IJCRR - 6(6), March, 2014
Pages: 26-32
Print Article
Download XML Download PDF
EFFECTIVENESS OF MITOMYCIN-C APPLICATION AS AN ADJUNCT IN SURGERIES FOR RECURRENT PTERYGIUM - A META ANALYSIS
Author: Narendra P. Datti, Nagesha C. K., Rashmi N. R., Shalini
Category: Healthcare
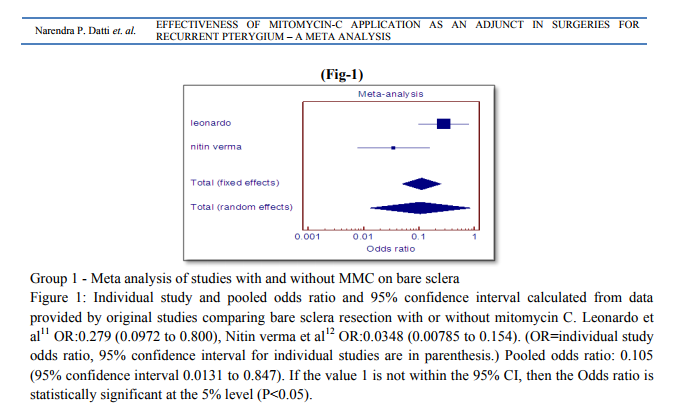
Abstract:Background: Recurrent pterygium poses distinct problem like high postoperative recurrences and many surgical approaches have been tried to decrease recurrences. Currently, mitomycin C (MMC) application and amniotic graft are used as adjunct apart from the standard limbal-conjunctival autograft. Aim of study: Aim of this study is to determine through meta-analysis, the risk of recurrences and frequency of post operative complications associated with MMC application over bare sclera or along with amniotic graft for recurrent pterygia. Method: A thorough search of online resources for randomised controlled clinical trials comparing bare sclera technique with or without MMC and amniotic graft with or without MMC application was done. The purpose was to determine the pooled odds ratio and 95% confidence interval for post operative pterygium recurrence. Results: Among 5 studies, 2 studies comparing bare sclera technique with or without MMC showed pooled odds ratio of 0.105 with 95% CI 0.0131 to 0.847. Study comparing amniotic graft with or without MMC showed odds ratio 0.298 with CI of 0.0817 to 1.089. Conclusion: Application of MMC on bare sclera reduced recurrence rate to 10% and on amniotic graft it reduced to 30% with no added serious complications.
Keywords: Mitomycin-C, Amniotic graft, Bare sclera, Recurrent pterygia, Meta-analysis.
Full Text:
INTRODUCTION
Pterygium is a fibrovascular growth arising from the conjunctiva onto the cornea. A number of surgical techniques have been described for primary pterygium excision including bare sclera technique1 , bare sclera resection with mitomycin-c (MMC) application2 , conjunctival autograft3 and recently amniotic membrane grafts4 . The treatment with these adjuncts have significantly reduced but not eliminated the problem; as far as the recurrent pterygium is concerned, there are greater challenges associated with treatment5 . Added to high recurrence rate, is the problem of deciding on the best approach of its surgical excision, since a recurrent pterygium is usually associated with subconjunctival fibrosis and/or corneal thinning and scarring. Mitomycin-C is an antitumor agent that acts by inhibiting DNA synthesis. The mechanism of action seems to be inhibition of fibroblast proliferation at the level of episclera6 . Adjunct MMC for pterygium surgery was first described by Kunitomo and Mori7 in Japan in 1963 and in US by Singh et al8 in 1998 as postoperative topical MMC with concentration of 0.4-1mg/ml. At present, MMC is being mainly used after pterygium excision as an intraoperative application to bare sclera for the management of both primary and recurrent pterygium.9 In order to further reduce the recurrence and postoperative complications, an intraoperative MMC treated sclera is normally covered with a conjunctival or amniotic membrane graft4 . Despite the fact that studies on MMC have shown rare but significant conjunctival, scleral, and corneal toxicity10, its use as an adjunct in primary or recurrent pterygia surgeries seems to be beneficial in few randomised clinical trials11-15 . We conducted a Meta-analysis of published randomised clinical trials analysing the recurrence rates and frequency of postoperative complications with MMC application over bare sclera or along with amniotic graft for recurrent pterygia. The purpose of this study was to determine the pooled odds ratio and 95% confidence intervals for postoperative pterygium recurrence.
MATERIALS AND METHODS
Selection strategy and selection criteria Following an established protocol, a survey of published studies comparing at least two of the three surgical techniques in the treatment of recurrent pterygium – bare sclera resection, bare sclera resection with MMC application and amniotic membrane transplantation with MMC – was conducted through an electronic search. We have not analysed technique of limbalconjunctival autograft with MMC here, because of paucity of Randomised Controlled Trials analysing its effect with or without MMC for recurrent pterygium surgery. Randomised controlled trials (RCTs) that compared above mentioned techniques and reported recurrence rates and post operative complications were included. Exclusion criteria included non-randomised, non-controlled trials, studies with other adjunct techniques and unpublished data. Clinical trials were identified through (1) Electronic search of PUBMED, Science direct, MD consult, Google scholar, MEDLINE and EMBASE. (2) Manual searches of the reference list of original article reports through electronic search. Searches were conducted using the keywords “recurrent pterygium”, “Mitomycin-C”, “Amniotic membrane”. The computerised search covered the period from 1980 to October 2013. Two reviewers (N.D and C.K.N) confirmed study eligibility and extracted data independently, and data were pooled using standard Meta-analysis techniques.
RESULTS
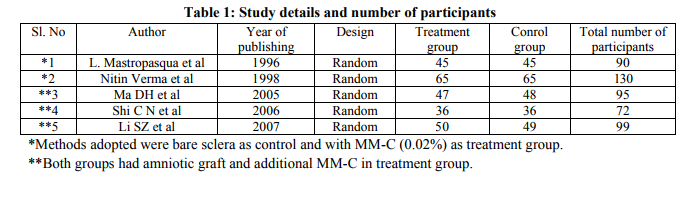
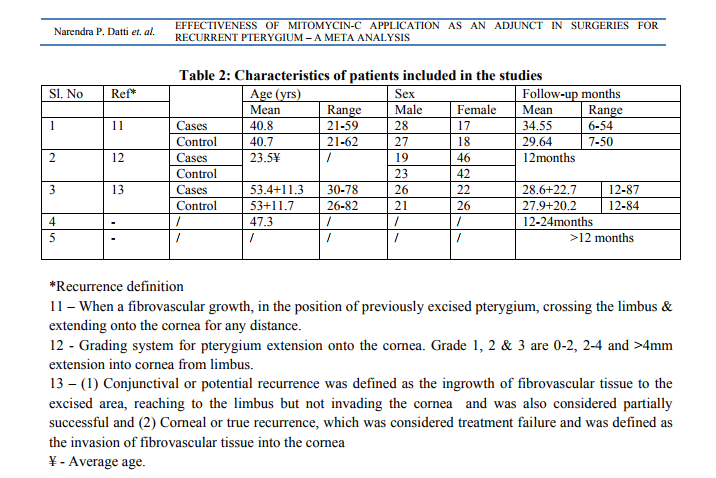
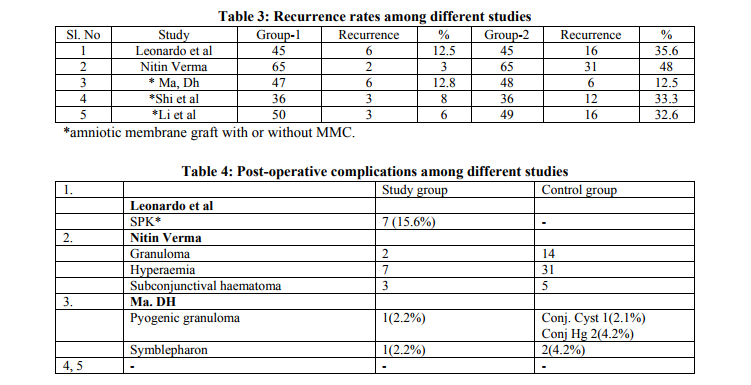
Total five eligible studies were identified, two that compared bare sclera resection with or without MMC application11,12, three studies that compared amniotic graft placement with or without MMC13,14,15. For statistical analysis and to maintain homogenicity in studies, 5 studies were divided into 2 groups. 1st group consisted of two studies of bare sclera technique with or without MMC and 2nd group with three studies consisting of amniotic membrane transplantation with or without MMC. Table 1 provides characteristics of clinical trials comparing mitomycin C on bare sclera and on amniotic graft. Table 2 provides a description of the population characteristics of studies included, follow-up periods and recurrence definition. Table 3 and 4 show recurrence rates and complications encountered in different surgical techniques. 3 studies were from English literature and 2 studies from Chinese literature. Full text was available in 3 studies and in 2 studies, only abstract was available. The results of meta-analysis showed that recurrence rate of bare sclera with MMC were 8% which was lower than bare sclera alone group with 47% recurrence rate. Amniotic Membrane Graft with MMC group was associated with lower recurrence rate (9%) compared to AMG group alone (25.5%). Heterogenecity was found between the studies in group 1 and group 2. In group 1, Q=5.2422 with significant P value (p=0.0220) and in group 2, Q=5.9912 with significant P value (p=0.05). The heterogenecity between the studies were taken into consideration and analysed with due care by random effect analysis of raw data. Narendra P. Datti et. al. EFFECTIVENESS OF MITOMYCIN-C APPLICATION AS AN A
DISCUSSION
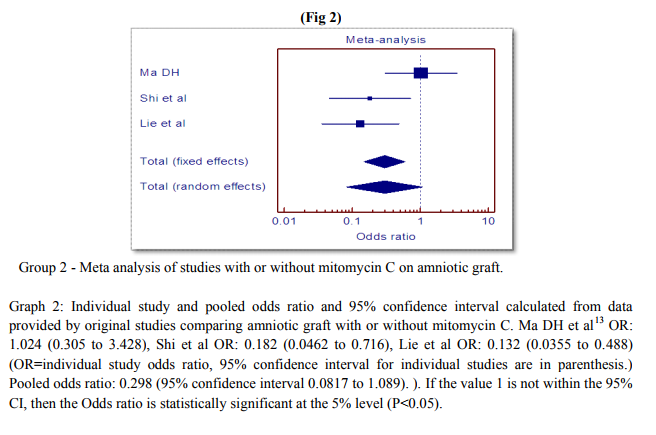
Pterygium, a worldwide degenerative corneal disease with multifactorial etiology, is particularly common in tropical and subtropical countries.16 Although different treatment regimens have been proposed for the treatment of pterygium, the main complication of pterygium treatment is recurrence.17,18 Recurrent pterygium is more difficult to control, and various treatment modalities including radiotherapy19, antimetabolite or antineoplastic drugs2 , conjunctival flap3 , and conjunctival or limbal autograft transplantation have been proposed. 4 Now a days, conjunctival10 or limbal autografts and amniotic membrane transplants5 have been commonly used alone or combined with MMC11 as adjuvant treatment for recurrent pterygium. Use of antimetabolites, especially intraoperative administration of MMC, may be performed in conjunction with amniotic membrane transplantation.13,14 Covering bare sclera with amniotic membrane may decrease the risk of scleral ulcer formation as a late complication with the use of antimetabolites.20,21 This study provides evidence of the inherent risk of pterygium recurrence after excision of recurrent pterygium with or without mitomycin C application over bare sclera or amniotic graft. Analysis of group 1 studies showed that for every 100 recurrences in bare sclera alone group, there were only 10 recurrences with application of MMC with a 95% confidence interval of 0.0131 to 0.847 (Pooled OR=0.105). These results show dramatic change in recurrence rate with MMC application.(Graph:1) Analysis of group 2 studies showing role of MMC on amniotic grafts in preventing recurrences, showed pooled odd’s ratio of 0.298 with 95% confidence interval of 0.0817 to 1.089. This implies for every 100 recurrences in Amniotic Membrane Graft alone group, there were only 30 recurrences if MMC was added in AMG. Only one study13 revealed no difference with addition of MMC compared to Amniotic Membrane Transplant alone. The association between exposure (MMC) and control group (AMG alone) was less strong compared to group 1 studies but still carried high significant value in terms of recurrence rates.(Graph:2) We have found that bare sclera or AMG augmented with MMC was associated with a lower recurrence rate than either of it alone in recurrent pterygium surgeries. An interventional prospective case series comparing limbal-conjunctival autograft (L-CAT) with or without MMC showed least recurrence rate in MMC group.16 L-CAT theoretically is a natural substitute to cover bare sclera and hence associated with low recurrences but recurrent surgeries on conjunctiva pose difficulties in harvesting healthy conjunctival graft. We have not analysed this technique here because of paucity of RCTs analysing its effect with or without MMC for recurrent pterygium surgery. As per complications are concerned, Superficial punctate keratitis was found in only one study in MMC group. Otherwise the mentioned complications (table 4) are nonspecific and do not seem directly related to the effects of MMC. Moreover these complications are more in control group than treatment group suggesting protective role of MMC in preventing complications other than recurrences. There are many case series, prospective studies and reports of complications arising from MMC application21-24; no such serious complications like scleral or corneal melt were reported in our study group. The reason could be difficult to analyse but needs more data to conclude these findings. As per quality assurance and strength of studies is concerned, heterogenecity was found, which do weaken the result. Things like unpublished data, research in langauge other than English, Chinese and publication bias might appear like an island in a sea of darkness which may partly make the analysis incomplete. Hence, we tried doing a good home work before interpreting the findings.
CONCLUSION
To summarise, this is the first ever Meta analysis done, analysing the surgeries for recurrent pterygium using MMC as adjuvant. From above analysis, it is clear that MMC application over bare sclera stood highly scientific and rationale. So, we should strongly discourage bare sclera technique alone in a recurrent pterygium surgery. This fact is more or less well established from other meta analyses which tested MMC effectiveness on primary pterygium surgery.25,26 With respect to the surgeries with amniotic graft concerned, addition of MMC as an adjunct overweighs advantages compared to complications per se due to MMC. Hence, MMC is strongly recommended in high risk groups. There appears to be low magnitude of recurrence both in control and cases of group 2 studies. Here, amniotic graft has major contribution in low recurrence but addition of MMC makes the figures encouraging. In this regard, new research should focus on long term effects of mitomycin-C in recurrent pterygium surgeries.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
REFERENCES
1. D’Ombrain. The surgical treatment of pterygium. Br J ophthalmol 1948;32:65-71.
2. Singh G, Wilson CS, Foster CS. Mitomycin eye drops as treatment for pterygium. Ophthalmology1998;95:813-21.
3. Kenyon K, Wagoner MD, Heltinger ME. Conjunctival autograft transplantation and recurrent pterygium. Ophthalmology1985;92:1461-70.
4. Katrircioglu YA, Altiparmak VE, Duman S. comparison of three methods for the treatment of pterygium: amniotic membrane graft, conjunctival autograft, and autograft plus mitomycin C. orbit.2007;26:5-13.
5. Shimazaki J, Shinozaki N, Tsubota K. transplantation of amniotic membrane and limbal autograft for patients with recurrent pterygium associated with symblepharon. Br J.ophthalmol.1998;82:235-240.
6. Donnenfeld ED, Perry HD, Wallerstein A, et al. Subconjunctival mitomycin c for the treatment of ocular cicatricial pemphigoid. Ophthalmology.1999;106(1):72- 8;discussion79.
7. Kunitomo N, Mori S. studies on pterygium. Report N. A treatment of pterygium by mitomycin C instillation. Acta Soc ophthalmol Spn.1963;67:601-607.
. Singh G, Wilson MR, Foster CS. Mitomycin eyedrop as treatment for pterygium. Ophthalmology.1998;95(6):813-821.
9. Ang LP, Chau JL, Jan DT. Current concepts and techniques in pterygium treatment. Curr opin ophthalmol.1998;82:235-240.
10. Muthu FM, Sobaei G, Jatar T, Yildirim E. A comparitive study of recurrent pterygium surgery:limbal conjunctival autograft transplantation versus mitomycin C with conjunctival flap. Ophthalmologgy.1998;106(4):817-821.
11. Leonardo Mastropasqua, Paolo Carpineto, Marco Ciancaglini, Pier Enrico Gallenga. Long term results of intraoperative mitomycin C in the treatment of recurrent pterygium. British Jounal of Ophthalmology 1996; 80: 288-291.
2. Nitin verma1 , Jambi arringa garap1 , Rosilyn marisi and Apisai kerek1 . Intraoperative use of mitomycin C in the treatment of recurrent pterygium. PNG Med J 1998 Mar;41(1):37-42.
13. Ma DH, See LC, Hwang YS, Wang SF. Comparison of amniotic membrane graft alone or combined with intraoperative mitomycin C to prevent recurrence after excision of recurrent pterygia. Cornea. 2005 Mar;24(2):141-50.
14. Shi CN, Zhou GL. Application of mitomycin C in amniotic membrane traansplantation to treat recurrence pterygium. Cuangzhou Med J (chin)2006;37(5):37-39.
15. Li SZ. Effect analysis of amnion membrane transplantation combined with mitomycin C in the treatment of pterygium. J bethune military medical college (chin)2007;10(5):290-291.
16. Mohamed A Fakhry. The use of mitomycin C with autologous limbal-conjunctival autograft transplantation for management of recurrent pterygiumClinical Ophthalmology 2011:5 123–127.
17. Starck T, Kenyon KR, Serrano F. Conjunctival autograft for primary and recurrent pterygia: surgical technique and problem management. Cornea 1991;10:196 –202.
18. Mahar PS, Nwokora GE. Role of mitomycin C in pterygium surgery. Br J Ophthalmol 1993;77:433–5.
19. MacKenzie FD, Hirst LW, Kynaston B, Bain C. Recurrence rate and complications after beta irradiation for pterygia. Ophthalmology 1991;98:1776–80; discussion 1781.
20. Rubinfeld RS, Pfister RR, Stein RM, et al. Serious complications of topical mitomycin-C after pterygium surgery. Ophthalmology 1992;99:1647–54.
21. Dunn JP, Seamore CD, Ostler HB, Nickel BL, Beallo A. Development of scleral ulceration and calcification after pterygium excision and mitomycin therapy. Am J Ophthalmol 1991;112:343–4.
22. Rubinfeld RS, Pfister RR, Stein RM, Foster CS, Martin NF, Stoleru S et al. Serious complications of topical mitomycin-C after pterygium surgery. Ophthalmology 1992 Nov;99(11):1647-54.
23. Shabbir Saifuddin, Alaa El Zawawi. Scleral changes due to mitomycin C after Pterygium excision: A report of two cases. Indian J Ophthalmol 1995;43:75-6.
24. B Safianik, I Ben-Zion, and H J Garzozi. Serious corneoscleral complications after pterygium excision with mitomycin C. Br J Ophthalmol2002March;86(3):357-8.
25. Yin-Wei Song, Ai-Hua Yu, Xiao-Jun Cai. Effectiveness of amniotic membrane transplantation combined with mitomycin C in the treatment ofpterygium: a meta-analysis. Int J Ophthalmol2010;3(4):352-355.
26. Juan Camilo Sánchez-Thorin, Guillermo Rocha, Julie B Yelin. Meta-analysis on the recurrence rates after bare sclera resection with or without mitomycin C and conjunctival autograft placement in surgery for primary pterygium. Br J Ophthalmol 1998 82: 661- 665.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License