IJCRR - 6(7), April, 2014
Pages: 31-34
Print Article
Download XML Download PDF
FORAMINA TRANSVERSARIA 'BIPARTITA': A STUDY OF CERVICAL VERTEBRAE
Author: Gyata Mehta, Swapnali Shamkuwar, Varsha Mokhasi
Category: Healthcare
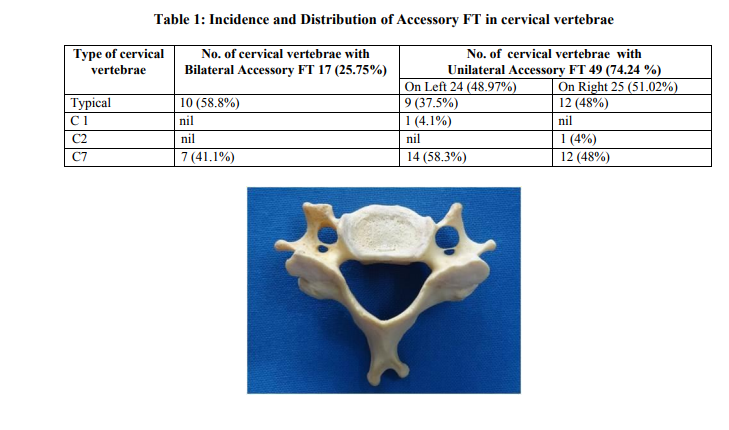
Abstract:Objectives: The Foramen Transversarium (FT) transmits the vertebral artery (except in C7 vertebra), vertebral veins and the sympathetic plexus that accompanies the vessels. The deformation and variation of this foramen may affect the anatomical course of vital vascular and neural structures and consequently cause pathological conditions. With the advent of newer surgical techniques for treatment of unstable cervical spine, awareness about morphological variations of cervical vertebrae and surrounding structures has become essential. Aim: Aim of the study was to find the incidence and distribution of accessory foramina transversaria in cervical vertebrae with emphasis on their embryological basis and surgical importance. Methods: Five hundred cervical vertebrae (typical and atypical) were collected from the Department of Anatomy. Each cervical vertebra was examined for the presence of accessory FT. They were also observed for the absence of FT. Results: It was observed that accessory FT was found in 66 (13.2 %) vertebrae. Amongst these 17(25.75%) showed accessory FT bilaterally and 49 (74.24%) showed accessory FT on one side only. There was no significant difference in the presence of accessory FT on the two sides. Absence of FT was not seen. Conclusions: Recognition of double FT has significant clinical importance as the course of vertebral artery may be distorted in such situations. It is of great relevance to neurophysicians, neurosurgeons and radiologists.
Keywords: cervical vertebrae, accessory Foramina Transversaria, vertebral artery.
Full Text:
INTRODUCTION
The cervical vertebrae are characterized by the presence of Foramen Transversarium (FT) in the transverse process. This foramen usually contains vertebral artery (except in C7 vertebra), veins and sympathetic plexus. The deformities and variations of this foramen may affect the anatomical course of vascular and neural structures and consequently cause pathological conditions. It may cause vertebrobasilar insufficiency as a result of neck movements. Compression of vertebral artery may result in headache, migraine and fainting attacks1 . Since vertebral and basilar arteries contribute to the blood supply of the inner ear, hence spasm of the same artery due to irritation of the sympathetic plexus, may be manifested not only by neurological symptoms but also by labyrinthine or hearing disturbances2 . Accessory FT is considered when the FT is anatomically divided by a fibrous or bony ridge and the smaller posterior part is called the accessory FT3 . Ambiguity persists about the content of this accessory FT, whether it is occupied by the vertebral vein or vertebral nerves or by a duplicate vertebral artery or both. The relations of these structures are of surgical importance in the posterior approach of the cervical spine.
MATERIAL AND METHODS
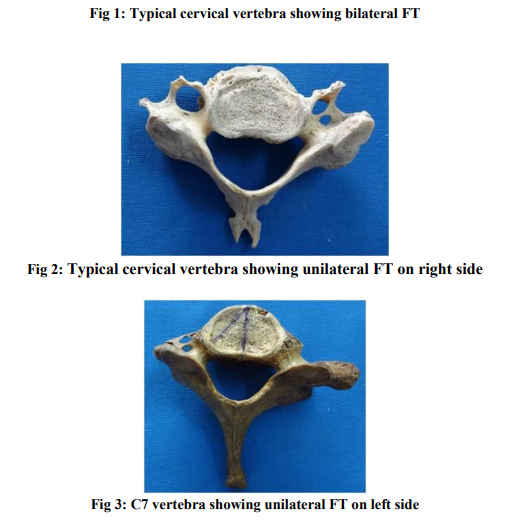
Five hundred cervical vertebrae were collected from the Department of Anatomy. Out of these, 177 were typical cervical vertebrae and 323 were atypical cervical vertebrae. Amongst the atypical cervical vertebrae, 106 were C1, 137 were C2 and 80 were C7. Each cervical vertebra was examined for the presence of accessory FT. They were also observed for the absence of FT. Photographs were taken and archived.
RESULTS
Out of the total 500 cervical vertebrae, Accessory FT was observed in 66 (13.2%) vertebrae. Amongst these 17 (25.75%) showed accessory FT bilaterally and 49 (74.24%) showed accessory FT on one side only. There was no significant difference in the presence of accessory FT on the two sides. It was observed that accessory FT was found more in C7 vertebrae and typical vertebrae and less frequently in C1 and C2 vertebrae.
DISCUSSION
The FT is the result of special formation of the cervical transverse process. It is formed by a vestigial costal element fused to the body and the originally true transverse process of the vertebra. The vertebral plexus and nervous plexus are caught between the bony parts4 . Many factors are involved in causing morphological variations of FT including developmental factors, mechanical stress, size and number of anatomical structures passing through5 . Since the vertebral vessels are a factor in the formation of the FT, it can be assumed that variation in the presence and course of the vessels will be manifested in changes in the FT. Conversely, variations of the FT can be useful for estimating change or variations of the vessels and accompanying nerve structures. The embryogenesis of the vertebral arteries occurs between day 32 and 40 of gestation. The paired vertebral arteries arises from longitudinal branches that link together to form a longitudinal vessel and secondarily lose their intersegmental connections to the aorta6 . It has been speculated that persistence of a portion of the primitive dorsal aorta with two intersegmental arteries may give rise to vertebral artery duplication. Failure on the regression of the inter segmental arteries can also result in vertebral artery fenestration7 . This fenestration may contribute to the development of double FT. Hence accessory FT is likely to be associated with anatomical variants of vertebral artery such as duplication and fenestration. Duplicated vertebral arteries have two origins and fusion points in the neck outside the spinal canal. Fenestrated vessels have single origin and divide into two parallel trunks within or outside the vertebral canal. Studies on accessory FT have been undertaken earlier. The occurrence rate ranged from 1.5%8 to 22.7%1 . Taitz et al reported double FT in 7% of vertebrae and triple FT (unilateral) in 0.2%2 . A study of typical cervical vertebrae showed the presence of double FT in 8% of vertebrae, more common in C6 vertebra3 . Another study showed total incidence of 1.6% with unilateral presence more than bilateral and more common in lower cervical vertebrae (C6 & C7)9 . The findings of the present study were consistent with the previous studies. Double FT were seen in 13.2% of vertebrae with higher prevalence of unilateral double FT(74.24%) as compared to bilateral double FT(25.75%).There was not much significant difference on the two sides. Absence of FT was not found, when compared to other studies showing bilateral absence of FT10 .
CONCLUSION
Knowledge of accessory FT is clinically significant as it may affect the course of vertebral vascular bundle and nerves causing symptoms to patients. Recognition of such variations is important particularly in posterior cervical surgery. It is of great relevance to neurophysicians, neurosurgeons and radiologists.
References:
REFERENCES
1. Kaya S et al. Double Foramen Transversarium Variation in Ancient Byzantine Cervical Vertebrae: Preliminary Report of an Anthropological Study. Turkish Neurosurgery 2011;21,534-538
2. Taitz C, Nathan H , Arensburg B .Anatomical observations of the foramina Transversaria. Journal of Neurology, Neurosurgery and Psychiatry;1978,41,170-176
3. Sharma A, Singh K, Gupta G, Srivastava S. Double foramen transversarium in cervical vertebrae an osteological study. J Anat.Soc.India 2010;59,229-231
4. Gray H. Development of vertebral column. Gray’s Anatomy. The Anatomical Basis of Clinical Practice, 40 th ed. Susan Standring, Elsevier Churchill Livingstone, London; 2008, p792-796
5. Jaffar AA, Mobarak HJ, Najm SA. Morphology of the Foramen Transversarium A Correlation with Causative Factors. AlKindy Col Med J 2004;2,61-64
6. William J Larsen. Development of vasculature. Human Embryology. 3 rd ed. Churchill Livingstone, London; p179-181
7. Sim E, Vaccaro AR, Berzlanovich A, Thaler H, Ullrich CG. Fenestration of the extracranial vertebral artery: Review of the literature. Spine 2001;26,139-142
8. Das Srijit, Suri R, Kapur V. Double Foramen Transversaria: an osteological study with clinical implications. Int Med J 2005;12,311- 313
9. Murlimanju BV et al. Accessory Transverse Foramina in the Cervical Spine: Incidence, Embryological Basis, Morphology and Surgical Importance. Turkish Neurosurgery 2011;21,384-387
10. Nayak S. Bilateral absence of foramen transversarium in atlas vertebra: a case report. Neuroanatomy 2007;6,28-29
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License