IJCRR - 6(6), March, 2014
Pages: 48-54
Print Article
Download XML Download PDF
ABNORMAL LEFT VENTRICULAR RELAXATION IN YOUNG PREHYPERTENSIVES: A CASE CONTROL STUDY
Author: Santha Kumari, Jaiganesh K., Amirtha Ganesh
Category: Healthcare
Abstract:Background: Prehypertension predicts established hypertension. The structural and functional alteration of the heart caused by prehypertension is unclear. Aims and Objectives: The present study was designed to compare the diastolic function in young normotensive and prehypertensive subjects between the age group of 18\?35 years. Subjects and Methods: Pulse wave transmitral Doppler echocardiographic data was assessed in 100 subjects. Of which, 50 were normotensives (systolic < 120 mm Hg and diastolic < 80 mm Hg) and 50 were prehypertensives (systolic = 120 \? 139 mm Hg and diastolic = 80 \? 89 mm Hg). Their early and late diastolic peak mitral flow velocity ratio (E/A ratio) were measured. Un-paired student's t-test was used for statistical analysis. Results: When compared with normotensive, in the prehypertensive group the E/A ratio was significantly decreased (p=0.05) Conclusion: This study concludes that diastolic abnormalities starts even in young prehypertensive individuals. The changes in the indices of diastolic function were only subtle in this age group of prehypertensives. Prehypertension is a predictor of established hypertension and diastolic dysfunction.
Keywords: Prehypertension, E/A ratio
Full Text:
INTRODUCTION
Hypertension is one of the major cardiovascular risk factor and is reported to be the fourth contributor to premature death in developed countries and seventh in developing countries (1). Hypertension is defined as persistent elevation of blood pressure equal to or more than 140 mm Hg systolic and equal to or more than 90 mm Hg diastolic in adults. The Seventh Report of Joint National Committee on Prevention, Detection, Evaluation and Treatment of high blood pressure (JNC-7) introduced a new category, prehypertension where systolic blood pressure was 120-139 mm Hg and diastolic blood pressure 80 - 89 mm Hg(2). The overall prevalence of prehypertension in our general population is almost comparable with that of United States (31%). Prehypertension was highest in the age group of 30 - 39 years (36%)(3,4). Prehypertension predicts established hypertension. A number of structural changes in the heart which eventually leads to systolic and diastolic abnormalities is caused by hypertension per se. Left ventricular diastolic dysfunction has been reported to be the earliest manifestation of cardiac involvement in subjects with hypertension. Diastolic impairment is associated with significant morbidity and mortality (5, 6). Few studies show that diastolic dysfunction starts even at the prehypertensive stage(7) . Cardiovascular structure and function can be studied by non-invasive imaging methods like pulse wave Doppler echocardiography. Altered mitral inflow velocities indicating prolonged left ventricular relaxation can be detected by this method even before any clinical or electrographic abnormalities develop (8- 10). The aim of this study is to compare the left ventricular diastolic function in young normotensives and prehypertensives. To assess and compare the diastolic function parameters E- velocity, A- velocity and E/A ratio in young normotensive and prehypertensives subjects.
SUBJECTS AND METHODS
This study was conducted after receiving the approval from Research Committee and Institutional Human Ethical Committee (IHEC), of Mahatma Gandhi Medical College and Research Institute, Puducherry, India. 100 subjects between 18 to 35 years of age of both genders were recruited from outpatient medicine department and master health check up of our institution from January 2012 to June 2013. Among them, 50 subjects were cases (prehypertensives) and 50 were controls (normotensives).
Inclusion criteria:
? Subjects between the age group of 18 to 35 years. ? Normotensive individuals with systolic BP 100 - 119 mm Hg and diastolic BP 60 - 79 mm Hg ? Prehypertensive individuals with systolic BP 120 - 139 mm Hg and diastolic BP 80 - 89 mm Hg
Exclusion criteria
Stage I and II hypertensives ? Secondary hypertension including chronic kidney disease, hypertensives with target organ damage. ? History of coronary artery disease, congestive heart failure, cardiomyopathies, diabetes, pregnancy. ? Use of anti- hypertensives, steroids or cardio active medications. Age, gender, anthropometric measurements, occupation, personal history were collected.
Blood pressure measurement
(11): Subjects were asked to rest in supine position for about 5-10 minutes in a quiet, calm examination room. Based on accuracy and reliability blood pressure was measured using standard mercury sphygmomanometer. Appropriate cuff selection based on the circumference of the bare upper arm at the midpoint between the shoulder and the elbow was selected. The cuff is wrapped around the midpoint of the bare upper arm. The lower edge of the cuff should be 2.5 cm above the antecubital fossa where the head of the stethoscope is to be placed. Inflate the cuff rapidly to 70 mm Hg and then by 10 mm Hg increments while palpating the radial pulse. The reading at which the pulse disappears is noted. By inflating the cuff rapidly and steadily to a pressure 20 - 30 mm Hg above the level previously determined by palpation and then deflating at 2 mm Hg/sec. As the pressure in the cuff falls, the manometer readings at the first appearance of Korotkoff sounds (phase I) is noted as systolic blood pressure and the pressure at which the sound disappears (phase V) was recorded as diastolic blood pressure. The measurements were repeated after 30 seconds of rest. Three blood pressure readings were recorded. The average of second and third reading was taken as systolic and diastolic blood. Echocardiographic Methods(12, 13): Echocardiography was performed using iE Philips Sonos system with the subject lying down in left lateral decubitus position. Mitral flow velocities were recorded within the apical 4-chamber or apical long axis view to determine the left ventricular filling hemodynamics. Evelocity, A- velocity and E/A ratio, were measured. The Doppler cursor was placed parallel to mitral inflow and maximum velocity measured with the sample volume at the mitral valve leaflet tips. The mitral peak E- wave (early filling) and A- wave (inflow with atrial contraction) were measured offline and E/A ratio was calculated.
Statistical Analysis
Statistical analysis was carried out using SPSS version 16.0. The baseline characteristics of the Study population to the baseline blood pressure was investigated using the student’s t-test. For parametric data, the level of significance between normotensive and prehypertensives groups was tested by unpaired student’s t-test.
RESULTS
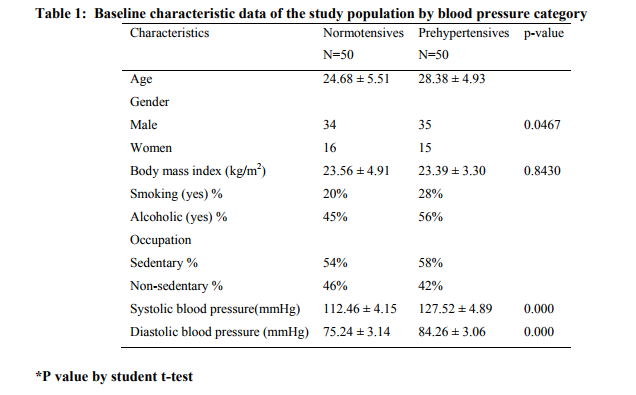
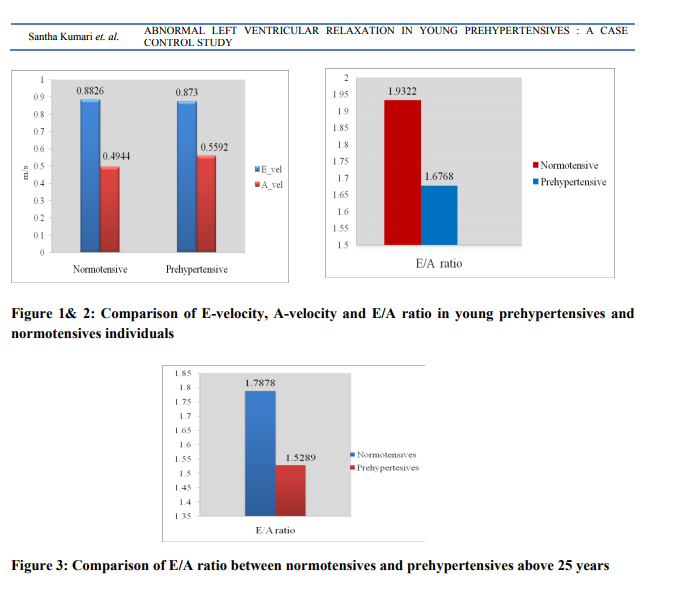
Our study group consisted of 100 subjects between 18- 35 years of age of both gender. Among fifty prehypertensives, 35 subjects (70%) were men and 15 subjects (30%) were women. Fifty normotensives were controls, 34 (68%) were men and 16 (32%) were women. The mean age was 24.6 years for normotensives and 28.38 years for prehypertensives. The mean body mass index (BMI) in prehypertensives and normotensives were 23.39 kg/m2 and 23.56 kg/ m2 respectively. In prehypertensives 58% were sedentary workers and 42% of them were non sedentary workers. In normotensives 54% were sedentary workers and 46% were non sedentary workers. There were 28% smokers in prehypertensive group compared to 20% smokers in normotensive group. 56% of prehypertensives and 45% of normotensives were alcoholic. The mean systolic and diastolic blood pressures in prehypertensives were 127.52 mmHg and 84.26 mm Hg respectively and mean systolic and diastolic blood pressures in normotensives were 112.46 mm Hg and 75.24 mm Hg respectively (Table 1). When compared with normotensives, in the prehypertensive group it is observed that E-velocity did not show significant difference between prehypertensives and normotensives with a p value of 0.785 (>0.05). The comparison of A- velocity between normotensives and prehypertensives shows a significant difference with p-value of 0.031 (<0.05) and the E/A ratio was significantly decreased with p= 0.05 (Figure 1 and 2). When E/A ratio was compared between 25- 35 years, a significant difference between prehypertensives and normotensives with a p= 0.0234 was observed (Figure 3).
DISCUSSION
Prehypertension is a risk factor for developing hypertension and is associated with subclinical cardiovascular disease. The present study was undertaken to compare the left ventricular diastolic function of young normotensive and prehypertensive adults. Diastolic mitral flow flow velocity pattern was used to estimate left ventricular diastolic function. Our study demonstrated significant left ventricular diastolic function abnormalities in prehypertensive adults. Mean age of prehypertensive subjects and normotensives were 28.38 years and 24.6 years respectively. Fischer et al (14) reported that the prevalence of diastolic function abnormalities in general population which varied according to age from 2.8% in individuals aged 25-35 years to 15.8% among those older than 65 years. In our study increase in age was associated with diastolic function abnormalities. Since mean age of prehypertensive group was higher than normotensive group it can be argued that higher mean age in prehypertensive subjects per se resulted in diastolic abnormalities in this group. When subjects with age more than 25 years were considered, prehypertensives and normotensives had comparable mean age of 30.25 years and 29.65 years respectively and it was demonstrated that there was significant diastolic function abnormalities in prehypertensives. The above finding indicates that even after age- adjustment, there was significant left ventricular diastolic abnormality in prehypertensives group. In both prehypertensives and normotensives, there were more male participants than female participants. There have been fewer gender comparison studies of diastolic left ventricular function. In the Framingham study, mitral flow velocity ratios were similar between men and women. One study did find lower absolute peak velocities in middle aged women, which may be consistent with diastolic dysfunction. In our study there was no significant gender difference between prehypertensives and normotensives. Many studies have demonstrated a strong correlation between BMI and diastolic function abnormalities (15, 16) . Valocic et al (17), in his study of 260 patients did not find any relation between BMI and diastolic function abnormalities. The mean BMI in prehypertensives and normotensives were 23.39kg/m2 and 23.56 kg/ m2 respectively. Of which, 52% of prehypertensives had normal BMI, 6% were under weight and 28% were obese. BMI was normal in 46% of normotensives, 6% were under weight and 28% were obese. Our study did not show any relation between elevated BMI and left ventricular relaxation. Stork T. et al (18) demonstrated significant LV diastolic function abnormalities in cigarette smoking independently of its role as a risk factor for coronary atherosclerosis. Ahmet Yilmaz et al (19), studied diastolic function in 69 smokers (mean age: 30 – 4.9 years) and compared with 30 non-smokers (mean age: 31.4 – 4.8 years) and demonstrated that E/A ratio, was significantly (p < 0.001) abnormal in smokers as compared to normal subjects There were 28% smoker in prehypertensive group as compared to 20% in normotensive group in our study and there was no significant differences in any of the diastolic function parameters. Lazarevic AM et al (20) demonstrated impaired LV relaxation in chronic asymptomatic alcoholic patients. In our study 56% prehypertensives and 45% normotensives were alcoholics and there was no significant diastolic function abnormalities detected in these groups. Previous studies have shown that diastolic function abnormalities were common among sedentary males and females and our study demonstrated significantly prolonged left relaxation in sedentary prehypertensives (21) . Kim SH et al (22), demonstrated early abnormalities of left ventricular diastolic function in middle- aged Korean adults with prehypertension
Comparison of E- velocity and A- velocity in normotensive and prehypertensive subjects When left ventricular wall becomes stiff, increasing the back pressure as it fills slows the early (E) filling velocity, thus lowering E/A ratio. The reversal of the E/A ratio less than 1 (A velocity becomes greater than E velocity) is often accepted as a marker of diastolic dysfunction in older adults. It was also noted that there was a reduction in E velocity and rise in A velocity among the prehypertensives with changes in E velocity being insignificant and changes in A velocity being significant (p< 0.05). When compared to normotensive group the E/A ratio were significantly lower in young prehypertensive subjects. However, reversal of E/A ratio which is common finding in older adult was seen only in 4 (8%) prehypertensive subjects. Advanced changes in left ventricular relaxation is likely to set in older adults due to more worsening of structural changes in the left ventricle due to hypertension and age related physiological changes.
CONCLUSION
This study showed non invasive assessment of transmitral flow velocity by Doppler echocardiography and allows early identification of diastolic abnormalities among prehypertensive individuals. Prehypertension is a warning sign. It means that the prehypertensives are at a greater risk of developing high blood pressure related complications. Early identification of prehypertension complications like prolonged left ventricular relaxation in young age group may prevent or postpone the more severe complication. Further studies are required to confirm the benefits of lifestyle modifications and therapeutic interventions in young prehypertensive subjects.
ACKNOWLEDGEMENT
I would like to express my sincere gratitude to Dr. Manimarane A. DM (Cardiologist), for the continuous support of my research, for his patience, motivation, enthusiasm, and immense knowledge. I also acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors /publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
REFERENCES
1. Deepa R, Shanthirani CS, Pradeepa R, Mohan V. Is the ’rule of halves’ in hypertension still valid? Evidence from the Chennai Urban Population Study. J Assoc Physicians India 2003; 51: 153-7.
2. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: National High Blood Pressed Education Program coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA. 2003;289:2560–72. [PubMed]
3. Yadav S, Boddula R, Genitta G, Bhatia V, Bansal B, Kongara S, et al. Prevalence and risk factors of pre-hypertension and hypertension in an affluent north Indian population. Indian J Med Res. 2008;128:712–20. [PubMed]
4. Anand Chockalingam AB, Patterns and predictors of prehypertension among health urban adults in India. Angiology 2005 sep-oct; 56(5):557-63.
5. Iriarte MM, Perez Olea J, Sagastagoitia D, Molinero E, Murga N. Congestive heart failure due to hypertensive ventricular diastolic dysfunction. Am J Cardiol.1995 Nov 2; 76(13):43D-47D
6. Fouad FM. Left ventricular diastolic dysfunction in hypertensive patients, Circulation, 1987:75 (Suppl.1) 148-155.
7. Ike SO, Ikeh VO, The prevalence of diastolic dysfunction in adult hypertensive Nigerian. Ghana Med.J.2006:40(2):55-60
8. Thomas JD, Weyman AE. Echocardiographic Doppler evaluation of left ventricular diastolic dysfunction. Physics and physiology. Circulation.1991; 84:997.-1002
9. Myreng Y, Smiseth OA. Assessment of left ventricular relaxation by Doppler echocardiography. Circ. 1990; 81:260.
10. Appleton C.P., Hatle L.K., Popp R.L., Relation of transmitral flow velocity patterns to left ventricular diastolic function. New insights from a combined hamodynamic and Doppler echocardiography study. J Am Cardiol.1988; 12:426-440.
11. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G, National kidney foundation. National kidney foundation practice guidelines for chronic kidney disease: evaluation, classification and stratification. Ann Intern Med 2003; 139:137-147.
12. Elaine M. Urbina, Philip R. Khoury, Connie McCoy, Stephen R. Daniels, Thomas R. Kimball, and Lawrence M. Dolan, Cardiac and Vascular Consequences of Prehypertension in Youth. J Clin Hypertens (Greenwich). 2011 May; 13(5): 332-342. doi:10.1111/j.1751-7176.2011.00471.
13. Roelandt J.R.T.C., M. Pozzoli. Non-Invasive Assessment of Left Ventricular Diastolic (Dys) function and filling pressure.
14. M. Fischer, A. Baessler, H.W. Hense, C. Hengstenberg , M. Muscholl, S. Holmer, A. Doring, U. Broeckel, and H. Schunkert , Prevalence of left ventricular diastolic dysfunction in the community. Results from a Doppler echocardiographic-based survey of a population sample. Eur Heart J (2003) 24 (4): 320-328.
15. HartCY, Redfield MM. Diastolic heart failure in the community. Curr Cardiol Rep.2000; 2:461- 469
16. Kuch B, Hense HW, Gneiting B, et al. Body composition and prevalence of left ventricular hypertrophy. Circulation.2000; 102:405-410
17. Valocik G, Mitro P, Zapachova J, Majercak I, Mudrakova K. Relation of various body mass index to systolic abd diastolic dysfunction. Bratisl Lek Listy 2008; 109(2) 52-56
18. Stork T, Eichstadt H, Mmockel M , Bortfeldt R, Moller, R Hochrein H . Changes of diastolic function induced by cigarette smoking: An echocardiographic study in patients with coronary artery disease. Clin Cardiol. Vol. 15, February 1992
19. Ahmet Yilmaz, Kenan Yalta, Okan Onur Turgut, Mehmet Birhan Yilmaz, Alim Erdem, Filiz Karadas, Ali Ozyol and Izzet Tandogan. The effect of smoking on cardiac diastolic parameters including Vp, a more reliable and newer parameter Cardiology Journal 2007Vol. 14, No. 3, pp. 281-286
20. Lazarevic AM, Nakatani S, Neskovic AN, Marinkovic Y, Yasumura Y, Stojicic D, Miyatake K, Bojic M, Popovic AD. Early changes in left ventricular function in chronic asymptomatic alcoholics: relation to the duration of heavy drinking. J Am Coll Cardiol. 2000 May; 35(6):1599-606.
21. Louise Bennet, Charlotte Larsson, Marianne Söderström, Lennart Råstam, and Ulf Lindblad. Diastolic dysfunction is associated with sedentary leisure time physical activity and smoking in females only. Scand J Prim Health Care. 2010; 28(3): 172-178.
22. Kim SH, Cho GV, Baik I, Lim SV, Choi CU, Lim HE, Kim EJ, Park CG, Park J, Kim J, Shin C. Early abnormalities of cardiovascular structure and function in middle-aged Korean adults with prehypertension: The Korean Genome Epidemiology study. Am J Hypertens. 2011 Feb; 24(2):218-24.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License