during Cognitive and Emotional Processing in Schizophrenia: A Review of Functional Magnetic Resonance Imaging Findings. Vol. 34, Human psychopharmacology. Hum Psychopharmacol; 2019 [cited 2020 May 28].
-
AmM, ED, LC, Jt K. New Discoveries for an Old Drug: A Review of Recent Olanzapine Research. Vol. 132, Postgraduate medicine. Postgrad Med; 2020 [cited 2020 May 28].
-
Pang N, Thrichelvam N, Naing KO. Olanzapine-induced Pancytopenia: A Rare but Worrying Complication. East Asian Arch Psychiatry Off J Hong Kong Coll Psychiatr Dong Ya Jing Shen Ke Xue Zhi Xianggang Jing Shen Ke Yi Xue Yuan Qi Kan. 2017 Mar;27(1):35–7.
-
Manceaux P, Constant E, Zdanowicz N, Jacques D, Reynaert C. Management of marked liver enzyme increase during olanzapine treatment: a case report and review of the literature. Psychiatr Danub. 2011 Sep; 23 Suppl 1:S15-17.
-
20-113-ENG-112-6-773500.pdf. [Cited 2020 May 28].
-
Chan HY, Chang CJ, Chiang SC, Chen JJ, Chen CH, Sun HJ, et al. A randomised controlled study of risperidone and olanzapine for schizophrenic patients with neuroleptic-induced acute dystonia or parkinsonism. J Psychopharmacol Oxf Engl. 2010 Jan; 24(1):91–8.
-
Inada T, Yagi G, Miura S. Extrapyramidal symptom profiles in Japanese patients with schizophrenia treated with olanzapine or haloperidol. Schizophr Res. 2002 Oct 1; 57(2–3):227–38.
-
Tran PV, Dellva MA, Tollefson GD, Beasley CM, Potvin JH, Kiesler GM. Extrapyramidal symptoms and tolerability of olanzapine versus haloperidol in the acute treatment of schizophrenia. J Clin Psychiatry. 1997 May; 58(5):205–11.
-
Tollefson GD, Beasley CM, Tran PV, Street JS, Krueger JA, Tamura RN, et al. Olanzapine versus haloperidol in the treatment of schizophrenia and schizoaffective and schizophreniform disorders: results of an international collaborative trial. Am J Psychiatry. 1997 Apr; 154(4):457–65.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License