IJCRR - 6(8), April, 2014
Pages: 14-17
Print Article
Download XML Download PDF
CHRONIC HEMIFACIAL SPASM - A MASQUERADER OF EPILEPSIA PARTIALIS CONTINUA
Author: Manigandan Gopi, Sunny D.A.N., Aashish Aarumugam
Category: Healthcare
Abstract:Hemi Facial Spasm (HFS) is commonly caused by compression of seventh cranial nerve by dolichoectatic arteries of posterior circulation though genetic and idiopathic causes to be considered1. Here we report a case of chronic HFS, A 55 years old female previously diagnosed to be HFS due to aberrant vascular loop compressing the facial nerve, on treatment for the past five years with no improvement in the symptoms. Patient EEG showed electrical activity in the right frontal lobe suggesting each spasm was due to partial seizure and diagnosis of Epilepsia Partialis Continua (EPC) was made. Patient symptoms resolved completely after starting newer anti convulsant medication suggesting that the facial spasms are due to EPC. Even though EPC is arising from cerebral cortex or sub cortical region it may present and to be mistaken as HFS - a peripheral movement disorder when it affects the face alone as in this case.
Keywords: Hemifacial spasm, Epilepsiapartialis continua
Full Text:
INTRODUCTION
Hemi facial spasm represents myoclonus of the muscles innervated by seventh cranial nerve. As the name suggests it occur unilaterally but bilateral involvement can also occur rarely. Though the ephaptic transmission theory2 and kindling theory3 suggests facial nerve dysfunction as the cause of hemifacial spasm the compression of facial nerve by posterior circulation vessels is considered to be the wide accepted cause of hemifacial spasm. Here we report a case of hemifacial spasm which on evalvuation showed epileptic discharge from right cerebral cortex as its cause which is unusual and reported very few in literature4-6 .
CASE REPORT
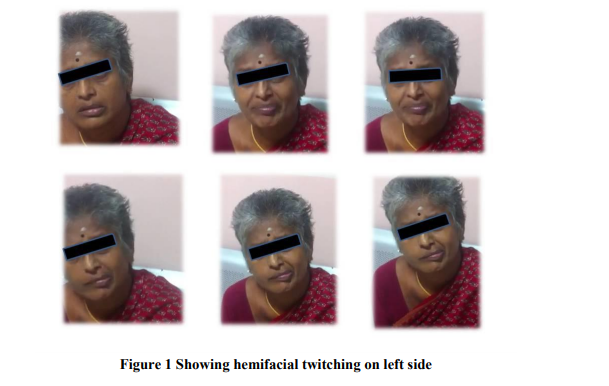
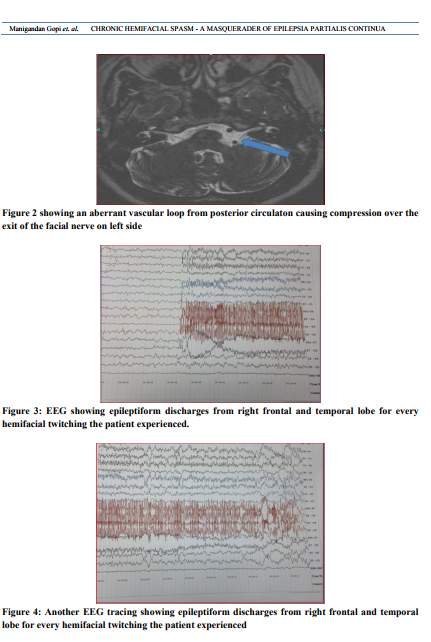
A 55-year-old-female was admitted and evaluated for an acute onset of Generalized tonic clonic seizure (GTCS) with post ictal confusion and 5 years history of facial twitching in left side (fig-1) with discomfort without pain. She had no prior illnesses. No history of head injury, meningitis / encephalitis or other precipitating events. There were no other abnormalities on the neurological or general examination. Brain MRI performed before 5 years at the onset of spasms and showed aberrant vascular loop from posterior circulaton causing compression over the exit of the facial nerve (fig- 2) and started on clonazepam as patient was allergic to carbamazepine. Inspite of therapy for one year patient symptoms didn’t resolve and she underwent botulinum toxin injection. Patient did not improve and advised for micro surgical decompression of facial nerve at the site of compression but patient was not willing for surgery and continued on clonazepam and baclofen. Patient now presented with GTCS and evalvuated for the same and repeat MRI brain did not reveal any new finding and EEG was taken which showed frequent epileptiform discharges from right frontal and temporal lobe (fig-3, 4) for every facial twitching which the patient had experienced and discharges from both the cortex when patient had GTCS suggesting secondary generalized seizure. Patient was allergic to carbamezipine, newer antiepileptics like levetiracetam and lacosamide provided almost complete resolution of facial twitching. When she temporarily discontinued the drugs due to sleepiness there was subsequent recurrence of these abnormal movements. The diagnosis of Epilepsiapartialis continua was confirmed by the finding of irregular epileptiform discharges from right cerebral hemisphere and rhythmic / semirhythmic focal slowing during prolonged video / EEG monitoring while the patient was experiencing Hemi facial spasm.
DISCUSSION
Epilepsiapartialis continua manifest as focal motor clonic seizures, which remain localized to the part of the body in which they originate (face / limbs) and the motor activity is persistent lasting for minute, hours, days, weeks or even years together7 . EPC can be considered the status epilepticus equivalent of simple partial motor seizures7 . In most cases of EPC the seizure focus lie on cerebral cortex eventhough subcortical foci have also been reported8 . Hemi facial spasm (HFS) is defined as unilateral, involuntary, irregular, clonic or tonic movement of facial muscles innervated by seventh cranial nerve.. Although most cases of hemifacial spasm are idiopathic and probably caused by vascular compression of facial nerve other etiologies like bells palsy, facial nerve injury by demyelination, vascular insult and hemifacial spasm mimickers should be considered. The hemifacial mimickers are classified as psychogenic, tics, dystonia, myoclonus and hemi masticatory spasm9 . In our case the mimicker has been identified as EPC. The ictal etiology for hemifacial spasm is evident from our case by the presence of electrical activity from the right frontal lobe for each facial twitching witnessed when EEG was taken and the prompt response to the antiepileptic drugs. It is further substantiated by the recurrence of twitching on withdrawl of the drug. The presence of aberrant vascular loop causing compression of the facial nerve made the previous clinician to think and treat as hemifaciaal spasm caused by vascular compression of facial nerve as it is the most widely accepted cause of hemifacial spasm. But the presentation of hemifacial spasm with GTCS made us to evalvuate for seizure and found that epileptic discharge from the right frontal lobe (partial seizure) present as facial twitching of the left side of face which is mistaken as hemifacial spasm due to clinical similarity and by the anatomic finding of aberrant vascular loop causing compression of the facial nerve. Since this partial seizure in our patient was persisitent for 4 years it is considered as Epilepsia partials continua. The EPC nature of HFC reported already in literature10 has a normal facial nerve course. In our case the patient had vascular compression of facial nerve and the cause for the facial twitching was not because of the compression but because of the Seizure activity is evidenced by the response from anticonvulsant medication and failure to respond for botulinumtox injection which is the commonest treatment for HFS of vascular compression of facial nerve11. Hence we hypothesize and emphasize that the prompt response of this patient with chronic HFS to newer antiepileptic drugs possibly indicate that HFS can occur sometimes as a manifestation of EPC with focal epileptiform discharge from the brain rather than due to facial nerve hyperexcitability.
CONCLUSION
We conclude that, Even though Hemifacial spasm is of neuropathic or idiopathic of origin, this case report should alert the physicians about the seizure activity from the cerebral cortex presenting as hemifacial spasm and EEG should be advised for all the cases of HFS irrespective of the MRI finding

References:
REFERENCES
1. Rahman, M.D. Ersalan; Jonathan D. Trobe, and Stephen S. Gebarski (June 2002). "Hemifacial Spasm Caused by Vertebral Artery Dolichoectasia". American Journal of Ophthalmology 133 (6): 854–855
2. Gardner, J.W.; Sava, Gerard A. (1962). "Hemifacial Spasm - A reversible pathophysiologic state". Journal of Neurosurgery 27 (3): 240–47.
3. Eby, Joesph; Sung Tae Cha,Hrayr K. Shahinian (2002). "Fully endoscopic vascular decompression of the glossopharyngeal nerve".The Journal of Craniofacial Surgery 13 (1): 90–95
4. Hogan RE, Rao VK. Hemifacial motor and crying seizures of temporal lobe onset: case report and review of electro-clinical localisation. J NeurolNeurosurg Psychiatry. 2006;77(1):107–10.
5. Arzimanoglou AA, Salefranque F, Goutieres F, Aicardi J. Hemifacial spasm or subcortical epilepsy? Epileptic Disord. 1999;1(2):121–5.
6. Chae JH, Kim SK, Wang KC, Kim KJ, Hwang YS, Cho BK. Hemifacial seizure of cerebellar ganglioglioma origin: seizure control by tumor resection. Epilepsia. 2001;42(9):1204–7.
7. Bancaud J, Bonis A, Trottier S, Talairach J, Dulac O. [Continuous partial epilepsy: syndrome and disease].Rev Neurol (Paris). 1982;138(11):803-14.
8. Juul-Jensen P, Denny-Brown D. Epilepsiapartialis continua. Arch Neurol. Dec 1966;15(6):563-78.
9. Yaltho TC, Jankovic J. The many faces of hemifacial spasm: differential diagnosis of unilateral facial spasms. MovDisord. 2011 Aug 1;26(9):1582-92
10. Espay AJ, Schmithorst VJ, Szaflarski JP. Chronic isolated hemifacial spasm as a manifestation of epilepsiapartialiscontinua.EpilepsyBehav. 2008 Feb;12(2):332-6
11. Singh S. Botulinum toxin in hemifacial spasm: Revisited.Indian J Plast Surg. 2013 Jan;46(1):159-60
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License