IJCRR - 10(17), September, 2018
Pages: 01-05
Date of Publication: 10-Sep-2018
Print Article
Download XML Download PDF
Efficacy of Steroid and Proton Pump Inhibitors in Patients Undergoing Tonsillectomy \? A Comparative Study
Author: Vijay Sundaram, Satya Prabhakarrao, Akhila
Category: Healthcare
Abstract:Introduction: Advancement of technology has affected the surgical methods of tonsillectomy for reaching desired benefits. This study aims to find a practical, economical and pragmatic way in managing post-operative morbidity with respect to tonsillectomy. Materials and Methods: Patients were randomly divided into two groups \? Group A and Group B. Group A received Injectiondexamethasone, while Group B received oral pantoprazole. Post-operatively patients were assessed on pain, incidence of haemorrhage and wound healing on POD 0, 1, 7 and 14. Results: Group A had comparatively less pain on POD 0 and POD 1, but over the long term both groups didn't show any significant difference. Both groups didn't show much difference in regards to healing of tonsillar fossa. Incidence of Secondary haemorrhage (2%) and Reactionary haemorrhage (4%) were seen in Group A, but no incidence of haemorrhage was recorded in Group B. Discussion: Tonsillectomy as a surgical procedurehas evolved over the years.our study tookin to account two pharmacological agents which is administered,works and acts by radically different approach in which most potent,economical with fewer side effect was found to be Dexamethasone. Conclusion: The results concluded that there was no significant statistical difference between the two drugs in alleviating postoperative pain, haemorrhage and wound healing.
Keywords: Tonsillectomy, Post-operative, Pain, Haemorrhage, Healing
Full Text:
The first tonsillectomy was reported by a Roman Physician Celsus about 2000 years ago. Tonsillectomy is one of the most common otolaryngologic surgical procedure done all over the world.
Advancement in technology have affected the surgical methods of tonsillectomy for the reaching the desired benefits. This helps in reducing the operative time, intraoperative blood loss, post-operative pain and prolonged morbidity.
A variety of methods have been attempted, with the aim of reducing the postoperative pain associated with tonsillectomy such as lasers, radio-frequency, coblation, bipolar etc. Apart from instrumentation physicians have over half a century studied the pathology behind the post-operative pain and the other morbidities associated with tonsillectomy.
In this context, my study aims to find a practical, economical and pragmatic way in managing post-operative morbidity with respect to tonsillectomy. The two drugs before mentioned have radically different ways of approaching the problem, yet the goal remains the same.
Materials and Methods
Study Design
-
Prospective, comparative study.
-
Setting: Conducted in the department of ENT and Head & Neck surgery in NRI Medical College and General Hospital from January 2016 to January 2018
-
Sample size: Study conducted on 100 patients (50 in each category)
Inclusion Criteria
Exclusion criteria
-
Children under 18 years of age
-
Patients with Peritonsillar abscess
-
Immuno-deficient patients
-
Other indication of tonsillectomy including as a part of UPPP or Styloidectomy
-
Acute infection
-
Tumours of tonsils
-
Co- morbid conditions (hypertension, cardiac disease, diabetes mellitus, bronchial asthma
Study Group
Patients were randomly divided into two groups: Group A and Group B
-
Group A : 50 patients received Inj. Dexamethasone 0.5 mg/kg (maximum 8mg) before intubation and on POD 1 after a period of 24 hours
-
Group B: 50 patients received orally pantoprazole 40mg O.D for 2 weeks prior to the tonsillectomy. No steroids are given to this group.
Methodology
-
Cases selected according to the inclusion criteria will be subjected to detailed history and clinical examination
-
Patients will be randomly selected into 2 groups. One receiving Steroids & one receiving proton pump inhibitors.
-
Pre-operative investigations like haemoglobin percentage, total count, differential count, bleeding time, clotting time, prothrombin time, partial thromboplastin time, international normalised ratio, blood grouping & typing, and urine routine were performed
-
Standardization of Surgical procedure:
-
Intra-operative Assessment:
-
Post operatively patients will be assessed on pain and wound healing
-
Follow up on Post-operative day 0,1,7 and 14 from the date of surgery
-
At POD 0
-
At POD 1
-
At POD 7
-
At POD 14
-
Post-operative pain is assessed by visual analogue scale
The patients were discharged and called for follow up at the end of 1st week and 2nd week from date of surgery to assess the tonsillar fossa.

Tonsillar fossa was assessed by calculating the rate of healing, as determined by size of post tonsillectomy slough. The size of the post tonsillectomy slough was taken as an indication of the rate of healing process. Five grades of healing are considered: 0, 25, 50, 75 and 100 per cent, according to the size of the slough in comparison with the areal size of the original post-operative bed. (26), where 0% represented a bed completely covered with slough and 100% represented a totally healed bed. The lower grade was selected in case of inequality between both sides.
All patients were monitored closely in post-operative period to check for any eventuality of bleeding with respect to the laterality, quantum of bleed and their subsequent management.
The data obtained from both groups was compared and statistically analysed.
Results
A total of 100 patients were included in the study, with 50 patients in each group. They were divided into 2 groups as Group A and Group B based on blind randomization. Patient in group A received steroids and patients in Group B received Proton Pump inhibitor. All patients were assessed for post-operative pain, tonsillar fossa healing and incidence of haemorrhage. The data collected were tabulated and statistically analysed in consultation with a qualified statistician.
Statistical Analysis
-
Mean and standard deviation were estimated from the sample for each study group.
-
Student ‘t’ test and chi-square was applied to find the level of significance between Group A and Group B
-
In this study p<0.05 was considered as the level of significance.
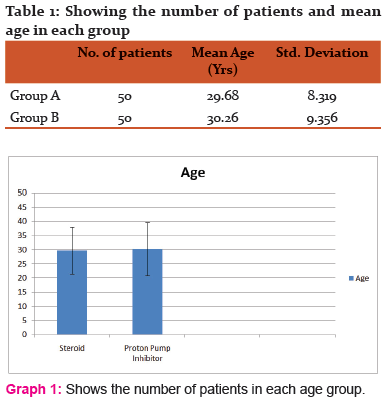
Age Distribution
There were a total of 100 patients included in this study with 50 patients in each group. The mean age in Group A was 29.68 years and that in Group B was 30.26 years.
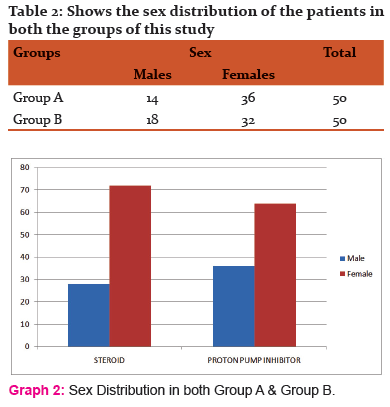
Sex distribution
There were 14 males and 36 females in Group A & 18 males and 32 females in Group B.
Post Op Pain Score
Post-operative pain scores was charted on day 0, day 1, day 7, day 14 using visual analogue scale in which 0 indicates no pain and 10 very severe pain.
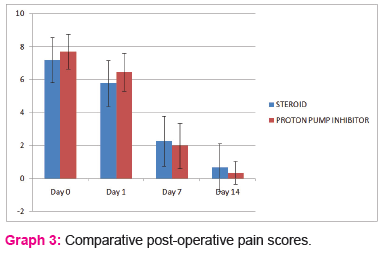
Pain score at Day 0
-
The mean pain score during post-operative day 1 in Group A was 7.18 and 7.70 in Group B
-
The standard deviation in Group A is 1.380 and 1.055 in Group B
-
The P-value is 0.03 and is statistically significant
-
Group A had comparatively les pain on POD 0
Pain score at Day 1
-
The mean pain score in Group A was 5.78 and in Group B it was 6.46
-
The standard deviation in Group A is 1.389 and in Group B it was 1.147
-
The p-value was 0.004 and is statistically significant
-
Group A had comparatively less pain on POD 1
Pain score at POD 7
-
The mean pain score in Group A was 2.28 and in group B it was 1.98
-
The standard deviation in Group A was 1.512 and in group B it was 1.378
-
The p-value was found to be 0.392 which is statistically insignificant
-
At day 7, there is no significant difference in the pain score between the two groups
Pain score at POD 14
-
The mean score in Group A was 0.66 and in Group B it was 0.34
-
The standard deviation in group A was 1.451 and in Group B it was 0.688
-
The p-value was found to be 0.201 which is statistically insignificant
-
At day 14, there is no significant difference in the pain score between the two groups.
-
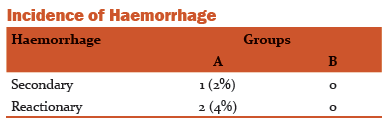
The incidence of secondary haemorrhage in group A is 2% and that of Reactionary haemorrhage is 4%. Where as in Group B no episode of neither Reactionary or Secondary haemorrhages was recorded.
-
The p-value is found to be .213 and is statistically insignificant
-
Hence there is no significant difference in the incidence of haemorrhage between the two groups.
Healing of Tonsillar Fossa
Tonsillar fossa was assessed by calculating the rate of healing, as determined by size of post tonsillectomy slough which is done at the end of Day 0, 1, 7 and 14
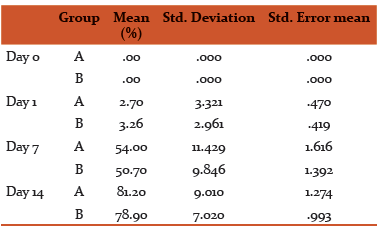
During POD 0, the mean healing percentage in both Group A and Group B was 0%
-
The standard deviation was also found to be .00 in both the groups
-
The p-value was found to be 1.000, which is statistically insignificant.
-
At the end of POD 0, there was no significant progress in healing in either Group A or B.
-
At POD 1, the mean healing percentage in group A was found to be 2.7% and in Group B it was found to be 3.26%
-
The standard deviation in Group A was 3.321 and in Group B it was found to be 2.961
-
The p-value was found to be .241, which is statistically insignificant
-
At the end of POD 1, there was no significant progress in healing in either Group A nor B
-
At POD 7, the mean healing percentage was 54% in Group A and Group B it was 50.7%
-
The standard deviation in Group A as 11.429 and in Group B it was found to be 9.846
-
The p-value was found to be .133
-
At the end of POD 7, there was no significant progress in healing in either Group A nor B
-
At the end of POD 14, the mean wound healing was found to be 81.2% in Group A and in Group B it was found to be 78.9%
-
The standard deviation in group A was 9.010 and in Group B it was found to be 7.020
-
The p-value was found to be .110, which is statistically insignificant
-
At the end of POD 14, there was no significant progress in healing in either Group A nor B

Discussion
Tonsillectomy as a surgical procedure has evolved over the years. It is the commonest surgery performed in children by Otolaryngologists.
Many types of instrumentation and different techniques have been attempted and published over the two centuries.
Our study is an attempt to compare two pharmacological agents: Dexamethasone and pantoprazole and analyse the clinical outcome in managing morbidities associated with post-tonsillectomy patients. A prospective single centered study encompassing hundred patients divided in two distinct groups. Group A was administered Inj. Dexamethasone and group B was administered pantoprazole per orally. At the end of the study we analysed patients in both the groups for wound healing, post-operative pain and incidence of reactionary/secondary haemorrhage. Patients were randomly placed in both the groups. The mean age group and sex distribution in both the groups were comparable. The mean age in group A was 29.68 and the mean age in Group B was 30.26. There were fourteen males and thirty six females in Group A, whereas there were eighteen males and thirty two females in group B. Majority of the patients in the study were in the 18-29 age group (56%), followed by 30-40 years (36%) and then above forty (8%).
Our study took into account two pharmacological agents, which is administered, works and acts by radically different approach. Steroid usage in tonsillectomy has been studied thoroughly for close to forty years since the seminal paper by Papangelou in 1972[3]. In 1975, Anderson et al [4] did a double-blinded study where in 165 patients were injected with depo-steroid or saline into the tonsillar fossae immediately after tonsillectomy. Multiple studies over a period of time tried and tested various steroid agents. Of them the most thoroughly studied, most potent, economical with fewer side effect was found to be Dexamethasone.
All the patient kept in the study were selected for elective tonsillectomy by the classical dissection & snare technique. Patients allotted in group B were advised regular medication with oral Pantoprazole two weeks prior to surgery. The patients were hospitalized for surgery after 2 weeks. A clinical trial done by Carissa J Wentland used omeprazole for a period of 4 weeks prior to surgery. Upon admission, intravenous pantoprazole administration was stopped. Both groups received Inj. Ranitidine at the rate of 50mg I.V. BD pre & post operatively. Haemostasis was secured by bipolar cauterization in all participants of the study. Both groups A & B received the same antibiotics and analgesics as per standard dosage. The antibiotic used in the study was Amoxicillin-clavulanic acid and the analgesic used was paracetamol. Both antibiotic and analgesic agent was administered via intravenous route during their hospital stay. Upon discharge drugs were advised to be taken in per orally.
Patients of both the group were evaluated after surgery POD-0, POD-1, POD-7 & POD-14. Our study focused on three major aspects, namely: post-operative pain, wound healing and incidence of reactionary/secondary haemorrhage. Pain score were recorded using a visual analogue score, where in 0 inferred no pain and 10 inferred severe pain. Measuring the amount of slough in the tonsillar fossa assessed wound healing. The Visual Analogue Scoring (VAS) system of quantifying pain was utilized in studies done by Stewart et al.
Managing immediate post-operative pain can very well increase post-operative oral intake and can subsequently bring down prolonged hospitalization which as per studies done by Brown et al has shown as much as 14% of post tonsillectomy patients require repeat or prolonged hospitalization. Post operatively group A tended to have better oral intake during the immediate postoperative period. However the average hospital stay for both group A and B when compared were not statistically significant. Dexamethasone suppresses the postoperative increase in circulating levels of beta-endorphin. Tissue injury-induced acute inflammation plays a significant role in the genesis of postoperative pain. The analgesic property of corticosteroid may be due to their inherent anti-inflammatory action.
Wound healing was assessed by measurement of the amount of slough in the tonsillar fossa. At the end of day 0, hardly any healing was noticed in both the groups. On comparing the healing rate at the end of day 0, 1, 7 and 14, we found no statistical significance when it came to both the groups. This finding concurs with the studies done by volket al.
During the period of study two patients presented with reactionary haemorrhage (2%) and one patient presented with secondary haemorrhage (1%). All three cases were seen in Group A. None of the patients in Group B presented with haemorrhage post-operatively.
Conclusion
-
Patients administered with dexamethasone immediately before intubation and after twenty four hours postoperatively showed significant reduction of pain in the immediate postoperative period.
-
Both Steroid (dexamethasone) and PPI (pantoprazole) had no significant advantage in pain management by the end of first and second week, post operatively.
-
Patients in both the groups had no significant influence in post-operative wound healing.
-
Incidence of reactionary & secondary haemorrhage in both groups was statistically insignificant.
-
Patient administered with dexamethasone had better oral intake compared the group administered with pantoprazole.
-
Proton pump inhibitors (pantoprazole) did not have a significant advantage over steroid group in pain management.
-
There is a need for more such evidence based studies in future that would help in analysing the data comparable to this study.
References:
-
Curtin JM. The history of tonsil and adenoid surgery. Otolaryngol Clin North Am. 1987; 20(2): 415-419
-
Timms MS, Temple RH. Coblation tonsillectomy: A double blind randomized controlled study. J. LArungolOtol 2002; 116:450 – 2
-
Papangelou, L. (1972), Steroid therapy in tonsillectomy. The laryngoscope, 82: 297 – 302
-
Anderson HA, Rice BJ, Cantress RW. Effects of injected deposteroid on post tonsillectomy morbidity: a double blind study. Arch Otolaryngol 1975; 101:86-8.
-
Sayaka Suzuki, MD, Hideo Yasunaga, MD, PhD; Hiroki Matsui, MPH; HiromasaHorigucki, PhD; Kiyohide Fushimi, MD PhD; Tatsuya Yamasoba, MD, PhD: Impact of Systemic Steroids on Posttonsillectomy Bleeding Analysis of 61 430 Patients using a National Inpatient Database in Japan: JAMA Otolaryngology – Head & Neck Surgery October 2014
-
Steward DL, Grisel J, Meinzen-DerrJSteward: Steroids for improving recovery following tonsillectomy in childeren (review) : Cochrane library
-
Mohammed Shakkel, Aaron Trinidale, Ahmed Al Adhami: Intraoperative dexamethasone and risk of secondary haemorrhage: Journal of otolaryngology –Head & neck surgery vol 39, no 6 (December) 2010
-
Hargreaves K.M., Schmidt E.A., Mueller G.P. et al. (1987) Dexamethasone alters plasma levels of beta-endorphin and postoperative pain. Clin. Pharmacol. Ther. 42, 601-607
-
Mark vs Volk, MD, DMD, Pierre Martin, MD Linda Brodsky, MD. John F. Stnievich, M: The effects of preoperative steroids on tonsillectomy patients: Otolaryngology –Head and Neck surgery October 1993.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License