IJCRR - 6(6), March, 2014
Pages: 33-35
Print Article
Download XML Download PDF
TUBERCULOSIS OF THE BREAST, AN UNCOMMON DISEASE-A CASE REPORT
Author: N. Murugesan, K. Natarajan, V.S. Ananthan
Category: Healthcare
Abstract:The aim of studying this patient with tuberculosis of the breast is to highlight the diagnostic difficulties posed by this rare disease which mimics many other serious conditions because of its multifaceted presentation. The patient under study presented with a firm mass in her right breast. Biopsy of the lump confirmed the diagnosis of tuberculosis, as it is important to rule out carcinoma of the breast. Finding the typical tubercular granuloma on histopathological examination settled the issue. Tuberculosis of the breast is more common in young women and it usually presents as a mass, recurrent chronic abscess, ulcer or a sinus. A high index of suspicion and awareness of the varied presentation of the disease will help not to miss the diagnosis.
Keywords: Tuberculous mastitis, Acid fast bacillus
Full Text:
INTRODUCTION
Tuberculosis of the breast is not very rare (1). The presentation of this disease is variable. Most often it can be mistaken for carcinoma, fibrocystic disease or abscess of the breast. The confirmatory test is the demonstration of the acid fast bacilli or typical granuloma in the lesion. As HIV infection is on the rise globally tuberculous mastitis may also correspondingly increase in incidence.
CASE REPORT
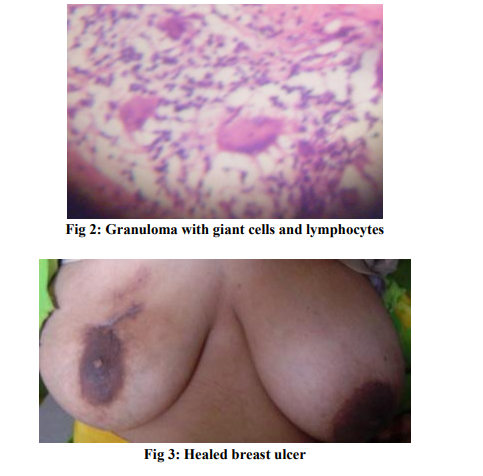
A 27 year old female patient presented with a two month history of a painless lump in the right breast which was gradually increasing in size. She had evening rise of temperature. There was no discharge from the nipple. She gave no history of loss of weight or loss of appetite. There was no history of similar complaints in the past. She had no previous history of tuberculosis. On examination she was not anemic, no generalized lymphadenopathy. Blood pressure and pulse were normal. Respiratory and other systems were normal. Examination of the right breast revealed a non tender firm lump 3 x 2 cm size in the upper half just above the areola at 12 o clock position. It was freely mobile and not attached to skin or the deeper structures. Her left breast was normal. There was no axillary or cervical lymphadenopathy. Blood Investigations revealed normal haemoglobin, and normal white cell count and differential count. ESR was 45mm at half hour 85mm in one hour. Mantoux skin test was negative. Sputum for AFB was negative. Blood Sugar was - Fasting 88mg, Post prandial 178mg. Chest x-ray was normal. FNAC of the breast lump revealed inflammatory cells and was negative for AFB and fungus mycelia. It did not produce any growth on culture. She had no relief after a prolonged course of Broad spectrum Antibiotics. The breast lump became semi fluctuant and hence incision and drainage of the abscess were done. She developed multiple sinuses in and around the area of incision and drainage and the swelling further increased in size (Fig 1). Then, under GA, excision of the breast lump and surgical debridement were done. Histopathology of the right breast lump was reported as TB granuloma. She was started on Anti Tubercular Treatment with 4 standard drugs namely HREZ. She had excellent response after 2 months of intensive phase treatment. The discharge from the sinuses stopped and all sinuses healed after six months of anti tuberculosis treatment.
DISCUSSION
Sir Astley Cooper was the first to describe tuberculous mastitis as "scrofulous swelling in the bosom of young women" in 1829(2). Tuberculous mastitis is not very rare. The mammary tissue is relatively immune to tuberculous infection like skeletal muscle and spleen (3). India has a high incidence of tuberculosis (4). Even though tuberculosis of the breast is not uncommon in the developing world, it is becoming common in the developed world due to increase in the number of immunocompromised patients (5). In spite of this, the disease is not often reported. The reason may be that this condition presents in a variety of ways. It is usually confused with fibroadenoma or carcinoma (6). This may also present as an abscess, a chronic sinus, fistula or a fungating ulcer. It may or may not be associated with pulmonary or other extra pulmonary tuberculosis. It is postulated that the route of infection to the breast might be retrograde spread from the axillary or mediastinal nodes. It is also possible that the disease may directly spread from a suckling infant. Gupta et al. found a correlation between prevalence of tuberculosis in the faucial tonsils of suckling infants and higher incidence of tuberculosis in lactating women (7). Definitive diagnosis can be made by a positive culture or presence of AFB bacilli on staining. In our patient, even though AFB was not demonstrated in FNAC, typical granuloma was seen on histopathological examination (Fig 2). The patient had an excellent response to anti tuberculosis therapy (Fig 3).
CONCLUSION
India has a very high incidence of pulmonary and extra pulmonary tuberculosis. Tuberculosis of the breast is not uncommon. It poses diagnostic difficulties because of its varied presentation and similarities to various other conditions. When it presents as a mass then malignancy has to be excluded by excision biopsy. Presence of tubercular granuloma will clinch the diagnosis.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. The authors are grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript.

References:
REFERENCES
1. Kalac N, Ozkan B, Bayiz H, Dursun AB, Demirag F. Breast tuberculosis. Breast 2002; 11: 346-9.
2. Cooper A. Illustrations of the diseases of the breast. Part I. Longmans. Orme, Brown and Green. London:1829; 73
3. Mukerjee P, George M, Maheshwari HB, Rao CP. Tuberculosis of the breast. J Indian Med Assoc 1974;62 : 410-2.
4. WHO global tuberculosis report 2013 www.who.int/tb/data
5. Kervancioglu S, Kervancioglu R, Ozkur A, Sirikci A. Primary tuberculosis of the breast. Diagn Interv Radiol 2005; 11:210-2.
6. Graunsman RI, Goldman ML. Tuberculosis of the breastreport of nine cases including two cases of co-existing carcinoma and tuberculosis. Am J Surg 1945; 67 : 48.
7. Gupta R, Gupta AS, Duggal N. Tubercular mastitis. Int Surg 1982; 67:422-4
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License