IJCRR - 6(1), January, 2014
Pages: 06-20
Print Article
Download XML Download PDF
USE OF LOCKING PLATES IN FRACTURE MANAGEMENT
Author: Raza A., Kailash K., Mahalingam S.
Category: Healthcare
Abstract:The history of fracture management can be traced back to the prehistoric times. It was not until the late nineteenth and early twentieth century that operative treatments of fractures were contemplated. However operative treatment of fractures at that time was associated with devastating results secondary to infection with high morbidity and mortality. As a result, the mainstay of treatment of fractures remained traction and closed reduction within plaster of Paris. On the other hand, non-operative treatment of fractures was associated with the development of joint stiffness, disuse osteopenia and muscle atrophy, collectively described as „Fracture disease?. During 1950s, the Swiss AO group standardized the use of plating systems. The AO group revolutionized the concept of rigid stable internal fixation with early functional mobilisation which resulted in a positive impact on fracture disease. With time, surgeons started gaining more confidence in the operative management of fractures when better results were obtained while adhering to the principles of strict asepsis and using antibiotics. The article describes the use of modern locking plates in the management of fractures in different areas. Overall, the literature supports using locking plates for fixation of periarticular fractures of long bones, multifragmentary fractures of diaphysis and metaphysis and periprosthetic fractures. Locking plates are not the panacea for all type of fractures. As clinical experience with locking plate broadens, new indications and applications will emerge.
Keywords: Locking plate, Internal fixation.
Full Text:
INTRODUCTION
The history of fracture management can be traced back to the prehistoric times. Analysis of bones of Neolithic man shows both successful and unsuccessful attempts in fracture fixation [16]. It was not until the late nineteenth and early twentieth century that operative treatments of fractures were contemplated. Later, devices were developed that could be applied to the broken bone either externally or internally to hold the fracture and let it heal in the required position. External fixation was first attempted by Albin Lambotte in 1902 [49] and Gerhard Kuntscher developed his intramedullary nail in 1938. However operative treatment of fractures at that time was associated with devastating results secondary to infection with high morbidity and mortality. As a result, the mainstay of treatment of fractures remained traction and closed reduction within plaster of Paris. On the other hand, nonoperative treatment of fractures was associated with the development of joint stiffness, disuse osteopenia and muscle atrophy, collectively described as „Fracture disease?.During 1950s, the Swiss AO group standardized the use of plating systems [24]. The AO group revolutionized the concept of rigid stable internal fixation with early functional mobilization which resulted in a positive impact on fracture disease. With time, surgeons started gaining more confidence in the operative management of fractures when better results were obtained while adhering to the principles of strict asepsis and using antibiotics. The contribution by AO group in the understanding of fracture healing, management and internal fixation is undisputedly enormous.
Development of Locking plates
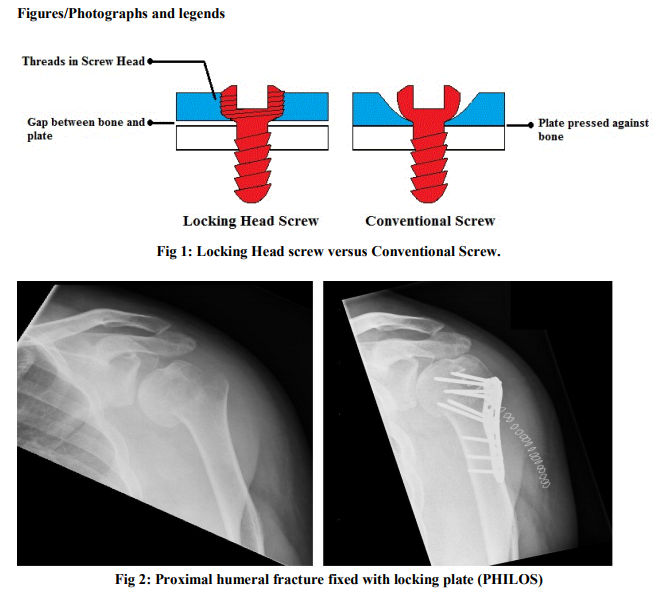
The fixation achieved by conventional plate-bone construct is based on friction between the plate and bone interface. As the plate is firmly pressed against the periosteum, it impairs the periosteal blood supply with subsequent poor and slower bone healing. With time surgeons and researchers recognised the importance of biological environment of the fracture. The principle of “Biological Internal Fixation” emphasized more flexible fixation to encourage the callus formation, with less precise direct reduction thus reducing surgical trauma [54]. As a result Zespol plates and Schuhli nuts were introduced to convert conventional plate into fixed-angle device with plate acting as internal fixator. Later, the point contact fixator (PC-Fix) and Less Invasive Stabilisation Systems (LISS) were developed by AO, which had even minimal contact areas on the bone with improved preservation of periosteal and endosteal blood supply [47]. Thus locking plates were developed to achieve biological internal fixation with relative stability, yet strong enough to allow early functional mobilisation.
How Locking Plates Work
Conventional plates owe their stability to firm contact with bone surface, and reducing this contact also reduces the stability of implant-bone construct. In order to maintain such low contact to allow for biological fixation and yet stay stable, locking plates are designed as „fixed angled devices?. „Fixed-angle device? means that when screws are placed in the plate and stress is applied, the angle between the plate and screws does not change. In order to achieve this, locking head screws were developed which can lock within the screw holes of the locking plate by virtue of their threaded heads. Once locked, these screws even under stress maintain their relative position with respect to the plate, thus providing both angular and axial stability. In a conventional plate, loosening of one screw renders instability by reducing the contact pressure between the plate and bone. Thus loosening of even one screw can potentially jeopardize the overall stability with rapid sequential loosening, as is seen in osteopenic and osteoporotic bones. This however is not seen in locking plates where stability is not based on interface friction as the plate-screw construct acts as a composite structure. Currently locking plates are being used for treating a wide variety of fractures. Let us briefly consider different areas of the body where these plates have been used while comparing them with other treatment modalities.
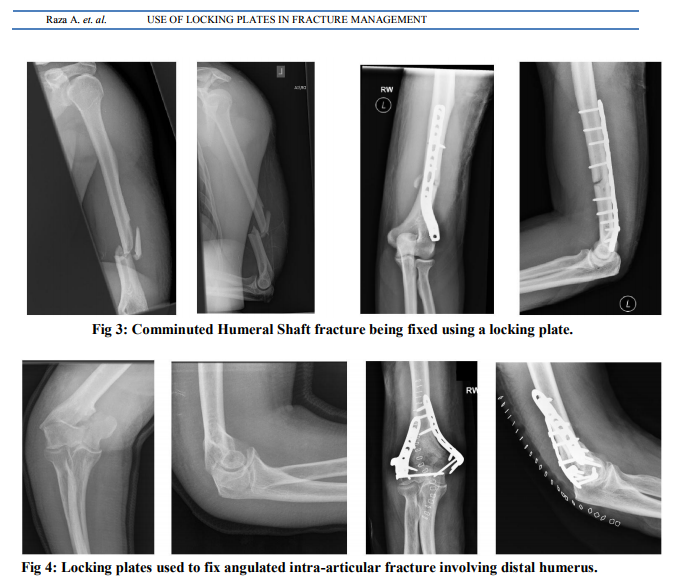
Proximal Humeral Fractures
Proximal humeral fractures are the third most common osteoporotic fractures after hip and distal radius with females having higher risk than men [5]. The large majority of these fractures are managed non-operatively as they are mostly stable and minimally displaced ( <1 cm ) [19]. Various biomechanical studies have compared PHILOS (Proximal Humeral Internal Locking System) and LCP-PH (Locking Compression Plate-Proximal Humerus) with intramedullary nails and other conventional plates. Overall, the locking plate-bone construct has always been found to be more stiffer in torsion and bending when cyclical loads are applied as shown by Edwards et al. [23] and Kralinger et al. [45]. A study performed by Fuchtmeier et al, however, showed that intramedullary implants were superior in bending and torsional stiffness than extramedullary implants [33]. It is important to emphasize that results were based on only five loading cycles leading to implant failure whereas in the human body implant-bone constructs are subjected to different types of load. Cyclical loading as tested by Edwards et al [23] and Kralinger et al [45] predominates in human function. Thus studies performed using cyclical loading are a more true representation of normal physiological loading conditions. Increased rigidity of the implant; although both biomechanically and theoretically attractive, has been attributed to the enblock cutout of the whole implant [65]. According to a systematic review, one major factor of re-operations was cut-out after loss of reduction. They recommended that the ideal elastic to rigidity ratio still needs to be determined in order to achieve the best outcome [65]. Operative fixations of proximal humeral fractures are not devoid of complications. It has been shown that the risk of osteonecrosis, neurovascular complications and deep infections are minimal when a fracture is fixed with indirect techniques using percutaneous wire fixation or intramedullary nailing. Fenichel et al.[31] and Keener et al. [43] have shown no occurrences of any of the above mentioned complications by percutaneous wire fixation. According to a recent systematic review and other studies, the overall incidence of AVN ranges from 4% to 11.1% when locking plates are used [29,51,63,65]. The incidence of deep infection was shown to be mean 2.2% and loss of reduction ranging from 3.7% to as high as 12.2%. Primary implant failure, an uncommon complication, was found to be 0.7% [65]. The intraoperative error of choosing incorrect length of the screws is the commonest complication with the use of PHILOS plate, which ranges from 2% to 17.9% [65]. This has also been confirmed by a prospective multicentre study done by Sudkam et al. [63].
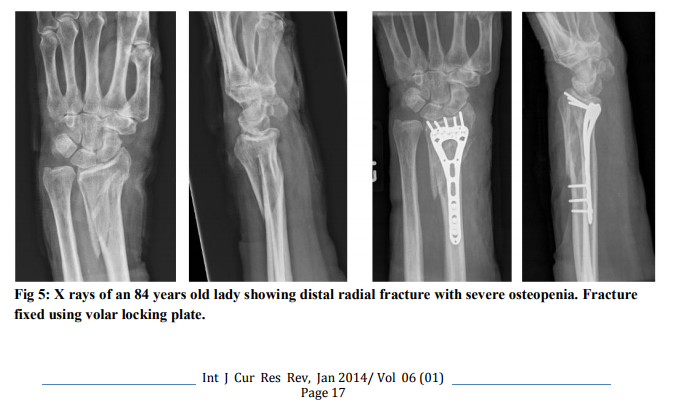
Humeral Shaft and Distal Humeral Fractures
The majority of humeral shaft fractures can be treated conservatively [12,58]. Conservative methods are associated with prolonged immobilisation and subsequent lengthy rehabilitation. Although conventional plating allows early mobilisation, it requires an extensive approach. This extensive approach can be detrimental to fracture healing and can cause iatrogenic nerve injury [20]. The use of an intramedullary nail has also been found to be associated with iatrogenic nerve injury along with high incidence of delayed union and shoulder pain [8,30]. Locking plates have been recommended to be used for comminuted fractures and osteopenic bones as they provide angular stability. In addition, these plates can be applied using a minimally invasive technique to avoid the complications associated with the extensive approach [1]. However, there is still a potential for iatrogenic nerve injury. In anterior approach, the injury to musculocutaneous nerve can be avoided by an extended distal incision with careful exposure of the nerve. In a cadaveric study, the author suggests to insert the distal locking screws by an open approach [2]. The radial nerve is most commonly injured in the spiral groove which can be avoided by using unicortical screws in the middle one third of the shaft of humerus. Distal humeral fractures constitute 2-6% of all fractures. The principle of treating distal humeral fractures involves anatomical reduction with primary stabilisation to allow early rehabilitation. These fractures are notoriously associated with stiffness even after short duration of immobilisation. Due to reduced cortical thickness, the adequacy of screw purchase with stable fixation is quite challenging. This can result in non-unions as high as 75% [38]. Both locking and conventional plates can be used in the operative treatment of distal humeral fractures, but the bility to achieve primary stable fixation with conventional plating is limited in those fractures which are associated with osteopenia, metaphyseal communition and inability to achieve cortical contact. These are the fractures where locking plate should ideally be used. Most support doublecolumn plating but the configuration in which the plates should be applied remains controversial. Overall, the plates are normally applied either orthogonally or in parallel configuration [66].
Distal Radius Fractures
Distal radius fractures are the most commonly occurring fractures. Most of these fractures are treated conservatively in cast immobilisation. There are many surgical options available to operatively treat these fractures. Among these include closed reduction & pin fixation, external fixation and ORIF. Since a large majority of these fractures are also osteoporotic in nature, precontoured locking plates were developed with the view to provide stable fixation subsequently reducing the risk of loss of reduction and collapse of fracture site whilst facilitating early joint mobilization. The concept behind achieving fracture stability by using fixed angled devices is based on their ability to function as „neutralization devices? by supporting the subchondral bone without depending on distal screw purchase [52]. In osteoporotic fractures of distal radius, the strongest remaining bone is the subchondral plate; hence both smooth and threaded pegs provide reliable fixation if applied immediately below the subchondral bone [52]. The criss-cross orientation of the locking head screws and pegs provide a 3- dimentional scaffold that cradles the articular surface [52]. One of the most important aspects of treatment outcome is the functional status of the injured hand and wrist. Studies performed using conventional plating [7,13], external fixator [18,22,41] and volar locking plate [35] showed good to excellent functional outcome. However, the average grip strength was more than 90% in the case of conventional plating and externally fixation. Only 25% of the patients had excellent and 49% had good grip strength in the study performed by Hakimi et al. using volar locking plate [35]. Rizzo et al. compared volar locking plates, external fixation and pining [57]. The external fixation group was associated with higher DASH score and frequent hand therapy visits, thus volar locking plate was recommended to be more appropriate than external fixation. The use of external fixator also carries the risk of pin track infections, however most of these infections in the studies done were superficial and treated successfully with oral antibiotics leading to no subsequent complications [23,57]. One of the well known complications of using volar plating, whether locking or conventional, is rupture of flexor pollicis longus tendon. This complication is not seen with use of external fixator. The use of Kirschner wire for fixation of severely communited unstable intra-articular fracture is not recommended. K-wires are mostly indicated and appropriate for the Colle?s type distal radial fracture lying near to the joint which are deemed unstable by plaster immobilisation or similar fractures presenting with secondary displacement after initial plaster immobilisation [32]. Two common complications of K-wire fixation of distal radial fractures are nerve irritation (12%) and wire migration (10%) [62]. Locking plate fixation of those fractures amenable to treatment with K-wire fixation will not only be cost ineffective but should be considered an over treatment when good results have been shown by other studies [32,62].
Femoral Fractures
The LISS (Less Invasive Stabilisation System) and LCP (Locking Compression Plate) have been there since 1980?s for the treatment of femoral fractures. Although the starting point of locking devices in femur was for the treatment of sub-trochanteric fractures, LISS plate and LCP are developing a place in the treatment of the diaphyseal and distal femoral fractures. Intramedullary nails are in widespread use for femoral shaft fractures. Clinically significant rotational malunion have been found to be as high as 30% in femoral shaft fractures treated with intramedullary devices [10]. A biomechanical study performed by Citak, et al. comparing rotational strain pattern of intramedullary devices with both conventional and locking plates has shown clinically significant rotation in both statically and dynamically locked nails averaging 14.2o and 15.7o respectively [15]. Only 3.8o of rotational strain was seen when comparable physiological loads were applied to a locking plate-bone construct and this was found to be statistically significant. This demonstrates the superiority of the locking plates in controlling the rotational deforming forces under laboratory physiological loads. Supracondylar fractures of femur are one of the most challenging fractures to treat. These fractures can vary from purely supracondylar to fractures with intra-articular extension. Marked communition is a hallmark of these injuries especially in osteoporotic bones and multiple trauma. These injuries can sometime present as periprosthetic fractures in elderly patient with knee arthroplasty. Many different implants have been used to fix fractures of the distal femur namely condylar blade plate, intramedullary nail, DCS and buttress plating. Earlier results of fixing these fractures internally were not encouraging. Neer et al. showed 90% satisfactory results with nonoperative treatment in comparison to 52% with internal fixation [51]. Later studies performed by applying AO principles of fracture management markedly improved the outcome in these fractures. Thus Schatzker et al. quotes 75% good results with internally fixed supracondylar fractures in comparison to 32% managed non-operatively [59]. Severely comminuted and osteoporotic supracondylar fractures still pose a major challenge. Since the advent of the concept of „Biological plate fixation? more emphasis has been placed on preserving bone biology. The use of a LISS and LCP were developed in order to minimise the problems associated with other internal fixation devices, most of which rely on the friction between bone and implant for stability. The use of LISS plate in treating such complex and challenging fractures has resulted in a reasonably satisfactory outcome. In one study, Schutz, et al. achieved 90% union rate [60]. In another study, Syed et al. has reported 88% union rate in 25 patients of supracondylar fractures being treated with LISS plate [64]. Overall there was 12% infection rate including two superficial and one deep infection, both successfully treated with antibiotics [64]. Interestingly, Schutz et al. and Syed et al.showed a revision rate of 23% and 12% respectively [60,64]. The main reason of revision was found to be delayed/non-union in both studies. A comprehensive systematic review on using LISS plate in supracondylar fractures of 663 patients with 694 fractures, revealed a 40% complication rate. The common complications were residual deformity (38.4%), implant malpositioning (11.2%) and infection (9.8%) [61].
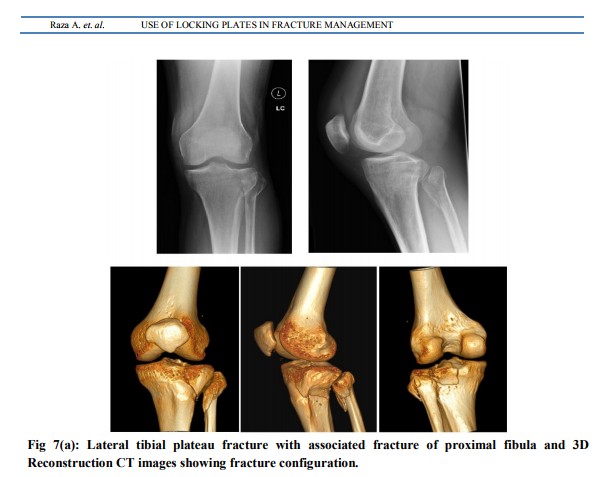
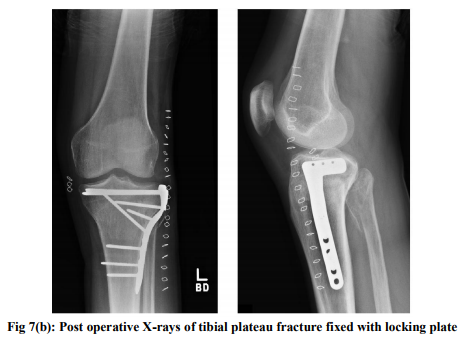
Tibial Fractures
Tibial plateau fractures involve proximal tibia in its articular and meta-epiphyseal segments [6]. The normal valgus alignment of lower limb with reduced bone strength of lateral tibial plateau relative to medial results in a greater frequency of lateral than medial tibial plateau fractures [50]. Minimally displaced fractures are treated nonoperatively, however, displaced fractures mostly require surgical fixation. Complex proximal tibial fractures are high energy injuries with severe soft tissue damage and extensive comminution. The use of locking plates is recently being explored in the management of such fractures [9,17,25,34,56]. Locking plates respect the biological environment of fracture and can be also applied by minimally invasive technique, however a prospective randomized study on the treatment of bicondylar tibial plateau fractures has failed to reveal any obvious advantage over conventional plates in terms of fracture healing, infection rate and adequacy of fixation [39]. Diaphyseal and extra articular distal tibial fractures are frequently treated with intramedullary devices. Studies have revealed good outcome with the use of reamed intramedullary nails in terms of fracture union and functional status [48]. Kayali et al. did not find any statistically significant difference between two groups of patients treated with either an intramedullary nail or locking plate [42]. However, patients treated with an intramedullary nail can have symptoms of anterior knee pain which can be as high as 29% [67]. In these cases, even if the nail is removed, 50% have persistent anterior knee pain. The tibia is a subcutaneous bone and distal part of this bone has limited muscle attachments, thus making it prone to delayed and non-unions. One of the most challenging varieties of distal tibial injuries are pilon fractures. These fractures involve distal tibial metaphysis with intra articular extension into the ankle joint. A number of different devices are available for the treatment of these fractures namely conventional plates and screws and external fixation. Complications range from 20-50% [49]. Joveniaux et. al. reported an overall 30% complication rate of conventional plating, limited internal fixation using screws/Kwires and external fixation in distal tibial fractures [40]. Whereas Hazarika et al. showed better results using LISS plate and 10% non-union rate [37]. Hasenboehlr et al. also showed comparable results with LCP used in a minimally invasive fashion [36]. In this study, two out of three non-unions were seen in patients with history of peripheral vascular disease and chronic alcohol abuse with heavy smoking. The high profile of the locking plate with limited soft tissue cover over distal tibia can result in pressure ulcers or hardware irritation requiring removal [36].
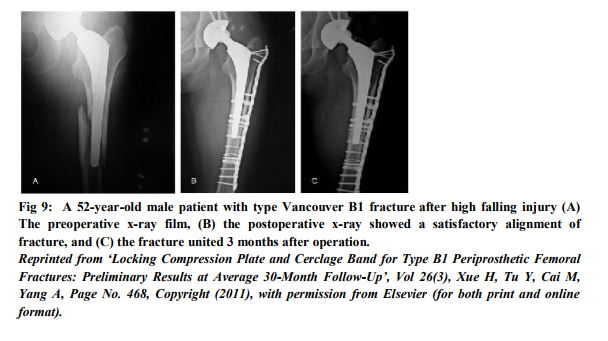
Peri-prosthetic Fractures
The incidence of peri-prosthetic fractures is only 0.3% to 2.5% [21]. These fractures pose a grave challenge to trauma surgeons as they are difficult to treat requiring lot of experience and novel approaches. Due to the presence of previous implant, there is already limited bone available to achieve fracture stability. Also the presence of cement can make it extremely difficult and often impossible to use intramedullary devices in the treatment of these fractures. Locking plates have been found to be an effective option in the treatment of these fractures particularly using MIPO technique. LCP is commonly used for proximal femoral periprosthetic fractures and LISS for the distal ones. These plates when applied using minimally invasive technique preserve periosteal circulation allowing biological fixation. In order to avoid compromising the cement mantle or prosthesis, unicortical locking screws can be used. This can be further augmented by the use of cerclage wires [11,69]. Those authors who have employed minimally invasive techniques have shown lower implant failure and non-union rates. Buttaro, et al. used LCP for Vancouver type B1 fractures using open technique [11]. He noticed 43% implant failure in those fractures where LCP was not augmented with cerclage wire and strut graft and recommends this combination. He attributes implant failure secondary to extensive soft tissue stripping thus compromising bone healing. According to a systematic review by Smith, et al. the non-union rate of LISS plate for distal femur peri-prosthetic fractures was 3.5% [61]. A meta-analysis of 195 periprosthetic fractures showed a complication rate as high as 30% [14]. Kobbe, et al. conducted a midterm follow up of patients with peri-prosthetic fractures treated with LISS plate and found Harris hip score of 79.5% [44]. He also noted two cases (13%) of screw pull out. The study by Kregor et al. on supracondylar fractures around total knee arthroplasty showed complete unions in all the treated patients with LISS plate [46]. There was no incidence of screw pull out in his study. Several other case series have shown benefit of locking plates in fixing periprosthetic fractures [26,27,28,68].
CONCLUSION
Locking plates were developed to overcome the problems associated with fracture management of osteoporotic bones. Locking plates are part of the evolution of extra-medullary techniques to preserve biology, allow controlled movement (relative stability), encourage fracture healing and yet still allow early mobilization [49]. The superiority of locking plates has been proven by many biomechanical studies. Although some clinical trials have shown benefit, conclusive evidence is still lacking. This is due to the relative lack of good high powered randomised control trials. Even systematic reviews have failed to give a final verdict due to the lack of well controlled studies. The literature supports using locking plates for fixation of periarticular fractures of long bones, multifragmentary fractures of diaphysis & metaphysis and periprosthetic fractures. Ultimately, locking plates are not the panacea for all type of fractures. As clinical experience with locking plate broadens, new indications and applications will emerge. Overall, surgeons have started using these devices confidently in treating fractures and with time more evidence will be generated to further define the role of locking plates in the treatment of fractures. Until then, the treatment choice is still largely based on surgeon?s preference.
ACKNOWLEDGMENTS
We acknowledge the valuable comments of Mr Robert Smith, Consultant Orthopaedic Surgeon, Wrightington, Wigan and Leigh NHS Trust in the preparation of this review article.


References:
REFERENCES
1. Apivatthakakul T, Phornphutkul C, Laohapoonrungsee A, Sirirungruangsarn Y. Less invasive plate osteosynthesis in humeral shaft fractures. Oper Orthop Traumatol 2009; 21(6):602-13.
2. Apivatthakakul T, Patiyasikan S, Luevitoonvechkit S. Danger zone for locking screw placement in minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures: a cadaveric study. Injury 2010; 41(2):169-72.
3. Bae JH, Oh JK, Oh CW, Hur CR. Technical difficulties of removal of locking screw after locking compression plating. Arch Orthop Trauma Surg 2009; 129(1):91-5.
4. Bagby GW. Compression bone-plating: historical considerations. J Bone Joint Surg Am 1977; 59(5):625-631.
5. Baron JS, Barrett JA, Karagas MR. The epidemiology of peripheral fractures. Bone 1996; 18(3 Suppl):209S-213S.
6. Biggi F, Di Fabio S, D'Antimo C, Trevisani S. Tibial plateau fractures: internal fixation with locking plates and the MIPO technique. Injury 2010; (11):1178-82.
7. Blatter G, Weber GB. Wave plate osteosynthesis as a salvage procedure. Arch Orthop Trauma Surg 1990; 109(6):330-3.
8. Blyth MJ, Macleod CM, Asante DK, Kinninmonth AW. Iatrogenic nerve injury with the Russell-Taylor humeral nail. Injury 2003; 34(3):227-8.
9. Boldin C, Fankhauser F, Hofer HP, Szyszkowitz R. Three-year results of proximal tibia fractures treated with the LISS. Clin Orthop Relat Res 2006; 445:222-9.
10. Bråten M, Terjesen T, Rossvoll I. Torsional deformity after intramedullary nailing of femoral shaft fractures. Measurement of anteversion angles in 110 patients. J Bone Joint Surg Br 1993; 75(5):799-803.
11. Buttaro MA, Farfalli G, Paredes Núñez M, Comba F, Piccaluga F. Locking compression plate fixation of Vancouver typeB1 periprosthetic femoral fractures. J Bone Joint Surg Am 2007; 89(9):1964-9.
12. Camden P, Nade S. Fracture bracing the humerus. Injury 1992; 23(4):245-8.
13. Catalano LW 3rd, Cole RJ, Gelberman RH, Evanoff BA, Gilula LA, Borrelli J Jr. Displaced intra-articular fractures of the distal aspect of the radius. Long-term results in young adults after open reduction and internal fixation. J Bone Joint Surg Am 1997;79(9):1290-302.
14. Chen F, Mont MA, Bachner RS. Management of ipsilateral supracondylar femur fractures following total knee arthroplasty. J Arthroplasty 1994; 9(5):521-6.
15. Citak M, Kendoff D, Gardner MJ, Oszwald M, O'Loughlin PF, Olivier LC, Krettek C, Hüfner T, Citak M. Rotational stability of femoral osteosynthesis in femoral fractures - navigated measurements. Technol Health Care 2009; 17(1):25-32.
16. Clark WA. History of fracture treatment up to the sixteenth century. J Bone Joint Surg Am 1937; 19:47-63.
17. Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma 2004; 18(8):528- 35.
18. Cooney WP 3, Linscheid RL, Dobyns JH. External pin fixation for unstable Colles' fractures. J Bone Joint Surg Am 1979; 61(6A):840-5.
19. Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand 2001; 72:365-71.
20. Dabezies EJ, Banta CJ 2nd, Murphy CP, d'Ambrosia RD. Plate fixation of the humeral shaft for acute fractures, with and without radial nerve injuries. J Orthop Trauma 1992; 6(1):10-3.
21. Dennis DA. Periprosthetic fractures following total knee arthroplasty. Instr Course Lect 2001; 50:379-89.
22. Edwards GS Jr. Intra-articular fractures of the distal part of the radius treated with the small AO external fixator. J Bone Joint Surg Am 1991; 73(8):1241-50.
23. Edwards SL, Wilson NA, Zhang LQ, Flores S, Merk BR. Two-part surgical neck fractures of the proximal part of the humerus. A biomechanical evaluation of two fixation techniques. J Bone Joint Surg Am 2006; 88(10):2258-64.
24. Eggers GWN, Shindler TO, Pomerat CM. The Influence of the Contact-Compression Factor on Osteogenesis in Surgical Fractures. J Bone and Joint Surg 1949; 31A:693-716.
25. Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ. Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma 2004; 57(2):340-6.
26. Ehlinger M, Adam P, Moser T, Delpin D, Bonnomet F. Type C periprosthetic fractures treated with locking plate fixation with a mean follow up of 2.5 years.Orthop Traumatol Surg Res 2010; 96(1):44-8.
27. Ehlinger M, Adam P, Abane L, Rahme M, Moor BK, Arlettaz Y, Bonnomet F. Treatment of periprosthetic femoral fractures of the kneeKnee Surg Sports Traumatol Arthrosc 2011; 19(9):1473-8.
28. Ehlinger M, Adam P, Di Marco A, Arlettaz Y, Moor BK, Bonnomet F. Periprosthetic femoral fractures treated by locked plating: feasibility assessment of the mini-invasive surgical option. A prospective series of 36 fractures. Orthop Traumatol Surg Res 2011; 97(6):622-8.
29. Erhardt JB, Roderer G, Grob K, Forster TN, Stoffel K, Kuster MS. Early results in the treatment of proximal humeral fractures with a polyaxial locking plate. Arch Orthop Trauma Surg 2009; 129(10):1367-74.
30. Farragos AF, Schemitsch EH, McKee MD. Complications of intramedullary nailing for fractures of the humeral shaft: a review. J Orthop Trauma 1999; 13(4):258-67.
31. Fenichel I, Oran A, Burstein G, Perry Pritsch M. Percutaneous pinning using threaded pins as a treatment option for unstable two- and three- part fractures of the proximal humerus: a retrospective study. Int Orthop 2006; 30(3):153-7.
32. Fritz T, Wersching D, Klavora R, Krieglstein C, Friedl W. Combined Kirschner wire fixation in the treatment of Colles fracture. A prospective, controlled trial. Archives of orthopaedic and trauma surgery 1999; 119(3- 4):171-8.
33. Füchtmeier B, May R, Hente R, Maghsudi M, Völk M, Hammer J, Nerlich M, Prantl L. Proximal humerus fractures: a comparative biomechanical analysis of intra and extramedullary implants. Arch Orthop Trauma Surg 2007; 127(6):441-7.
34. Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res 2005; 439: 207-14.
35. Hakimi M, Jungbluth P, Windolf J, Wild M. Functional results and complications following locking palmar plating on the distal radius: a retrospective study. J Hand Surg Eur 2010; 35(4):283-8.
36. Hasenboehler E, Rikli D, Babst R. Locked compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury 2007; 38(3):365-70.
37. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia-- results in 20 patients. Injury 2006; 37(9):877- 87.
38. Helfet DL, Hotchkiss RN. Internal fixation of the distal humerus: a biomechanical comparison of methods.J Orthop Trauma 1990; 4(3):260-4.
39. Jiang R, Luo CF, Wang MC, Yang TY, Zeng BF. A comparative study of Less Invasive Stabilization System (LISS) fixation and twoincision double plating for the treatment of bicondylar tibial plateau fractures. Knee 2008; 15(2):139-43.
40. Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, Mainard D, Vix N, Dehoux E. Distal tibia fractures: management and complications of 101 cases. Int Orthop 2010; 34(4):583-8.
41. Kapoor H, Agarwal A, Dhaon BK. Displaced intra-articular fractures of distal radius: a comparative evaluation of results following closed reduction, external fixation and open reduction with internal fixation.Injury 2000; 31(2):75-9.
42. Kayali C, A?u? H, Eren A, Ozlük S. How should open tibia fractures be treated? A retrospective comparative study between intramedullary nailing and biologic plating.Ulus Travma Acil Cerrahi Derg 2009; 15(3):243-8.
43. Keener JD, Parsons BO, Flatow EL, Rogers K, Williams GR, Galatz LM. Outcomes after percutaneous reduction and fixation of proximal humeral fractures. J Shoulder Elbow Surg 2007; 16(3):330-8.
44. Kobbe P, Klemm R, Reilmann H, Hockertz TJ. Less invasive stabilisation system (LISS) for the treatment of periprosthetic femoral fractures: a 3-year follow-up. Injury 2008; 39(4):472-9.
45. Kralinger F, Gschwentner M, Wambacher M, Smekal V, Haid C. Proximal humeral fractures: what is semi-rigid? Biomechanical properties of semi-rigid implants, a biomechanical cadaver based evaluation. Arch Orthop Trauma Surg 2008; 128(2):205-10.
46. Kregor PJ, Hughes JL, Cole PA. Fixation of distal femoral fractures above total knee arthroplasty utilizing the Less Invasive Stabilization System (L.I.S.S.). Injury 2001; 32(3):64-75.
47. Kubiak EN, Fulkerson E, Strauss E, Egol KA. The evolution of locked plates. J Bone Joint Surg Am 2006; 88 Suppl 4:189-200.
48. Lam SW, Teraa M, Leenen LP, van der Heijden GJ. Systematic review shows lowered risk of nonunion after reamed nailing in patients with closed tibial shaft fractures. Injury 2010; 41(7):671-5.
49. Lambotte MA. Technique and indications of the prosthesis into the lost treatment of fractures. Presse med 1909; 17:321-323.
50. Mallina R, Kanakaris NK, Giannoudis PV. Peri-articular fractures of the knee: An update on current issues. Knee 2010; 17(3):181-6.
51. Neer CS 2nd, Grantham SA, Shelton ML. Supracondylar fracture of the adult femur. A study of one hundred and ten cases. J Bone Joint Surg 1967; 49(4):591-613.
52. Orbay J. Volar plate fixation of distal radius fractures. Hand Clin 2005; 21(3):427-41.
53. Perren SM, Schlegel U. Surgical aspects of implants and infection: the effect of material, design and application on resistance to local infection. Nova Acta Leopoldina 2001; 84:65- 73.
54. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br 2002; 84(8):1093-110.
55. Perren SM. Backgrounds of the technology of internal fixators. Injury 2003; 34(2):1-3.
56. Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma 2007; 21(2):83-91.
57. Rizzo M, Katt BA, Carothers JT. Comparison of locked volar plating versus pinning and external fixation in the treatment of unstable intraarticular distal radius fractures. Hand (N Y) 2008; 3(2):111-7.
58. Sarmiento A, Kinman PB, Galvin EG, Schmitt RH, Phillips JG. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am 1977;
59(5):596-601. 59. Schatzker J, Home G, Waddell J. The Toronto experience with the supracondylar fracture of the femur. Injury 1974; 6(2):113-28.
60. Schütz M, Müller M, Krettek C, Höntzsch D, Regazzoni P, Ganz R, Haas N. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury 2001; 32( 3):48-54.
61. Smith TO, Hedges C, MacNair R, Schankat K, Wimhurst JA. The clinical and radiological outcomes of the LISS plate for distal femoral fractures: A systematic review. Injury 2009; 40(10):1049-63.
62. Strohm PC, Müller CA, Boll T, Pfister U. Two procedures for Kirschner wire osteosynthesis of distal radial fractures. A randomized trial. J Bone Joint Surg Am 2004; 86-A(12):2621-8.
63. Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, Luo C, Plecko M, Wendt K, Köstler W, Konrad G. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am 2009; 91(6):1320-8.
64. Syed AA, Agarwal M, Giannoudis PV, Matthews SJE, Smith RM. Distal femoral fractures: long-term outcome following stabilisation with the LISS. Injury 2004; 35(6):599-607.
65. Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg 2009; 18(6):837-44.
66. Theivendran K, Duggan PJ, Deshmukh SC. Surgical treatment of complex distal humeral fractures: functional outcome after internal fixation using precontoured anatomic plates. J Shoulder Elbow Surg 2010; 19(4):524-32.
67. Väistö O, Toivanen J, Kannus P, Järvinen M. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft: an eight-year follow- up of a prospective, randomized study comparing two different nail-insertion techniques. J Trauma 2008; 64(6):1511-6.
68. Wood GC, Naudie DR, McAuley J, McCalden RW. Locking compression plates for the treatment of periprosthetic femoral fractures around well-fixed total hip and knee implants. J Arthroplasty 2011; 26(6):886-92.
69. Xue H, Tu Y, Cai M, Yang A. Locking compression plate and cerclage band for type B1 periprosthetic femoral fractures preliminary results at average 30-month follow-up. J Arthroplasty 2011; 26(3): 467- 471.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License