IJCRR - 8(8), April, 2016
Pages: 44-49
Date of Publication: 20-Apr-2016
Print Article
Download XML Download PDF
INTRAOPERATIVE AND POSTOPERATIVE COMPLICATIONS, ACCIDENTS AND FAILURES RELATED WITH DENTAL IMPLANT APPLICATIONS
Author: Damla Torul, Mehmet Cihan Bereket, Ismail Sener, Ali Ilker Bastan
Category: Healthcare
Abstract:With revolutions in biotechnology, implant surgery has become a routine therapy in the last three decades for the rehabilitation of completely or partially edentulous patients. Despite implant surgery increasing popularity and high success rates of, complications due to implant therapy are still unavoidable. Complications can occur either intra-operative or post-operative period of the surgery. Intra-operative complications such as hematoma and ingestion or inhalation of mechanical components or instruments can be serious as life-threatening. Other complications that occur during implant placements are usually associated with local damages such as nerve injury, adjacent teeth damage and perforations of the nasal cavity or maxillary sinus. Also mandible fractures, sinusitis, peri-implant mucositis, peri-implantitis and periapical implant lesions are the complications that frequently encountered after surgery. Therefore implant therapy is a complicated procedure and the management of the complications associated with this therapy requires a special training and experience. This review categorized complications associated with dental implant applications and discusses management options of these complications.
Keywords: Dental implant, Displacement, Hemorrhage, Life-threating, Nerve injury
Full Text:
INTRODUCTION Dental implants are appliances placed in the jawbones for the management of tooth loss to maintain adequate function and aesthetic [1].Since dental implants have been first introduced in 1970s, they are used in various areas of the mouth with an increasing success rate and popularity[2,3].In 2003, Ardekian et al. [4] reported the 5-year success rate of implants range between 93 % and 97 %.However, complications in implant surgery are frequently encountered and management of these complications are become an important issue [5-7]. Until recently, these implant-related complications have increased by the increase in the number of implants placed and dentists, not only specialist, placing implants [2]. This article examined implant complications in two parts. The first section focuses on intraoperative complications and the second segment addresses the post-operative complications of the implant therapy.
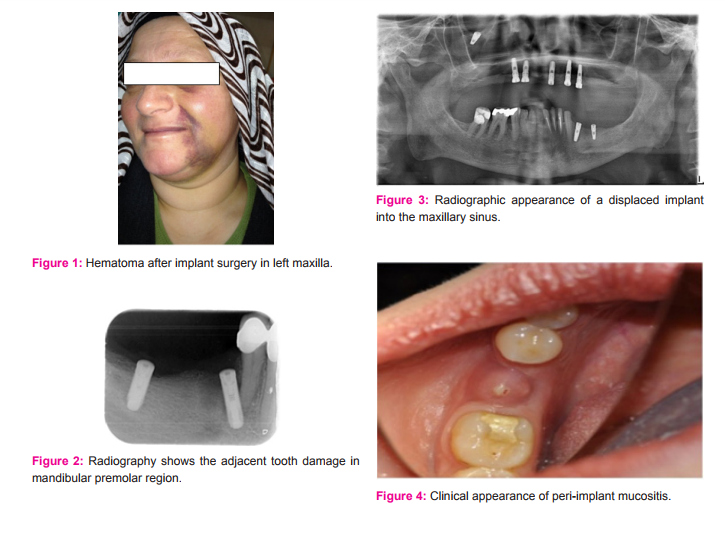
INTRAOPERATIVE COMPLICATIONS Intraoperative complications occur during surgeries and could either be life threatening or local damage triggering. Hemorrhage Hemorrhages can occur during any kind of surgery and they can be taken care of by simple local measures. However, excessive and long lasting hemorrhage is generally considered to be a complication, while it is rarely as serious as life threatening [4,8]. Severe hemorrhages can be associated with the incision of arteries, sinus-lift procedures and preparation of the implant hole [5].The facial and maxillary arteries and their branches are mainly provided the blood supply of the mandible [6].During surgery these arteries may be injured because of the perforation of cortical plates and may leads hemorrhagic accidents [6].Bleeding can be result with a “pseudo-Ludwig phenomenon” which is characterized by elevation of the tongue, elevation of the floor of the mouth and airway obstruction[9]. In maxilla the posterior superior alveolar, infraorbital, descending palatinal and posterior palatin arteries can be damaged during placement of implant or sinus lift procedures [5,6]. Bleeding which arise from the branch of the maxillary artery has been described previously [10,11]. In the presence of hemorrhage, treatment techniques include bone wax, compression, electrocoagulation, bone grafts and in severe cases ligation of the damaged vessels [5,7,8].
It is not recommended to aspirate the area because of its limiting effect on the tamponading effect of the blood clot. In the cases which have restricted visibility external carotid angiography and endovascular management may be necessary [9]. In severe cases airway control can be provided by nasotracheal intubationand cricothyroidotomyor tracheostomy [11]. To prevent this kind of complication, detailed preoperative evaluation and rigorous surgery should be provided. Also, preoperative CT scans and usage of short implants in the risk areas decreases the prevalence of this complication(Figure 1) [4,7,12].
Involuntary Ingestion or Inhalation of Mechanical Components or Instruments During intraoperative period of surgery, a slippery area shows up due to blood and saliva. Hence, the instruments or implant components can slip and fall into the mouth accidentally from the operator’s hand [8].In these accidents, instruments can aspirated or ingested in 13 % and 87 % of the cases respectively [13].Also, sharpness of the instruments may cause vital structure injuries[13]. Therefore, a life threatening complication may occur when these materials are ingested or inhaled by the patient [7,8]. When the instrument is in the gastrointestinal tract the first management options are radiographic examination and a fiber-rich diet [13]. If, a foreign object is aspirated, airway embarrassment can occur and this is a potentially life-threatening condition. Thus, the patient airway must provide immediately and the foreign object should remove as quick as possible [5,14]. Also, bronchoscopy or gastroscopy are useful to reduce the morbidity [13].
To prevent this complication, gauze throat screens and silk ligatures can be used during surgery[5,14]. Nerve injury Neurosensory disturbances are unpleasant experiences that occur as a result of poor flap design, direct mechanical damage to nerve, compression of intra-alveolar edema or hematoma, excessive preparation during implant placement, nerve repositioning and implant placement in atrophic mandible [4,5,7,8]. These disturbances are classified in increasing severity as neuropraxia, axonotmesis and neurotmesis, respectively. Generally these injuries are temporary and continue as 4 weeks to 10 months [7]. Within this period, patients with such injuries may have difficulties performing common activities due to paresthesia, anesthesia dysesthesia or hyperesthesia [7,15]. Commonly inferior alveolar nerve, the mental nerve, the incisor branch of the mandibular nerve, the lingual nerve, and the nasopalatine nerve are likely to be exposed to iatrogenic injury during implant placement procedures [8]. To prevent the nerve injury the preoperative evaluation and exact localization of anatomic structures in the implantation area are mandatory. CBCT and CT scans are the techniques of choice for locate the anatomic structures [6,7,16].
When nerve injury occur as a result of pressure originate from an implant, management options include the removal of the implant or placement of a short implant. In the cases of minor injuries spontaneous healing can observed within days or months. However, prolonged pressure and neuritis may result with permanent degeneration of the nerve [17]. The primary treatment of nerve injuries include neuronal anti-inflammatory drugs or vitamin B-complex, but if a persistent anesthesia or dysesthesia is present more specialized procedures such as microsurgery may be required [5,17]. Damage to Adjacent Teeth Adjacent tooth damage is a rare complication of implant surgery and generally occurs with single implant placements [4,8].Tooth damage can be associated with inadequate distance between the implant and adjacent tooth, wrong angulation of the implant or occurrence of excessive heat during surgery [18].
As a result of above mentioned factors total or partial vitality loss can be seen in the adjacent tooth. Patients are generally asymptomatic but pain or sensitivity may occur occasionally [8]. To prevent the damage of adjacent tooth, a minimum distance of 1,5 to 2mm should be provided between adjacent tooth and the implant [6,7].Also, pre-surgical computed tomography may help ensure accurate diagnosis [18].In the presence of this complication, root-canal treatment, apicectomy and extraction are among the available treatment options(Figure 2) [6]. Perforations of Nasal Cavity or Maxillary Sinus Placement of implants in maxilla close to the nasal cavity or maxillary sinus may result with the perforation of the maxillary sinus or the nasal floor [5-8,19]. Management of perforations of the sinus membrane is commonly provided with the placement of biomaterials [6,19]. Other methods for treating perforation are folding the membrane up against itself, using sutures and fibrin glue[19].However, in the presence of large perforations surgery must postpone during the healing process [7,8]. Several investigators mentioned that these complications are generally well-tolerated and didn’t affect the implant survival [4,5,7].
Displacement of the Implant Inside the Sinus or Nasal Cavity Insertion of implant several millimeters into the sinus or nasal cavity is well tolerated [7]. However, displacement of the implant inside the sinus or nasal cavity is a serious complication [8]. This may be caused by inadequate primer stability, suction effect and improper distribution of occlusal forces [6]. Also, thin maxillary bone, inadequate planning and lack of experience are contribute the movement of the implants in the maxillary sinuses and nasal cavities [20]. In the case of a dislocated implant, it must remove surgically by intraoral or transnasal approach to prevent further complications [6,8]. To prevent these complications knowledge of anatomy, correct pre-surgical planning and adequate post-surgical follow up is mandatory(Figure 3) [6].
EARLY POSTOPERATIVE COMPLICATIONS Mandible Fractures The most important risk factor for the mandible fractures is the placement of an implant in the severely atrophic mandible. Also, lateralization of inferior alveolar nerve increases the risk of the fracture [4,6,7]. The compression stress during these surgical procedures and the prepared osteotomy sites weakens bones and leads to pathologic fractures [4]. The reported prevalence of this complication is 0,2% in the edentulous mandible [21]. Fractures of the mandible associated with implant placement can occur either immediately or in the post-operative period of the surgery [22]. To avoid such complications, Parkand Wang [17] mentioned that atrophic mandible must have a minimum of 7 mm height and 6 mm width. The management of this complication is related with severity of the fracture, volume of the mandibular bone and the location of the implant [5,7].
Open reduction or conservative approaches with bone grafts can used for the fixation of the fractured mandible [22]. Flap Dehiscence Dehiscence can be defined as the surgical wound opening that result with the exposure of the dental implant [8].Coverscrew loosening, mechanical irritation and flap tension are among the contributing factors of this complication [17]. The reported incidence of this complication vary between 2% and 13% [6].In the presence of small dehiscence, granulation tissue can compensate the opening but if the dehiscence is large re-suturing of the area should be performed [8].
Emphysema Emphysema is a complication which is caused by the high intraoral pressure and it is rarely encountered [7,8]. Air originate from the surgical devices or materials can be forced into the surgical area and the emphysema will occur [7]. Clinically it presents with swelling of half of the face and patients complained of pain similar to the tension sensation [23]. A characteristic crackling sound is evinced upon palpation [8,23]. Massage and compression are the therapeutical measures to manage emphysema by accelerating resorbtion of the air trapped in the tissues [8].
LATE POSTOPERATIVE COMPLICATIONS Failed Osseointegration Impaired healing, occlusal loading during osseointegration, failure to follow the planned protocol, technical errors during surgery, infections and especially bone overheating during implant site preparation leads failures in osteointegration. Lack of osseointegration is results in loss of the implant [8,24].Failure of endosseous implants can occur before or after occlusal loading with a prosthetic superstructure. The reported failure rate is from 0,7% to 3,8% [25]. Infections Maxillary Sinusitis Posterior maxilla is a complicated area for implant placement, so sinus lifting and grafting procedures are usually used to overcome the limitations of this area. However, complications include sinusitis and infection can unavoidably occur as a result of these procedures [26]. Symptoms of sinusitis may include fever, facial pain, and yellow to green purulent discharge from the nose, which may drain posteriorly causing a cough and malaise [7]. Management of implant associated sinusitis is surgical and maintaining the drainage and ventilation are the purposes of this procedure [20].
Peri-Implant Mucositis Peri-implant mucositis is defined as the reversible inflammation of the mucosa adjacent to the implant and may be caused by inadequate prosthetic restorations, poor oral hygiene and improper abutments or healing caps [4,27,28]. Generally no signs of bone losses are observed in this situation [4]. Reddish color of the inflamed mucosa adjacent to implant, swelling and bleeding are the clinical features of the periimplant mucositis[28]. Mechanical, antiseptic and antibiotic treatments are possible procedures of choice for controlling an ongoing infection (Figure 4)[28].
Peri-Implantitis Peri-implantitis is an inflammatuar process around tissues of an implant and it results with the loose of the bone around the implant [29,30]. It is an important cause of implant failures and accounts for 10% to 50% of all failures observed one year after the implantation [1]. Early implant exposure, poor oral hygiene are the risk factors contributing peri-implantitis [4]. Diagnosis of peri-implantitis is based on degree of supporting boneloss, clinically detectable pocket depths, purulent discharge and implant mobility [28]. Management of peri-implantitis depend on the severity of the cases and include debridement, antimicrobial treatment or regenerative procedures [1,30].
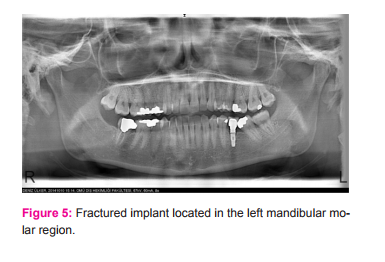
Periapical Implant Lesions The symptoms of apical peri-implantitis is pain, swelling, tenderness and occasionally the presence of a fistula [31]. Possible causes of this complication are excessive heating, contamination, vascular ischemia and pre-existing bone pathology [4,31,32]. Removal of granulation tissue, curettage of the bony walls and if the primary stability is absent scarification of the implant are the treatment options [32]. Implant Fractures Implant fracture is a biomechanical complication with the reported incidence of 0,2 % in totally edentulous and 1,5 % in the partially edentulous jaws. The lack of periodontal ligament is an important risk factor for this complication and hinder the compensation against the forces that occur at the time of chewing [33].
Also bone loss, manufacturing defects, excessive occlusal load and patients-related habits are the other possible causes of the implant fractures [30]. To overcome these shortcomings, periodic occlusal evaluation and proper preoperative planning by considering biomechanical principles are essential. Removal of the implant, modification of the existing prosthesis or modification of the fractured implant are the options for management of this condition (Figure 5) [34].
CONCLUSION Nowadays, there is no doubt that implant therapy has become the most predictable treatment option for rehabilitation of tooth loss. However, complications related with implant therapy are inevitable events that effect the success of the entire therapy. To reduce the incidence of these complications knowledge of surgical anatomy, careful clinical and radiographic examination, proper treatment planning, usage of appropriate instruments and rigorous surgery are important prerequisites. If all of these factors are carefully followed, the complications are effectively avoided. But, adequate training and experience are required when these complications occur.
References:
1. Hadi S, Ashfaq N, Bey A, Khan S. Biological factors responsible for failure of osseointegration in oral implants. Biology and Medicine 2011;3(2):164-70.
2. Wheeler SBCM. Complication or Substandard Care? Risks of Inadequate Implant Training. Cda Journal 2009;37(9):647-51.
3. Bornstein MM, Halbritter S, Harnisch H, Weber HP, Buser D. A retrospective analysis of patients referred for implant placement to a specialty clinic: indications, surgical procedures, and early failures. Int J Oral Maxillofac Implants 2008;23(6):1109-16.
4. Ardekian L, Dodson TB. Complications associated with the placement of dental implants. Oral Maxillofac Surg Clin North Am 2003;15(2):243-9.
5. Misch K, Wang HL. Implant surgery complications: etiology and treatment. Implant Dent 2008;17(2):159-68.
6. Lamas Pelayo J, Penarrocha Diago M, Marti Bowen E. Intraoperative complications during oral implantology. Med Oral Patol Oral Cir Bucal 2008;13(4):E239-43.
7. Greenstein G, Cavallaro J, Romanos G, Tarnow D. Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: a review. J Periodontol 2008;79(8):1317-29.
8. Annibali S, Ripari M, La Monaca G, Tonoli F, Cristalli MP. Local accidents in dental implant surgery: prevention and treatment. Int J Periodontics Restorative Dent 2009;29(3):325-31.
9. Del Castillo-Pardo de Vera JL, Lopez-Arcas Calleja JM, Burgueno-Garcia M. Hematoma of the floor of the mouth and airway obstruction during mandibular dental implant placement: a case report. Oral Maxillofac Surg 2008;12(4):223-6.
10. Lee CY. Brisk, prolonged pulsatile hemorrhage during the sinus graft procedure: a case report with discussion on intra-operative hemostatic management. Implant Dent 2010;19(3):189-95.
11. Jo J.H, Kim S.G, Oh JS. Hemorrhage related to implant placement in the anterior mandible. Implant Dent 2011;20(3):e33-7.
12. Kalpidis CD, Konstantinidis AB. Critical hemorrhage in the floor of the mouth during implant placement in the first mandibular premolar position: a case report. Implant Dent 2005;14(2):117- 24.
13. de Souza JG, Schuldt Filho G, Pereira Neto AR, Lyra HF, Bianchini MA, Cardoso AC. Accident in implant dentistry: involuntary screwdriver ingestion during surgical procedure. A clinical report. J Prosthodont 2012;21(3):191-3.
14. Pingarron Martin L, Moran Soto MJ, Sanchez Burgos R, Burgueno Garcia M. Bronchial impaction of an implant screwdriver after accidental aspiration: report of a case and revision of the literature. Oral Maxillofac Surg 2010;14(1):43-7.
15. Worthington P. Injury to the inferior alveolar nerve during implant placement: a formula for protection of the patient and clinician. Int J Oral Maxillofac Implants 2004;19(5):731-4.
16. Alghamdi AS. Pain sensation and postsurgical complications in posterior mandibular implant placement using ridge mapping, panoramic radiography, and infiltration anesthesia. ISRN Dent 2013;2013:134210.
17. Park SH, Wang HL. Implant reversible complications: classification and treatments. Implant Dent 2005;14(3):211-20.
18. Yoon WJ, Kim SG, Jeong MA, Oh JS, You JS. Prognosis and evaluation of tooth damage caused by implant fixtures. J Korean Assoc Oral Maxillofac Surg 2013;39(3):144-7.
19. Oh E, Kraut RA. Effect of sinus membrane perforation on dental implant integration: a retrospective study on 128 patients. Implant Dent 2011;20(1):13-9.
20. Biafora M, Bertazzoni G, Trimarchi M. Maxillary sinusitis caused by dental implants extending into the maxillary sinus and the nasal cavities. J Prosthodont 2014;23(3):227-31.
21. Chrcanovic BR, Custodio AL. Mandibular fractures associated with endosteal implants. Oral Maxillofac Surg 2009;13(4):231- 8.
22. Boffano P, Roccia F, Gallesio C, Berrone S. Pathological mandibular fractures: a review of the literature of the last two decades. Dent Traumatol 2013;29(3):185-96.
23. Lauc T, Kobler P. Early Post-Operative Complications in Oral Implantology Coll Antropol. 1998;22:251-7.
24. Sakka S, Coulthard P. Implant failure: etiology and complications. Med Oral Patol Oral Cir Bucal 2011;16(1):e42-4.
25. Baqain ZH, Moqbel WY, Sawair FA. Early dental implant failure: risk factors. Br J Oral Maxillofac Surg 2012;50(3):239-43.
26. Nam KY, Kim JB. Treatment of dental implant-related maxillary sinusitis with functional endoscopic sinus surgery in combination with an intra-oral approach. J Korean Assoc Oral Maxillofac Surg 2014;40(2):87-90.
27. Kadkhodazadeha MA, R. A New Classification for the Relationship between Periodontal, Periapical, and Peri-implant Complications. Iranian Endodontic Journal 2013;8(3):103-8.
28. Armas J, Culshaw S, Savarrio L. Treatment of peri-implant diseases: a review of the literature and protocol proposal. Dent Update2013;40(6):472-4.
29. Singh P. Understanding peri-implantitis: a strategic review. J Oral Implantol 2011;37(5):622-6.
30. Vaidya S, Khalikar A, Dange S, Desai R. Complications and their Management in Implantology. Int J Protshodont Restor Dent 2012;2(4):150-5.
31. Dahlin C, Nikfarid H, Alsen B, Kashani H. Apical peri-implantitis: possible predisposing factors, case reports, and surgical treatment suggestions. Clin Implant Dent Relat Res 2009;11(3):222- 7.
32. Penarrocha-Diago M, Boronat-Lopez A, Garcia-Mira B. Inflammatory implant periapical lesion: etiology, diagnosis, and treatment--presentation of 7 cases. J Oral Maxillofac Surg 2009;67(1):168-73.
33. Al-Quran F.A, Rashan B.A, Al-Dwairi Z.N. Management of dental implant fractures. A case history. J Oral Implantol 2009;35(4):210-4.
34. Mendonca G, Mendonca DB, Fernandes-Neto AJ, Neves FD. Management of fractured dental implants: a case report. Implant Dent 2009;18(1):10-6.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License