IJCRR - 6(1), January, 2014
Pages: 95-100
Print Article
Download XML Download PDF
PRIMARY HYPERPARATHYROIDISM DUE TO BILATERAL PARATHYROID ADENOMA - A CLINICAL CASE REPORT
Author: Mousumi Mukhopadhyay, Sharmistha Chattopadhay, Sanghamitra Chakraborty, Swati Bhattacharyya, Soumika Biswas
Category: Healthcare
Abstract:Primary hyperparathyroidism is known by inappropriate secretion of parathyroid hormone that results in hypercalcaemia. The most common cause of primary hyperparathyroidism is solitary adenoma of the parathyroid followed by multiple adenoma, parathyroid hyperplasia and carcinoma, in that order. This paper describes the case of a fifty two year old man who presented with pain and swelling over multiple joints on trivial trauma( right elbow, right knee and left shoulder) against a backdrop of diverse symptoms like anorexia, nausea, weight loss, etc. of insidious onset over the past ten months. Detailed laboratory workup revealed hypercalcaemia (measured on more than one occasion) with concomitant hypophosphatemia, hypercalciuria, raised serum intact parathyroid hormone and elevated skeletal isoenzyme of serum alkaline phospatase. The causes of non parathyroid hypercalcaemia in the differential diagnosis were excluded by the serum 25 hydroxy vitamin D estimation which was found to be in the upper normal range. Finally, the diagnosis was clinched by the serum iPTH assay which is the most sensitive and specific test for parathyroid function. The histological picture was consistent with parathyroid adenoma. Subsequently, surgical resection of the parathyroid achieved normocalcaemia and the patient was discharged with bisphosphonates and calcium supplements.
Keywords: Primary Hyperparathyroidism, Adenoma, Hypercalcaemia
Full Text:
INTRODUCTION
Primary Hyperparathyroidism is known by inappropriate secretion parathyroid hormone that result in hypercalcemia. 1 The incidence of the disease is 0.1% in general population, females being affected more than males by a ratio 3:2. 2 The disease occurs most often due to solitary adenoma of parathyroid gland ( 80-85% of cases) and less commonly due to multiple adenoma and parathyroid hyperplasia (15%) parathyroid cancer being the rarest (<1%) 3 .Parathyroid adenoma are caused by mutations of DNA in certain parathyroid cells which confers survival advantage on a clone of cells – that undergo clonal expansion to produce adenoma.4 Half of the patients remain asymptomatic. The other half presents with a wide range of clinical features like fatigue, malaise, G.I disturbances, nephrocalcinosis, neuromuscular involvement etc.5As, many patients remain asymptomatic or present with protean clinical features, laboratory studies of biochemical parameters play an important role in diagnosis, supported by findings of radiological imaging studies. In the present instance a case of primary hyperparathyroidism in a 52 year old man presenting with fracture on trivial trauma being reported.
CASE REPORT
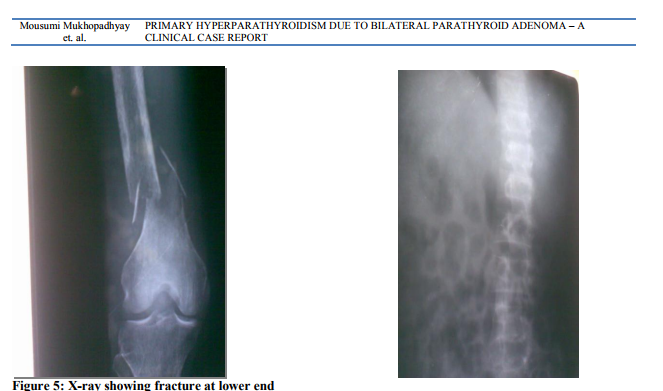
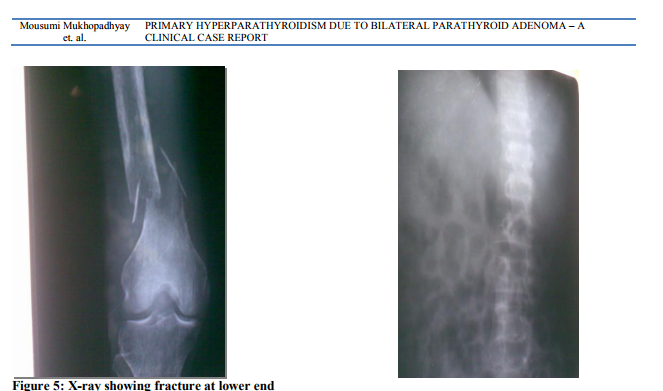
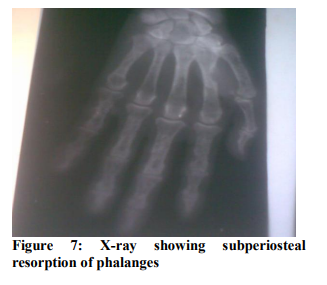
The 52 year old male patient reporting to a tertiary care institution complained of insidious onset of anorexia, nausea, vomiting, constipation and loss of weight for last ten months with swelling over multiple joints on trivial trauma for last two months. Subsequently lethargy, tiredness, muscle aches, depression and mental apathy that started interfering with his occupation. For the last two months, he developed pain and swellings over multiple joints (Right elbow, right knee and left shoulder) on trivial trauma which prompted him to seek medical advice (figure 1). The general examination revealed moderate degree of pallor. Any swelling or palpable lymph nodes in neck were conspicuous by their absence. The systemic examination of heart and lungs detected no abnormal findings; abdomen was non-tender, soft on palpation. Systemic examination of skeletal system indicated there was swelling of the Right elbow, right knee and left shoulder which were tender on palpation. Movement was also restricted about the above joints. The relevant laboratory investigations are detailed below. The hemoglobin was 8.3 g/dl of hemoglobin and total count 12,900 cells/cmm, the peripheral blood picture showed normocyctic, normochromic blood cells. The plasma glucose, serum urea and creatinine were within normal limits. Among the electrolytes, serum Na+ and K+ were 139mmol/L (136-145mmol/L) and 3.7mmol/L (3.5-5.5mmol/L).The total calcium adjusted for serum albumin (2.9 gm/dl) was 13.73 mg/dl and 14.73mg/dl on two different occasions while serum phosphate concentration was 2.2mg/dl (2.5-4.5mg/dl). The 24 hours urinary calcium was measured to be 1176mg (normal up to 300 mg/day on diet of unrestricted calcium). Serum intact parathyroid hormone (iPT) measured by ELISA was found to be 1842 pg/ml (10-65pg/ml).Parathyroid cell in parathyroid adenoma usually demonstrates abnormalities with a shift in their set point. This shift in their set point with non-suppressible component of PTH secretion leads to new steady state in which both PTH and serum calcium are higher than normal. Serum 25-OH vitamin D was also measured by ELISA and measured 57ng/ml (50-70ng/ml). In the hepatic enzyme profile, the most conspicuous change was noted in serum Alkaline Phosphatase levels at 887 U/L (53-128 U/L). The serum sample when incubated at 560C for 10 minutes and alkaline phosphatase was re-estimated to be 166U/L. Serum Protein electrophoresis and bone marrow examination excluded plasma cell dyscrasias or leukemia. The sonographic investigation of abdomen was within normal limit except for medullary tips calcification in both the kidneys (Figure 2). On sonography two hypoechoic well defined Space occupying lesion abutting both lobes of thyroid from posterior aspect. The Right sided SOL was about 3.6cmX 2.6cm (Figure 3) and left sided SOL about 1.5x1.1cm (Figure 4). No lymphadenopathy noticed along the great vessels of neck and the thyroid gland was within normal limit. The radiographs of various body parts suggested pathological fracture in right lower femur (Figure 5), the rarefaction of vertebra (Figure 6) and subperiosteal resorption of phalanges (Figure 7). After correction of anemia patient was treated surgically by resection of parathyroid gland. During surgery, 1X 1 cm mass involving left parathyroid gland was found. The superior left parathyroid gland was not found. A mass of 3X2 cm involving the right lower parathyroid gland extending up to the medial border and underneath the carotid sheath was found. No lymphadenopathy was found and dissection was done up to the ligament of Berry. Right upper parathyroid gland was found to be normal. The frozen section shows monomorphic population of round cells with almost uniform nucleus moderately eosinophilic cytoplasm arranged in sheets and trabecular pattern separated by broad fibrous band. No mitotic figures were found. This histopathology picture is consistent with parathyroid adenoma. The subsequent calcium after resection was 6.4 mg/dl and 3.4 mg/dl respectively. The patient was discharged with bisphosphonates 35mg once monthly and calcium supplements.
DISCUSSION
Among the multitude of homeostatic process in the body, one of the most tightly controlled is the metabolism of calcium. Still hypercalcemia is commonly encountered in clinical practice 6 and results when the flux of calcium into the extracellular compartment from skeleton, intestine or kidney is greater than its efflux.7 when hypercalcaemia is detected in a patient attending OPD --- primary hyperparathyroidism is the most probable cause. Diagnosis can be made by measuring laboratory parameters even in the backdrop of diverse symptoms or asymptomatic cases. Improvement in technologies have allowed laboratories to expand their role from measuring total calcium, phosphate and magnesium to other analytes such as intact PTH, Vitamin D metabolites etc.8 In the present instance hypercalcemia is established by measuring total calcium from serum calcium and albumin on more than one occasion with concomitant hypophosphatemia. The serum 25-OH is in the upper normal range which leads us to rule out causes of nonparathyroid hypercalcemia, as PTH stimulated the production of Vitamin D. of course the assay of iPTH, most sensitive and specific test for parathyroid function, provides the ultimate key to differential diagnosis of hypercalcemia. However, in developing countries the age group affected is about 20 years younger and presents mostly with renal and skeletal involvement.6 Moreover, documented vitamin D and calcium deficiency and altered dietary pattern with increased phosphate and phytate content suggests the etio-pathogenesis of skeletal involvement.7Certain laboratory findings also explain other pathological features associated with increased PTH. The high values of alkaline phosphatase which decreases considerably on exposure to higher temperature indicates the elevation of the skeletal isoenzyme of ALP which is heat sensitive. Skeletal involvement in a classical case of hyperparathyroidism presents with the following features of increased osteoclastic bone resorption associated with replacement of bone marrow by fibrovascular tissue as well as increased osteoblastic activity.8 The radiological findings of vertebra, phalanges further support the fact. Osteopenia due to decreased bone mineral density may also lead to fractures.9That fracture risk is increased in patients with Primary Hyperparathyroidism was also supported by a retrospective analysis of fracture incidence with disease between 1965 and 1992. Relative risk of fracture at vertebrae increases by 3.2 fold and distal forearm by 2.2.10 when the flux of calcium from the bone to the ECF becomes more than the amount of kidney can reabsorb, hypercalciuria develops which is evident in the present case.11 Though an urine sample collected in fasting state is best for detection in the present case (Ca2+ , iPTH, ALP all raised) points to the fact that calcium from demineralization is being excreted through kidneys. The patients need to undergo follow-up post-surgery with appropriate calcium replacement for 1 year as bone mineral density continues to increase 1 year post surgery
CONCLUSION
Thus in cases presenting with fracture on trivial trauma, calcium status needs to be measured. There after a systematic biochemical work up is required to clinch the diagnosis.
Abbreviations of terms used in the Case report:
1. iPTH – Intact parathyroid hormone.
2. DNA- Deoxyribonucleic acid
3. GI – Gastrointestinal
4. ELISA- Enzyme linked immunoabsorbant Assay
5. USG- Ultrasonography
6. ECF- Extracellular fluid
7. ALP- Alkaline phosphatase
8. SOL- Space occupying lesion
References:
REFERENCES
1. Bringhurst FR, Demay MB, Krokenberg HM : Hormones and Disorders of Mineral Metabolism : William Textbook of Endocrinology, Melmeds, Polonosky KS, Larsen PR, Krokenberg HM (eds) , 2012, 12ed, 1260 Philadelphia
2. Deshmukh, R. G.; Alsagoff, S. A. L.; Krishnan, S.; Dhillon, K. S.; Khir, A. S. M. (1998). "Primary hyperparathyroidism presenting with pathological fracture". Journal of the Royal College of Surgeons of Edinburgh 43 (6): 424–427.
3. Bilezikian, John P.; Silverberg, Shonni J. (2002). "Primary hyperparathyroidism: Epidemiology and clinical consequences". Clinical Reviews in Bone and Mineral Metabolism 1 (1): 25–34.
4. Bolland, M. J.; Grey, A. B.; Gamble, G. D.; Reid, I. R. (2004). "Association between Primary Hyperparathyroidism and Increased Body Weight: A Meta-Analysis". Journal of Clinical Endocrinology and Metabolism 90 (3): 1525.
5. "Endocrine Pathology". Retrieved 2009-05- 08.
6. Bile Zikian JP. Calcium and bone metabolism. In : Becker KL, Ed. Principles and Practice of Endocrinology and metabolism. Philadelphia: JD Lipincott, 1990: 398-569.
7. Jorde R, Bonaa HK, Sundsfjord J Primary hyperparathyroidism detected in a health screening: The Tromso Study. Journal of Clinical Epidemiology 2000; 53: 1164-9.
8. Health Hodgson SF, Kennedy MA. Primary Hyperparathyroidism: incidence, morbidity and potential impact in a community. NewEnglJMed 1980; 302:189_93.
9. WassifW, Kaddam I, Prentice M, Iqbal ST, Richardson A. Vitamin D deficiency and primary hyperparathyroidism presenting with repeated fractures.J Bone Joint Surg 1991:73- B:343-4.
10. Wengreen HJ, Munger RG, West NA et al Dietary protein intake and risk of osteoporotic hip fracture in elderly residents of Utab. J Bone Miner Res 2004: 19: 537-545
11. Gauger PG, Doherty GM. Parathyroid Gland. In: Townsend CM, Evers BM, Beauchamp RD, Mattox KL, editors. Sabiston Textbook of surgery. 17th ed. Philadelphia: Saunders/Elsevier;2004.p.1063-78.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License