IJCRR - 6(8), April, 2014
Pages: 37-41
Print Article
Download XML Download PDF
OSSIFIED TRANSVERSE ACETABULAR LIGAMENT - AN OSTEOLOGICAL STUDY
Author: A. Perumal, S. Sathiya
Category: Healthcare
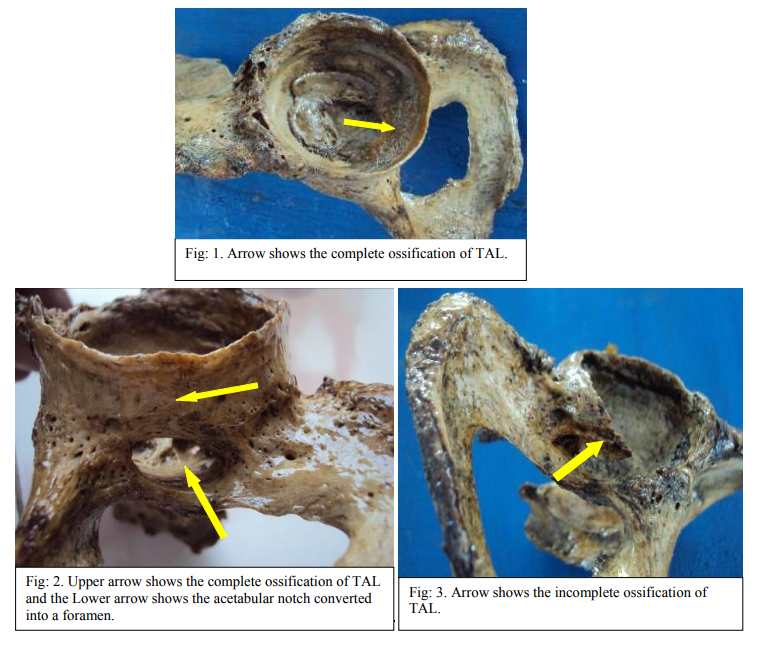
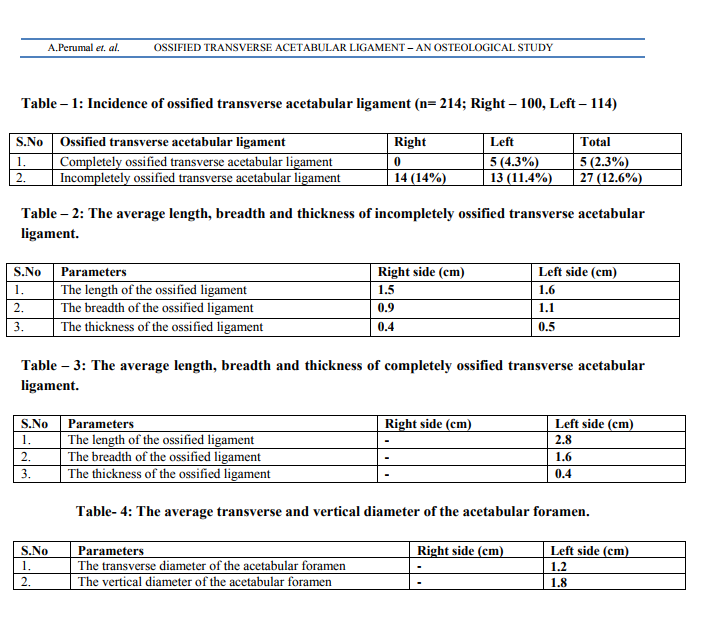
Abstract:Background: The ossification of transverse acetabular ligament is a rare interesting anatomical variation which converts the acetabular notch into a foramen. The transverse acetabular ligament (TAL) contributes to the stability of the joint. Sometimes the ligament gets ossified which limits the movement of hip joint and also leads to the compression of the nutrient vessel and subsequently result in ischemia of the area supplied by it. Ossification of the ligament as found in the present study may be helpful for the clinicians for differential diagnosis. Literature regarding the incidence, cause and clinical implications of this variation is therefore essential for radiologists, orthopaedicians and surgeons operating in the hip replacement surgery. The presence of ossified transverse acetabular ligament was noted and analyzed statistically. The study throws light on the incidence of the ossification of transverse acetabular ligament and discusses its clinical implications. Materials and Methods: Two hundred (214) dry human hip bones (right- 100 and left- 114) were taken for the study. The presence of ossified TAL was noted by macroscopic examination with naked eye. Results were tabulated and statistical analysis was done. Results: 4.3% of bones showed complete ossification of TAL on the left side hip bones and 14% of bones showed incomplete ossification of TAL on the right side and 11.4% on the left side hip bones. Conclusion: The knowledge of incidence of ossified TAL is essential for surgeons, orthopaedicians in performing the hip replacement surgery. The present study may be helpful for clinicians, radiologists and surgeons for differential diagnosis.
Keywords: Hip bone, transverse acetabular ligament, compression, incidence, clinical implication.
Full Text:
INTRODUCTION
The acetabulum of hip bone is a cup- shaped depression where the three components ilium, ischium, pubis meet and subsequently fuse. It receives the head of femur to form the hip joint. The peripheral margin of the acetabulum gives attachment to a fibro-cartilaginous rim. The two ends of the notch give attachment to the transverse acetabular ligament (TAL) and contribute to the stability of the joint. The gap between the ligament and the notch transmits acetabular branches of obturator and medial circumflex femoral vessels which supplies the acetabular fat and head of femur. But if the transverse acetabular ligament (TAL) gets ossified which converts the acetabular notch into a foramen. The ossified TAL limits the movement of hip joint and also leads to the compression of the nutrient vessel and subsequently results in ischemia of the area supplied by it1 . The ligamentum teres predominantly arises from the transverse acetabular ligament which is thickened, hypertrophied in patients with developmental dysplasia of the hip (DDH), in which repeated traction on the attachment of the ligament centrally leads to hypertrophy of transverse acetabular ligament, which in turn further decreases the size of the acetabular fossa and prevents reduction of the hip8 . The transverse acetabular ligament (TAL) can be used to orient the acetabular component during total hip arthroplasty10. Literature regarding the incidence, cause and clinical implications of this variation is therefore essential for radiologists, orthopaedicians and surgeons operating in the hip replacement surgery. The presence of ossified transverse acetabular ligament was noted and analyzed statistically. The study throws light on the incidence of the ossification of transverse acetabular ligament and discusses its clinical implications.
MATERIALS AND METHODS
Data for this study comprised of 214 hip bones (Right - 100 and Left - 114) irrespective of sex and age was conducted in the Departments of Anatomy, VMKVMC and VMHMC, Salem. Hip bone with acetabular damage will be excluded from the study. Each hip bone was examined macroscopically for the presence of ossified transverse acetabular ligament (complete or incomplete). The various parameters like length, breadth, thickness of the ossified TAL and incase of complete ossification of TAL the vertical and transverse diameters of the acetabular foramen were measured using the vernier caliper. The results were tabulated and analyzed statistically.
RESULTS
The results were presented in Table: 1, 2, 3 & 4. Complete ossification of the transverse acetabular ligament (Fig. 1, 2) was observed in 4.3% of bones (5 bones out of 114 hip bones) on the left side and on the right side no such ossification of ligament. Incomplete ossification of the transverse acetabular ligament (Fig. 3) was observed in 14% of bones (14 bones out of 100 hip bones) on the right side and on the left side it was 11.4% (13 bones out of 114 hip bones).
DISCUSSION
The labrum is a fibrocartilaginous rim which encompasses the circumference of the acetabulum, effectively deepening the socket and its basal surface attached to the acetabular bone and transverse acetabular ligament. The transverse acetabular ligament mainly gives stability and also it bridges the acetabular notch. The gap between the notch and the ligament transmits the acetabular branches of obturator and medial circumflex femoral vessels which supplies the acetabular fat and head of femur. When the ligament gets ossified leads to the compression of the nutrient vessel and subsequently results in ischemia of the area supplied by it1 . The incomplete ossification of TAL was more common on the right side hip bone than the left and the average values of length, breadth and thickness on the right were found to be 1.5cms, 0.9cms, 0.4cms respectively and on the left the average values were 1.6cms, 1.1cms, 0.5cms respectively (Table:2). The TAL ligament was completely ossified on the left side hip bone and the average value of length, breadth and thickness were found to be 2.8cms, 1.6cms, 0.4cms respectively (Table: 3). With complete ossification of the TAL the acetabular notch was converted into acetabular foramen and the average vertical, transverse diameters of the acetabular foramen were 1.2cms, 1.8cms respectively (Table: 4). Sharmila Bhanu et al2 described that one of the male pelvis showed bilateral ankylosis of sacroiliac joint, ossified sacrospinous ligament, sacrotuberous ligament and ossification of TAL on both sides. In their study, the length of the TAL was 3.6 cm on the right, 3.5 cm on the left side and maximum width of the ligament was 1.4 cm on the right and 2.1 cm on the left side hip bone. But in our study we observed 0.4% complete ossification of TAL on the left side bone and the average length, breadth was 2.8, 1.6cms respectively but no such variation was observed on the right side. The Anterior pelvic plane (APP) has been the cornerstone of image-based hip navigation technologies in which TAL was also used to predict the inclination and version of the acetabulum indirectly and when the ligament is ossified causing problems in registering bony land marks through the ossified ligament5,6. In open surgical hip dislocation the ligamentum teres capitis was separated at the level of its attachment into the transverse ligament and acetabular fossa9 . In case of ossified TAL there will be difficulties in performing this procedure. The present study reveals an incidence of ossification of TAL 4.3% of complete ossification on the left side and incomplete ossification of TAL 14% on the right and 11.4% on the left respectively (Table: 1).
CONCLUSION
Based on the present study, it was concluded that the ossified transverse acetabular ligament (TAL) interferes in the total hip replacement surgery. Hence the knowledge about the incidence of ossified TAL is essential for surgeons, radiologists, and orthopaedicians in performing the above procedure. The presence of ossified TAL can be revealed using Radiographic imaging which helps the surgeons to overcome the problems before performing the hip replacement surgery.
ACKNOWLEDGEMENTS
The authors sincerely wish to thank the management, administrators and the Professor and Head of the department of Anatomy of Vinayaka Missions Kirupananda Variyar Medical College, Salem for their whole hearted support and permissions to utilize their resources and conduct this study. The authors acknowledge the great help received from the scholars whose articles cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Authors are grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript.
References:
REFERENCES
1. Standring S. Gray’s Anatomy: Anatomical Basis of Clinical Practice. 39th Ed., London, Elsevier Churchill-Livingstone 2008; 1389– 1390.
2. Sharmila Bhanu P and Devi Sankar P. Bilateral ankylosis of sacro-iliac joint with ossified sacrospinous, sacrotuberous and transverse acetabular ligaments: a case report. International Journal of Anatomical Variations 2011; 4: 123–127.
3. Stefan Milz,Georgios Valassis, Andreas Buttner, Markus Maier, Reinhard Putz, James R. Ralphs, Michael Benjamin. Fibrocartilage in the transverse ligament of the human acetabulum. Journal of Anatomy 2001; 198: 223-228.
4. Archbold.B, Mockford.D, Molloy.J, McConway.L, Ogonda.D, Beverland. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement. British Editorial Society of Bone and Joint Surgery 2006; 88: 883-886.
5. Sam Hakki, Victor Bilotta, Janiel Oliveira, Luis dordelly. Acetabular Center Axis: Is It the Future of Hip Navigation?. Orthopaedics 2010; 33: 43-47.
6. A. Narvani, E. Tsiridis, C. C. Tai, P. Thomas. Acetabular labrum and its tears: Br J Sports Med 2003; 37: 207–211.
7. Daniel.J, Abramson, Samuel Kamberg, Jefferson Barracks, Missouri. Spondylitis, pathological ossification, and calcification associated with spinal-cord. The Jounal of bone and Joint Surgery 1949; 31-A: 275-283.
8. Luis Cerezal, Ara Kassarjian, Ana Canga, María Carmen Dobado, Juan Antonio Montero, EvaLlopis, Alejandro Rolon, Luis Perez-Carro. Anatomy, Biomechanics, Imaging and Management of Ligamentum Teres Injuries. RadioGraphics 2010; 30:1637– 1651.
9. Rafael J. Sierra, Robert T. Trousdale. Labral reconstruction using the ligamentum teres capitis. Clin Orthop Relat Res 2009; 467:753– 759.
10. Noah J. Epstein, Steven T. Woolson, Nicholas J. Giori. Acetabular Component Positioning Using the Transverse Acetabular Ligament. Clin Orthop Relat Res 2011; 469:412–416.
11. Sudsriluk Sampatchalit, Lina Chen, Parviz Haghighi, Debra Trudell, Donald L. Resnick. Changes in the Acetabular Fossa of the Hip: MR Arthrographic Findings Correlated With Anatomic and Histologic Analysis Using Cadaveric Specimens. AJR 2009; 193:127– 133.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License