IJCRR - 9(21), November, 2017
Pages: 58-63
Print Article
Download XML Download PDF
Study of Various Histopathological Patterns in Prostate Biopsy
Author: Mital Yadav, Hemina Desai, Hansa Goswami
Category: Healthcare
Abstract:Introduction: Diseases of prostate gland are important source of morbidity and mortality in male patients. The spectrum of diseases consists of inflammatory conditions, nodular hyperplasia, malignancy etc. The risk of diseases increases with age. Prostate biopsy is essentially a test which detects cancer and other benign conditions of the prostate in patients who have specific indications for it. Other modalities of diagnosis also have been developed, comprising of radiological modalities and prostatic biomarkers. However, biopsy with histopathological examination is the gold standard for the final diagnosis.
Aims and Objective: To study various histopathological patterns in Transurethral resection of prostate(TURP) and needle biopsy of prostate, including benign prostatic hyperplasia(BPH), prostatitis (identifying type and grade of inflammation),incidental detection of carcinoma prostate and confirmation of diagnosis of clinically suspected carcinoma with application of modified Gleason system for grading.
Materials and Methods: Total 100 cases of prostatic lesions including transurethral resection of prostate(TURP) and needle biopsy were evaluated in this study. The received specimens were fixed in 10% neutral buffered formalin and routine paraffin processing followed by hematoxyline and eosin staining was done. All the specimens were analysed with following parameters: type of specimen, age of patient, histopathological pattern and final diagnosis.
Results: In total 100 cases of present study, the most common age group presenting prostatic lesions was 61-70 years. The youngest patient presenting with prostatic lesion was 45 years age, and oldest was of 85 years of age. In this, various histopathological patterns observed were- Benign prostatic hyperplasia (BPH)in 45%,benign prostatic hyperplasia (BPH)with co-existing chronic prostatitis in 10%, granulomatous prostatitis 1% (single case),acute prostatitis 3% and acute on chronic prostatitis 6%.Less frequent finding were benign prostatic hyperplasia (BPH)with basal cell hyperplasia 1%,benign prostatic hyperplasia (BPH)with squamous metaplasia 2%,benign prostatic hyperplasia (BPH)with clear cell changes 3% and some of biopsy show only stromal tissue with hyperplasia in 4%.We reported 7 cases of adenocarcinoma prostate with application of modified Gleason grading system.
Conclusion: Benign lesions are more common than malignant lesions. Among the histological patterns of prostatic lesions, benign prostatic hyperplasia (BPH)is predominant type. It is necessary to study all prostate biopsy [Transurethral resection of prostate(TURP)and needle] in order to identify premalignant lesions, proliferative activity, and grade of inflammation. Histopathological diagnosis and grading plays a definitive role in the management of prostatic cancer.
Keywords: Transurethral resection of prostate (TURP) and Needle biopsy, Benign prostatic hyperplasia(BPH), Prostate Carcinoma
Full Text:
Introduction:
The prostate gland is the pear shaped glandular organ that weighs up to 20 gms1. Prostate is fibromusculoglandular organ encircling the neck of the urinary bladder. The prostate is an exocrine gland and forms a significant component of seminal fluid. Histologically it consists of glands lined by basal cuboidal cells and inner secretory columnar cells (double layered)1. Most patients of benign lesions present with complaints related to micturition and incontinence. Of the diseases which affects the prostate the most frequently encountered in clinical practice are benign prostatic hyperplasia (BPH), prostatic cancer and prostatitis2.
Benign prostatic hyperplasia is an extremely common condition in men over the age of 50 years and shows remarkable racial and geographical variations in incidence and mortality3. The clinical incidence of this disease is only 8% during the 4th decade, but it reaches 50% in the 5th decade and 75%in the 8th decade1.
Benign prostatic hyperplasia (BPH)is not premalignant lesion for the prostatic cancer but it may be related to prostate cancer arising in transition zone (Difenbach et al., 2002)4. Non-specific granulomatous prostatitis is noticed occasionally in prostate specimen. It was first described by Tanner and Mc Donald in 1943, who reported an incidence of 3.3% of granulomatous prostatitis in inflammatory lesions. Recently premalignant lesions have become defined, largely as a result of advances in technology.
Carcinoma of prostate is most common internal malignancy among men in United State and is responsible for 10% of cancer deaths 5.In India, prostate cancers constitute about 5% of all cancers in male5,6. Screening of prostatic lesions constitute prostate specific antigen, digital rectal examination, and transrectal ultrasound, but biopsy remains the gold standard diagnostic tool for final diagnosis. Prior to the PSA era, up to 27% of prostate cancers were detected incidentally at the time of transurethral resection of prostate(TURP)7. The modified Gleason's system appears better to predict progression -free survival after radical prostatectomy than the original Gleason's system did.
Material and methods:
The study was conducted in the Department of Pathology, B.J Medical College, civil hospital - a tertiary level hospital of Ahmedabad. The study period was from April 2017 to June 2017 and prostatic specimen data were collected retrospectively from archives of histopathology register. From April 2017 to June 2017 a total of 100 transurethral resection of prostate(TURP) and needle biopsy were evaluated. The received specimens were fixed in 10% neutral buffered formalin and routine paraffin processing followed by hematoxyline and eosin staining was done. All the specimens were analysed with following parameters: type of specimen, age of patient, histopathological pattern and final diagnosis. The slides were examined under light microscope, and Various histopathological patterns were studied in all cases and were classified with reference to age. Following histopathologic assessment, the tumors were classified according to WHO recommendation, and histologic grading was done using modified Gleason's system.
Result:
In this study a total of 100 prostate specimens were studied which were received between April 2017 to June 2017 in the histopathology section of department of Pathology in B.J. Medical College, Civil hospital, Ahmedabad. Of the 100 specimens 47(47%) were transurethral resection of prostate(TURP)specimens and 53(53%) needle biopsy specimens.
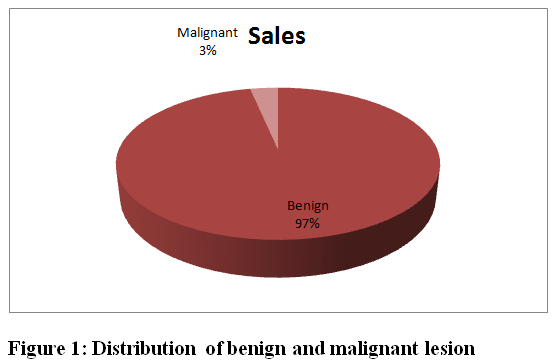
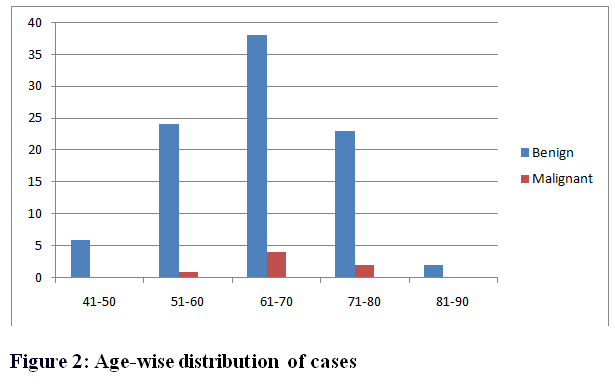
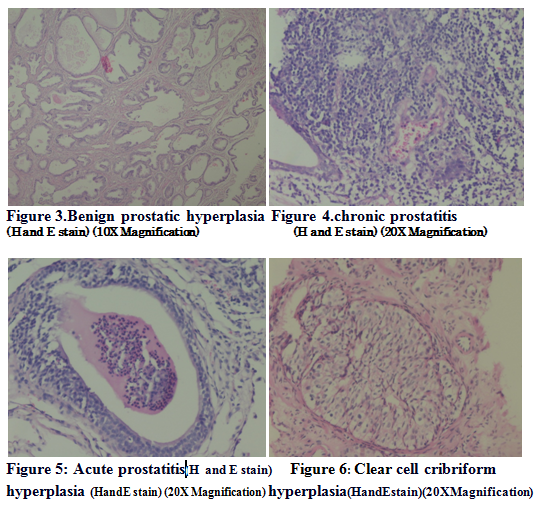
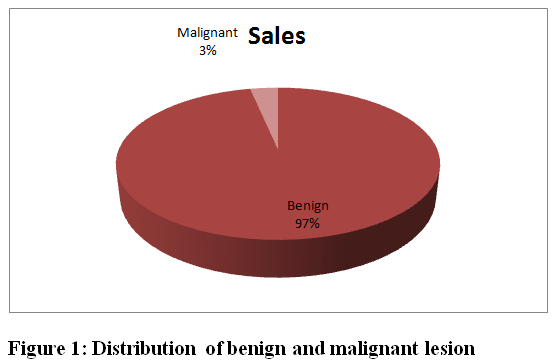
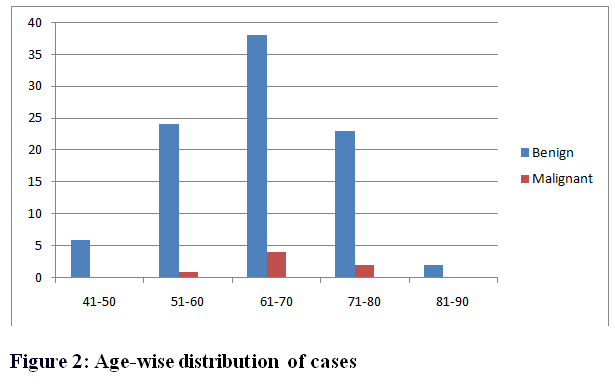
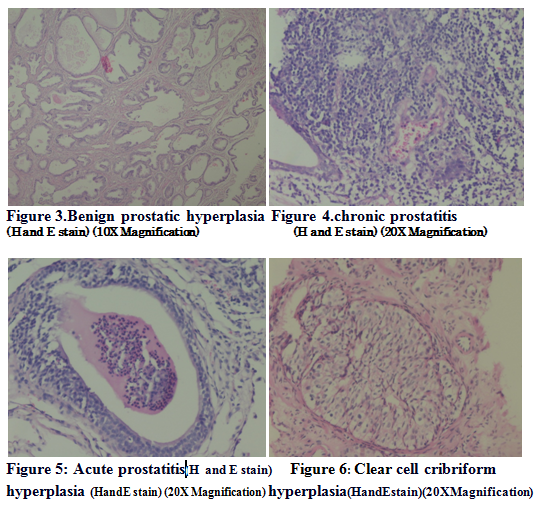
All prostatic specimens were broadly classified into benign 93(93%) and malignant 7(7%)[figure1]. Maximum cases of benign prostatic hyperplasia( BPH )(38) were seen in the 61-70 years age group[Table 1and figure 2]. A glandulostromal pattern of hyperplasia(72%)was the most frequent histological pattern which occurred. Stromal pattern of hyperplasia (4%) was less common.In this 45(45%) were benign prostatic hyperplasia (BPH) only [Figure 3]. Benign prostatic hyperplasia (BPH) with co-existing chronic prostatitis10(10%)[Figure 4], acute on chronic prostatitis 6(6%), acute prostatitis 3(3%)[Figure 5] and granulomatous prostatitis 1(1%)[Table 2]. In this study we reported one (1%) case of granulomatous prostatitis which showed granulomas with giant cells; however, Ziehl Nelsen staining was negative for AFB, and was labeled as non specific.
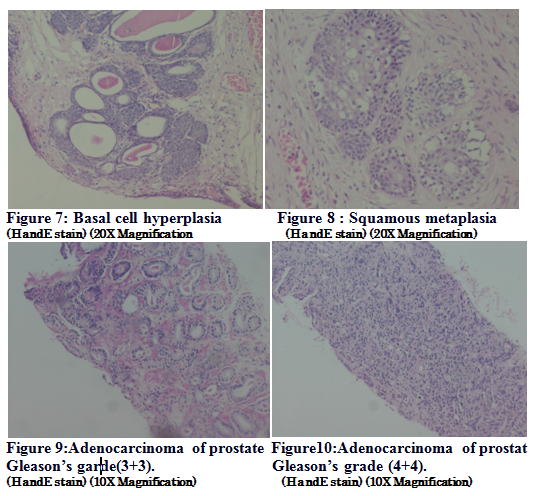
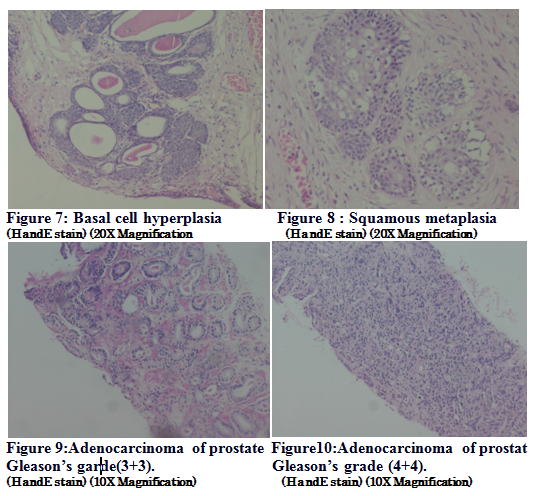
Less frequent finding was benign prostatic hyperplasia (BPH) with clear cell cribriform hyperplasia 3(3%)[Figure 6], benign prostatic hyperplasia (BPH) with basal cell hyperplasia 1(1%)[figure 7], benign prostatic hyperplasia (BPH) with squamous metaplasia 2(2%)[Figure 8].
We reported 7 cases of adenocarcinoma prostate with modified Gleason score. Histopathology of biopsy received showed single, separate, much more variable glands, closely packed but irregularly separated, ragged and poorly defined edge (Gleason's grade 3)[Figure 9]. Second most predominating pattern is fused glandular, cribriform pattern and hypernephroid (Gleason's grade 4) [Figure 10]. The most common predominant grades observed in this study were grade 3 and grade 4. The most common score obtained was 6 in 4 cases out of the total 7 adenocarcinoma cases.
Discussion:
A retrospective study of 100 cases of prostate biopsy were done, result were noted and comparison with other studies were undertaken as follows:
.
Age:
Lesions of prostate are extremely common over the age of 50 years. The clinical incidence of this disease is only 8% during the 4th decade, but it reaches 50% in the 5th decade and 75%in the 8th decade1. Benign prostatic hyperplasia (BPH)and carcinoma of the prostate are increasingly frequent with advancing age8.
In present study, age group affected with prostatic pathology was 45-85 years. Maximum cases of benign prostatic hyperplasia (BPH) (38) were seen in the 61-70 years age group similar to Matapurkar et al9. Kim KB et al. had more cases(44) in 71-80 age group10. Malignant lesions encountered predominantly in age group 61-70 years that are similar to Sharma et al11.
Benign and malignant:
Benign prostatic hyperplasia (BPH) and adenocarcinoma are the two most common conditions affecting prostate gland.
In present study malignant cases were7 (7%), and benign cases were 93 (93%) with ratio 1:14 approximately. In present study, the predominant lesion was benign prostatic hyperplasia (BPH) (45%) similar to Neha Angurana's12 study (50.5%), followed by benign prostatic hyperplasia (BPH)with prostatitis (21%) and prostate cancer (7%), basal cell hyperplasia and cribriform clear cell hyperplasia was observed.
Microscopy and Histopathological patterns:
Benign prostatic hyperplasia: There is hyperplasia of glandular and stromal tissue with papillary buds, in foldings and cysts. In glandulostromal pattern-Proliferating glands and fibromuscular stroma were assessed to be roughly in equal proportion. While in Stromal pattern- The sections showed more stromal elements than glands or were made up almost entirely of stromal elements.
In present study, glandulostromal pattern of hyperplasia(72%)was the most frequent histological pattern which occurred. Stromal pattern of hyperplasia (4%)was less common .Our study was in agreement with study done by Zeenath Begum, Abdul Hakeem Attar, Mandakini B. Tengli, Mohammed Mateen Ahmed13 (8%) in respect that glandulostromal hyperplasia was most commonly noted.
Prostatitis: It shows inflammatory change with in prostate glands. Acute prostatitis:where there are neutrophils within acini and throughout stroma, intraductal desquamated cellular debris, stromal edema and hyperaemia. Acute prostatitis is rarely seen in surgical specimens. In present study acute prostatitis(3%)was observed. Chronic prostatitis:Chronic prostatitis is more common. Chronic inflammation typically involves the prostate in periglandular distribution and contains an admixture of plasma cells,lymphocytes and histiocytes. In present study Benign prostatic hyperplasia (BPH)with co-existing chronic prostatitis in 10(10%) cases was observed. Chronic prostatitis is most commonly observed in benign prostatic hyperplasia (BPH)which was also observed by Dr. Ashish Joshee, Dr. Kaushal C.L. Sharma (14) in their study14. Malakoplakia:Usually associated with bladder disease, may clinically mimic cancer, resulting in prostatic induration and a hypoechoic lesion seen on transrectal ultrasound. On microscopy it show Marked histiocytic infiltrate containing Michaelis-Gutmann bodies (calcospherites) that may resemble signet ring cells at frozen section15.
Granulomatous prostatitis: Most commonly diagnosed granulomatous process within the prostate is non specific. It is thought to represent an initially immune-mediated process accompanied by a reaction to the prostatic secretions released from obstructed ducts on microscopic examination-large nodular aggregate of histiocytes, epithelioid cells, lymphocytes, and plasma cells. Characteristically, granuloma formation are seen16.
In present study granulomatous prostatitis(1%) was observed. The incidence of non specific granulomatous prostatitis was 0.5% obsereved in Stillwell TJ, Engen DE, Farrow GM17 in their study.
Types of epithelial hyperplasia
Various hyperplastic lesions were observed like papillary, basal, cribriform. basal cell hyperplasia is usually seen in the transitional zone, but it may also occur in the peripheral portion of the gland. Microscopically it appears as small, solid nests of benign-appearing epithelial cells with a somewhat clear cytoplasm1. Cribriform hyperplasia is an uncommon and controversial form of hyperplasia1. In clear cell cribriform hyperplasia, cytoplasm of hyperplastic glandular cells often a clear1.
In present study benign prostatic hyperplasia (BPH)with basal cell hyperplasia 1(1%) and clear cell cribriform hyperplasia 3 (3%)was observed.
Types of metaplasia:
Squamous metaplasia can be seen at the periphery of infarcts, after TUR, as a result of hormonal manipulation, or sometimes with no obvious predisposing cause. In present study benign prostatic hyperplasia (BPH) with squamous metaplasia in 2(2%) cases was observed.
Carcinoma Prostate:
Carcinoma of prostate is the second most common malignancy in men, second only to lung cancers. Hormonal factors play important role in the development of prostatic carcinoma.5-10% of prostatic carcinoma have a genetic link. A higher incidence has been seen in males with a first degree relative being affected1.
Features favoring prostatic carcinoma:
Architectural: Infiltrative patterns, small glands, crowded glands.
Nuclear: Prominent nucleoli, enlargement, hyperchromasia, mitotic figures, apoptotic bodies.
Cytoplasmic:Amphophilic cytoplasm, sharp luminal border18.
In present study carcinoma prostate was identified incidentally in 7 (7%) i.e., 7 of 100 cases, close to previous study by Otto B et al.19where only 1.4% patients were found to have prostate cancer on pathology in prostate biopsy samples. Adenocarcinoma was the only histological type of cancer found in this study Adenocarcinomas were graded according to Gleason's system by taking into account morphological appearance of glandular cells and the glandular pattern. The most common predominant grades observed in this study were grade 3 and grade 4. The most common score obtained was 6 in 4 cases out of 7 adenocarcinoma cases. Vollmer20 had score 6 most common whereas Brawn et al21 had scores 6 and 7 in his study.
Conclusion:
We conclude that prostatic lesions are common in age group of 61-70 years. Benign conditions are more common than malignant conditions Among the histological types of prostatic lesions, benign prostatic hyperplasia (BPH) is predominant type, followed by benign prostatic hyperplasia (BPH) with prostatitis. It is necessary to reassess periodically all prostate biopsies carefully in order to identify premalignant lesions, proliferative activity, grade of inflammation. Efforts should be made to apply modified Gleason's system in case of adenocarcinoma of prostate to improve management .
Table 1: Age-wise distribution of cases:
|
|
Benign,n(%)
|
Malignant, n(%)
|
|
41-50
|
6
|
0
|
|
51-60
|
24
|
1
|
|
61-70
|
38
|
4
|
|
71-80
|
23
|
2
|
|
81-90
|
2
|
0
|
|
Total
|
93
|
7
|
Table 2: Distribution of Histopathological Patterns pattern:
|
Histopathological patterns
|
No. Of cases
|
Percentage
|
|
Benign prostatic hyperplasia (BPH)alone
|
45
|
45%
|
|
Benign prostatic hyperplasia (BPH)with chronic prostatitis
|
10
|
10%
|
|
Benign prostatic hyperplasia (BPH)with acute on chronic prostatitis
|
6
|
6%
|
|
Granulomatous prostatitis
|
1
|
1%
|
|
Benign prostatic hyperplasia (BPH)with acute prostatitis
|
3
|
3%
|
|
Stromal hyperpasia only
|
4
|
4%
|
|
Benign prostatic hyperplasia (BPH)with Clear cell hyperplasia
|
3
|
3%
|
|
Benign prostatic hyperplasia (BPH)with basal cell hyperplasia
|
1
|
1%
|
|
Benign prostatic hyperplasia (BPH)with squamous metaplasia
|
2
|
2%
|
|
Benign prostatic tissue
|
18
|
18%
|
|
Adenocarcinoma prostate
|
7
|
7%
|
|
Total
|
100
|
100%
|
References:
1. Rosai and ackerman's surgical pathology tenth edition.
2. Cotran RS, Kumar V, Robbins SI. Prostate. In: Cotran RS, Kumar V, Robbins SI (eds): Robbins Pathologic Basis Of Disease, 6th ed., Philadelphia: Saunders Co., pp. 1025-1034, 1994
3. Walsh Pc. Benign prostatic hyperplasia. In: Walsh Pc, Gittes RF, Perlmatter AD, Stamey TA (eds) : Campbell's Urology 5th ed., vol.2, Philadelphia : W.B. Saunders co., pp. 1248-1265, 1986
4.Difenbach MA, Dorsey J, Uzzo RG, Hanks GE, Greenberg RE and Horwitz E et al., (2002). Decision making strategies for patients with localized prostate cancer, Seminars in Urologic Oncology 20 52-62. Egevad L,
5. Consolidated Report of Population Based Cancer Registries 2001-2004:
Incidence and Distribution of Cancer. Bangalore (IND): Coordinating
Unit, National Cancer Registry Programme, Indian Council of
Medical Research; 2006.
6. Garg M, Kaur G, Malhotra V, Garg R. Histopathological spectrum of 364 prostatic specimens including immunohiostochemistry with special reference to grey zone lesions. Prostate Int 2013; vol 1 (4) : 146-151.
7. B. Tombal, L. de Visccher, J. P. Cosyn et al., Assessing the risk of unsuspected prostate cancer in patient with Benign Prostatic hypertrophy : a 13 years retrospective study of incidence and natural history of T1a-T1b Prostate cancers, BJU International, Vol. 84, no. p. 1015-1020, 1999.
8. A Josephine - ?2014, clinicopathological study of prostate biopsy,  2014 Journal of Clinical and Diagnostic Research.
2014 Journal of Clinical and Diagnostic Research.
9. Matapurkar BG, Taneja OP. Incidence of carcinoma prostate. Ind J of Cancer 1969 Sept 172-182.
10. Kim KB, Kim KS. A Histopathological observation on 48 cases of benign prostatic hypertrophy. Korean J Urol 1982; 23(8):30.
11. Sharma GC, Mathur SC, Sharma ML. Occult carcinoma in benign hypertrophy of prostate (Clinicopathological study of 100 cases). Ind J Surg 1972 April: 152-155
12. Neha angurana, pattern of prostrate diseases- a histopathological study in Jammu, international journal of basic and applied medical sciences issn: 2277-2103 (online)
13. Zeenath Begum, Abdul Hakeem Attar, Mandakini B. Tengli, Mohammed Mateen Ahmed , Study of Various Histopathological Patterns in Turp Specimens and Incidental Detection of Carcinoma Prostate, Indian Journal of Pathology and Oncology, October - December 2015;2(4);303-308
14. Dr. Ashish Joshee, Dr. Kaushal C.L. Sharma; The histomorphological study of prostate lesions, IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN:
15.Wagner D, Joseph J, Huang J, Xu H. Malakoplakia of prostate on needle core biopsy,a case report and review of the literature.s
16.Oppenheimer JR, Kahane, Epstein JI. Granulomatous prostatitis on needle biopsy, Arch pathol Lab Med 1997.
17.Stillwell TJ, Engen DE, Farrow GM. The clinical spectrum of granulomatous prostatitis: A report of 200cases.J Urol.1987;138:320-323.
18.Epstein, George J, Netto. Biopsy interpretation of the prostate, Forth edition.
19. Otto B et al. incidental prostate cancer in Transurethral Resection of the Prostate Specimen in moderate era. Advances in Urology 2014 ;4:1-4
20.Vollmer RT. Prostatic cancer and chip specimen: complete versus partial sampling. Hum Pathol 1986; 17:285-290. 18. Otto B et al. incidental prostate cancer in Transurethral Resection of the Prostate Specimen in moderate era. Advances in Urology 2014 ;4:1-4.
21. Brawn PN, Ayala AG, vonEschenbach AC, Hussey DH, Johnson DE. Histologic grading study of prostate adenocarcinoma: The development of a new system and comparison with other methods- A preliminary study. Cancer 1982; 49:525-532.
 2014 Journal of Clinical and Diagnostic Research.
2014 Journal of Clinical and Diagnostic Research.





 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License