IJCRR - 6(6), March, 2014
Pages: 93-99
Print Article
Download XML Download PDF
TUBERCULAR CERVICAL LYMPHADENITIS : EXPERIENCE OVER A FOUR YEAR PERIOD
Author: Vineet Chaudhary, M. Abbas Ali, Ravi Mathur
Category: Healthcare
Abstract:Objective: This Study was done with the Aim to investigate various Clinico-pathological aspects of Tubercular cervical lymphadenitis. Material and Methods: Four hundred patients with cervical lymphadenopathy of all age group, out of which 220 males and 180 females who attended OPD of NIMS Medical college, Jaipur between March 2009 and Feb 2013 were included in study.FNAC of Cervical lymph nodes was done. The lymph node biopsy was done in selected patients. Mycobacterial culture was also done in selected patients. Total 218 cases of tubercular cervical lymphadenitis (proved by FNAC/Biopsy) were included in this study. Results: Most common cause of cervical lymphadenopathy was found to be tubercular in 218 patients (54.5%). Female/Male Ratio was 1:84. Younger Age Group (15-30 years) was most commonly affected, seen in 77 patients (35.32%). Diagnostic accuracy of FNAC in tubercular lymphadenitis was 95.41% .Concurrent pulmonary tuberculosis was seen in 33 patients (15%).Constitutional symptoms were present in 32 patients(14.67%).Montoux Test was positive in 100 patients(45.87%). Posterior Triangle of neck was most commonly involved.Commonest presentation of tubercular lymph nodes was multiple matted lymph nodes, seen in 110 patients (50.45%).In our study 150 patients (68.80%) presented as 2-4cms size lymph nodes. Conclusion: This study also emphasizes that complications can be minimized by regular anti tubercular treatment, good patient compliance and regular follow up especially for development of fresh complications.
Keywords: Tubercular cervical lymphadenitis, FNAC, ATT, Defaulters, Excisional biopsy, mycobacterium culture.
Full Text:
INTRODUCTION
Cervical lymphadenopathy is one of the commonest clinical presentation of the patients attending hospital outdoor.Grossly cervical lymph node enlargement can be classified as Acute and chronic cervical lymphadenitis. Chronic cervical lymphadenitis usually presents as chronic painless enlargement of cervical lymph nodes. Etiology of chronic cervical lymphadenitis is either tubercular or due to secondary malignant deposits or lymphomas. Tubercular lymphadenitis (historically referred to as scorfula) is the commonest form of extrapulmonary tuberculosis reported in children from TB endemic areas ,present in 8-10% of children diagnosed with TB in India and South Africa (1,2). Lymph nodes become infected with mycobacterium tuberculosis following lymphatic drainage from local disease site or after haemetogenousdisiminetion .The aim of this study was to investigate various clinicopathological aspects of tubercular cervical lymphdenitis among patients presenting to Four hundred patients with cervical lymphadenopathy of age group,new born to s
our institute over a four year period.
MATERIALS AND METHODS
eventy five years,out of which 220 males and 180 females who attended OPD of NIMS Medical college, Jaipur between March 2009 and Feb 2013 were included in study .Written Informed consent was obtained from all study subjects. All patients were clinically assessed and a detalied history was taken regarding age , sex ,mode of onset ,duration, distribution, family history, presence or absence of pain, fever, weakness, loss of weight, night sweats, anemia, cough, progress of disease. All clinical records were maintained. After taking patient’s history, full clinical examination was done. Special emphasis was made to site/size/clinical stage of cervical lymph node. All patients were subjected to routine investigations CBC, ESR,MT, X-Ray chest PA view. FNAC of Cervical lymph nodes was done with help of 10cc disposable syringe and needle (22gauge). Half smears were dried in air and half were fixed by immersing in absolute alcohol for one hour .The lymph node biopsy was done in selected patients. Mycobacterial culture was also done in selected patients.Total 218 cases of tubercular cervical lymphadenitis (proved by FNAC/Biopsy) were included in this study.
OBSERVATIONS
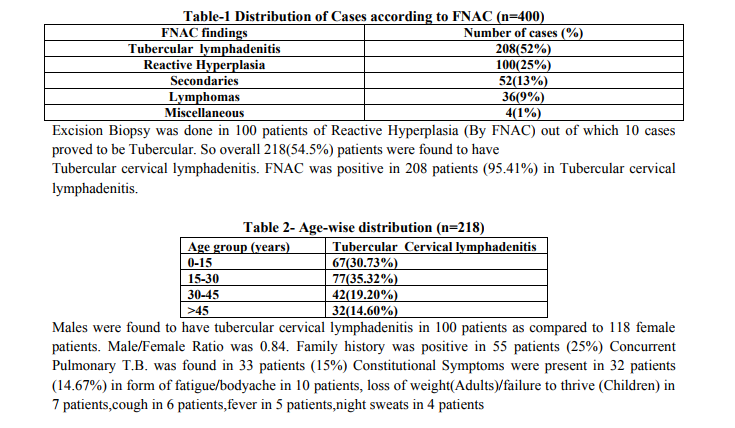
Out of total 400 patients, 220 (55%) were males and rest 180(45%) were females. Tubercular lymphedentis was the most common FNAC finding in 208 patients (52%) followed by Reactive hyperplasia in 100 patients (25%).
DISCUSSION
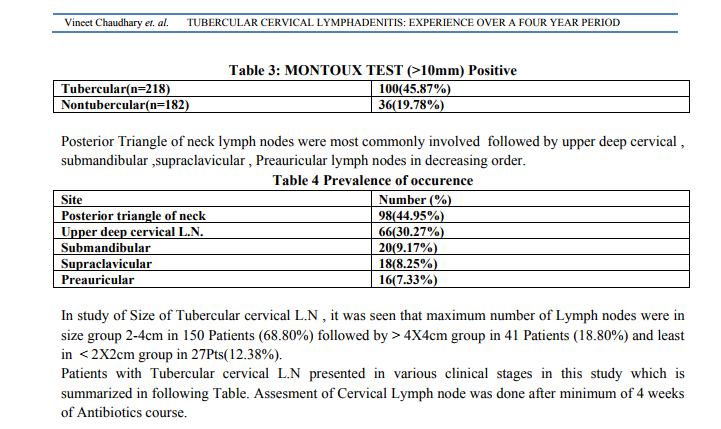
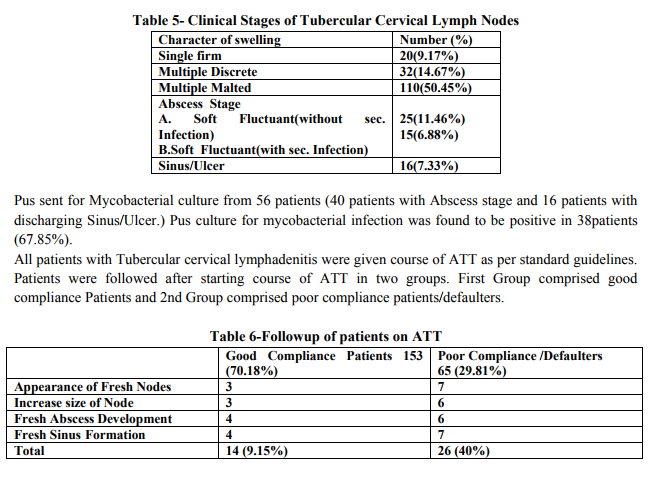
Lymphadenitis is the most frequently occurring form of pulmonary TB, with cervical Nodes being most commonly involved in adults. Although inguinal, mesenteric and mediastinal Nodes may be involved (1, 2.) It has been found that by FNAC alone, 208 patients (52%) were found to have tubercular cervical lymphadenitis followed next by Reactive Hyperplasia in 100 patients (25%). These 100 patients with Reactive Hyperplasia group were also subjected to Excisional Biopsy. It has been found in our study that 10 patients of Reactive Hyperplasia group proved to be Tubercular by Excisional Biopsy. So overall by Excicional Biopsy overall 218 (54.5%) patients proved to be tubercular in our study. This study emphasises that Tubercular cervical lymphadenitis is one of the most common clinical presentation of Extra pulmonary tuberculosis. In our study, FNAC of cervical lymph Node Biopsy was positive for Tubercular lesion in 208 patients, out of 218 patients. So, Diagnostic accuracy of FNAC in Tubercular Cervical lymphadenitis was 95.41% in our study. This study emphasises importance of FNAC in diagnosis of Tubercular Cervical Lymphadenopathy. Fine Needle aspiration is suggested as an initial investigation if lymph node Tuberculosis is suspected. (3) FNAC constituted main diagnostic tool, with positive yield in 90% on Patients, TB cervical lymphadenitis can be readily diagnosed by FNAC as a simple and cost-effective test. (4) Fine needle aspiration is simple, cheap and may be of value in the diagnosis of Tuberculosis, especially in developing countries with limited diagnostic and therapeutic resources.(5) In our study, 77 patients(15.32%) were found to have Tubercular Cervical Lymphadenitis in 15-30 year age group, followed by 67 patients (30.73%) patients in children age group (0-15 yr); 42 patients (19.20%) in 30-45 years age group and 32 patients (14.60%) in >45 age group. Our study shows maximum incidence of Tubercular Cervical Lymphadenitis in younger and children age group.Tuberculosis was found to be common in young patients who are in accordance with local data as well as international data. (6)In another study, Tuberculosis found to be commomest in young adult females (15-24yrs) age group and rare above age of 45yrs. (7) It has peak incidence in 20-40 age groups. (8) In our study. Tubercular Lymphadenitis was found in 118 (54.12%) female patients as compared to 100 (45.87%) male patients. So in our study, M: F was 0.84:1. TB lymphadenitis is showing some atypical characteristics for its distribution according to age and sex as it is more common in females and in younger age groups, in compare to pulmonary TB which is more commonly affects males and older age group.(9) Family History of any form of Tuberculosis in our study was found in 55 patients (25%). Concurrent Pulmonary tuberculosis was found in 33(15%) patients in our series. Constitutional symptoms were found in 32 (14.67%) patients. Fatigue, Bodyache was commonest symptom in 10 patients (4.58%) followed by loss of weight, failure to thrive (children) in 7 patients (3.21%), cough in 6 patients (2.75%), fever in 5 patients (2.29%), Night sweats in 4 patients (1.83%).Most physicians agree that Tubercular Cervical Lymphadenitis is a local manifestation of systemic infection but a striking feature of many reports in infrequent occurrence of systemIc features and specifically of pulmonary involvement. (10) Constitutional symptoms were not present in most patients in few series. In several series, in approximately 80% (11) patients, the chest films were normal so there is continuous debate whether Tubercular Cervical Lymphadenitis is a localized disease or a part of systemic disease. (12) Post Traingle of Neck was found to be most common involved in 98 patients (44.95% ) followed by upper deep cervical lymph nodes in 66 patients(30.27%) , submandibular lymph node in 20(9.17%) patients ,supraclavicular in 18(8.25%),preauricular lymph node in 16 patients(7.33%). In a study by Pameraetal (15) regarding distribution of enlarged lymph nodes, the upper jugular, submandibular and supraclavicular groups were found involved more often and occipital group less often. Montoux Test was positive in Tubercular Cervical Lymphadenitis in 100 patients (45.87%). Among 100 Tubercular cases (M.T. positive), 48 patients were below 15 years age. Hence Montoux Test was positive in 48 patients, out of 67 patients (71.64%) in 2cm, upto 4 cm) was found in 150 patients (68.80%), followed by LN size (>4cm) in 41 patients (18.80%), LN (<2cm) in 27 patients (12.38%). Pus/discharge sent frorMycobacterial culture in 40 patients presenting as soft fluctuant swelling(Abscess) and remaining 16 patients presenting as Sinus/Ulcer Pus culture for mycobacterial infection was found to be positive in 38patients (67.85%) In another study (16), 52 patients out of 80 (65%) showed positive culture for Mycobacterium Tuberculosis of human type in Lowenstein Jensen medium.Comparison was made between two groups. First group included 152 patients (70.18%) who were regularly taking ATT and second group included 65 patients (29.81%) with poor compliance/defaulters. It was found that in Defaulter group, appearance of fresh nodes was seen in 7 patients,increase in size of nodes in 6 patients, fresh abscess development in 6 patients and sinus formation in 7 patients, as compared to 1st group( Patients on regular ATT andgood compliance)these figures were 3 patients,3 patients, 4patients ,4 patients respectively. Over complication rate during course of ATT was seen in 26 patients (40%) in defaulter group campared to 14 patients (9.15%) in 1st group. This emphasises importance of Regular course of ATT in management of tubercular lymphadenitis. 14(9.15%) patients inspite of regular ATT developed various complications like Abscess/Sinus formation. Fresh untreated cases of tubercular cervical lymphadenitis were managed by 2 months Isonex, Rifampicin, Pyrazinamide followed by 4 months Isonex, and Rifampiciin. Relapses/ Defaulters managed by 2 (HRZES), 5(HRE). Randomised controlled trials have demostrated convincingly that tubercular lymphadenopathy can be treated by short course of chemotherapy. In adults the results of 9 months of INH, Rifampicin accompanied by Ethambutol for initial 2 months did not differ significantly from those receiving prolonged therapy of 18 months.(17) Equally good results were achieved by using a regimen of RMP and INH for 6 months supplemented by PZA during initial 2 months. (18) Paradoxical expansion of lymph node may be seen during first 2 months of treatment in up to 20% of cases, but the occurrence thereof doesn't indicate failure of chemotherapy. (19) Excision as treatment option is particularly suitable in Non tubercular mycobacterial infections, where the therapeutic response to chemotherapy is frequently suboptimal. (20) Incisional Biopsy should be avoided because it tends to result in sinus formation. (21)
CONCLUSION
Presentation of tuberculosis is not only as pulmonary but cervical lymphadenopathy also a common presentation. Most common cause of cervical lymphadenopathy was found to be tubercular followed by reactive lymphadenitis , metastatic deposits and Lymphomas.Cervical lymphadenopathy was commonly affect Younger Age Group(15-30years) Diagnostic accuracy of FNAC in tubercular lymphadenitis was 95.41% in our study which emphasises importance of FNAC as simple, cheap and excellent first line diagnostic step. Posterior Triangle of neck was most commonly involved. Commonest presentation of tubercular lymph nodes was multiple matted lymph nodes. In our study most of patients presented as 2-4 cms size lymph nodes. Various complications like appearance of fresh nodes, abscess, sinus etc are seen in more in defaulter/poor compliance patients as compared to patients who were regularly taking ATT. This study also emphasizes that complications can be minimized by regular anti tubercular treatment, good patient compliance & regular follow up specially for development of fresh complications.
References:
REFERENCES
1. Dandapat MC, Mishra BM, Dash Spectal peripheral lymph node tuberculosis: a review of 80 cases BrJ. Surg. 1990; 77: 911-912.
2. Memish ZA MahMW, Mahmood SA etal.Clinico diagnostic experience with Tuberculouslymphodenitis in Saudi Arabia. ClinMicriobiol Infect 2000:6:137-141.
3. Diagnosis and therapy of Lymph Node Tuberculosis .Praxis (Bern 1994) 1999 Jan 21, 88(4) 105-112.
4. J.laryngolotol 2009 July, 123 (7) Khan R, Harris SH, Vama AK, Syed A .Dept. of Pathology, JN Medical College, AMU.
5. ”Fine Needle Extra thoracic aspiration in HIV associated sputum Negative Tuberculosis”.Lancet 1992Dec 19- 26,340(8834-8835):1504-5
6. KhanAcl, Nawaz G. Khan Ar. An audit of 75 cases of cervical lymphadenopathy. J. Med.Sci. 2011; 19:95-97.
7. Olu, Eddo An, Ohanaka CE Peripheral lymphadenopathy in Nigerian adults. J pak Med Assoc 2006, 56, 405-408.Lancet 1992 Dec 19-26, 340 (8834-8835): 15.4-5.
8. Golden MP and VikramHR (2005) Extra Pulmonary tuberculosis: An overview Am. Fam. Physician 72: 1761-1768.
9. Shubha AB, Sapna H, Dinesh RB (2010) Tubercular lymphadenitis presenting a diagnostic Dilemma – a case report Int J Dent.Clin 2:48-52.
10. Mair IW Elverland HH. Cervical mycobacterial Infection J.Larygolotolo 1975:89.933-939.
11. Cervical Tuberculous lymphadenopathy: Changing Clinical patterns, and concepts in management. B Jha A Das N Nagarker R Gupta and S Singhal Post Grad. Med J. 2001 March 77 (905) 185-187
12. Ord RJ, Matz GJ. Tuberculous cervical lymphadenitis. Arch otolaryngnol 1974; 99:327-329.
13. Schroeder KE, Elverland HH, Mair IW, Liavaag PG GranulomAtous Cervical lymphadenitis J.Otolaryngol 1979:8:127-131
14. Wong ML, Jafe KBN Cervical mycobacterial disease. Trans Am AcadOpthalmootolary 1974; 78:75-87.
15. PamraSP, MathurGP, a Cooperative study of Tuberculous cervical lymphadenitis, Indian J Med Res.1974; 62:1631-1646
1 6. Peripheral L.Node Tuberculosis: A review of 80 cases BJS vol. 77, Issue 8, pages 911-912 Aug 1990 professor M.C.Dandapat, BM Mishra , S.P. Dash, P.K.Kar.
17. Campbell JA The Treatment of Superficial Tuberculous lymphadenitis. Tubercle 1990,71:1-3.
18. Campbell JA, Ormerod IP Friend JAR, etal. Six months versus nine months chemotherapy for Tuberculosis of lymph nodes: preliminary results Resp Med 1992, 86:15-19.
19. Goldmacher H, Taule C, Krolger C, etalAssesment of LN tuberculosis in Northern Germany, A clinical review Chest 2002:121:1177-1182.
20. Lindeboom JA, Kunper FJ, Prins J Metal. TuberculosIs Clinical Infect Dis 2006, 43 :1547-1551.
21. Marais BJ, Wright CA, Schaaf HS. Tuberculous lymphadenitis as a cause of cervical lymphadenopathy in children from Tuberculous endemic area. Paed.InfDis J 2006, 25:142-146
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License