IJCRR - 9(3), February, 2017
Pages: 08-13
Date of Publication: 10-Feb-2017
Print Article
Download XML Download PDF
Achievements and Implications of Positive Health Dignity and Prevention Model among People Living with HIV: A Systematic Evaluation of HAF II Project in Plateau State, Nigeria
Author: Ademola L. Adelekan1, 9*, Garos M. Bature2, Hadiza Maina3, Tagurum Yetunde4, Nanmak Bali5, Ezekiel Jamaka6, Sunday M. Koka2, Beben W. Wukatda2, Michael A. Owojuyigbe7, Olusegun Adeoye8, Michael Olugbil
Category: Healthcare
Abstract:Background: Nigeria accounts for almost half of all new HIV infections in sub-Saharan Africa every year. The positive health dignity and prevention (PHDP) intervention was designed by Plateau State Agency for the control of AIDS by engaging civil society organizations (CSOs) to reduced incidence of new infections, improved community-based care and support for people living with HIV (PLHIV) and reduce discrimination and stigmatization against PLHIV in plateau state, Nigeria. This article therefore presents the results of the intervention including the achievements and implications for programming.
Methods: This was an intervention project carried out in 3 out of 17 LGAs in plateau state with an estimated sample size of 17,177. The intervention was carried out by four CSOs who were engaged and provided with financial support under the HIV/AIDS Fund (HAF) II project. The CSOs worked among the PLHIV in the state using the PHDP model which is the minimum package for PLHIV interventions under the continuum of care. Data were collected using various data collection and reporting tools and entered into DHIS2 platform. Data were subsequently exported into Microsoft excel where it was analyzed and results presented in charts and tables.
Results: The overall target population reached during this intervention was 38211 PLHIV given a target reached of 222.5%. Among these, 74 persons died while 21 persons voluntarily withdrawn from this project. A total of 87 community dialogues were held and 912 influencers participated. A total of 12 income generating activities were also held and 89 persons benefitted. A total of 29312 (76.7%) persons were reached with at least one care representing a 76.7%. Out of the total of 51143 condoms required for this intervention, only 51.1% condoms were distributed while 1271 pregnant women were referred for antenatal care services.
Conclusion: This intervention had beneficial effects on people living with HIV and their families. Social and economic support for people living with HIV within the context of positive health, dignity and prevention is perhaps the most difficult to address, as it depends in large measure on the broader national economic, social and social protection systems, which are underfinanced in this intervention.
Keywords: HAF II project, Positive health dignity and prevention, People living with HIV
Full Text:
INTRODUCTION
In 2010, it was estimated that worldwide, over 34 million people were HIV-positive and approximately 68% of them lived in sub-Saharan Africa [1]. In this geographical region of the world, the typical pattern of healthcare is a combination of overburdened healthcare services with insufficient financial resources, inadequate infrastructure, few hospital beds and fewer health workers to cope with the health burdens faced [2-3]. The HIV pandemic, which is greatest in sub-Saharan Africa, contributes immensely to the health burden, and this further overstretches the already overburdened health systems [2;4]. Nigeria has the second largest HIV epidemic in the world [1]. Although HIV prevalence among adults is remarkably small (3.1%) compared to other sub-Saharan African countries such as South Africa (19.2%) and Zambia (12.9%), the size of Nigeria's population means 3.5 million people were living with HIV in 2015 [5]. An estimated 60% of new HIV infections in western and central Africa in 2015 occurred in Nigeria [5], together with South Africa and Uganda, the country accounts for almost half of all new HIV infections in sub-Saharan Africa every year [6]. This is despite achieving a 35% reduction in new infections between 2005 and 2013 [6]. Unprotected heterosexual sex accounts for 80% of new HIV infections in Nigeria, with the majority of remaining HIV infections occurring in key affected populations such as sex workers [7].
HIV prevalence is highest in Nigeria’s southern states (known as the South South Zone), and stands at 5.5%. It is lowest in the southeast (the South East Zone) where there is a prevalence of 1.8%. There are higher rates of HIV in rural areas (4%) than in urban ones (3%) [7]. Approximately 180,000 people died from AIDS-related illnesses in Nigeria in 2015 [8]. Since 2005, the reduction in the number of annual AIDS-related deaths has been minimal, indicative of the fact that only half (51%) of those living with HIV in Nigeria are accessing antiretroviral treatment (ART) [9]. Positive health dignity and prevention (PHDP) intervention designed by Plateau State Agency for the control of AIDS (PLACA) by engaging civil society organizations to reduced incidence of new infections, improved community-based care and support for people living with HIV (PLHIV) and reduce discrimination and stigmatization against PLHIV in plateau state, Nigeria. This article therefore presents the results of the intervention including the achievements and implications for programming.
MATERIALS AND METHODS
Study Design and Scope
This was an intervention project carried out among PLHIV in Plateau State, Nigeria. The HIV Programme Development Project (HPDP) aimed to improve the evidence-based targeting of activities within the State, by focusing on factors that drive the spread of the epidemic, thus attempting to reduce the incidence of new infections, while ensuring adequate care and support is provided for PLHIV.
Study Area
Plateau State is one of the states in the North-Central geo-political Zone. The state covers an area of about 26,899 square kilometers bounded in the North East by Bauchi State, North West by Kaduna State, South East by Taraba State and to the South and South West by Nasarawa State. Plateau state has a total population of 3,206, 531 people. The population of state from 2006 census was 1,598,998 males and 1,607,533 females with an annual growth rate of about 2.7%. The State has three senatorial zones and 17 Local Government Areas with a land area of 30,913km [10].
Study Population
The study population consisted of PLHIV who are randomly selected from three out of seventeen LGAs namely Jos North, Shendam and Pankshin LGAs.
Sample Size
The estimated sample size for this intervention was 17,177 PLHIV
Description of Intervention
This intervention was carried out by four Civil Society Organizations (CSOs) who were engaged and provided with financial support under the HIV/AIDS Fund (HAF) II component of HPDP II project. The CSOs engaged are Halt AIDS, Relief and Hope Foundation (RAHF), Christian Health Association of Nigeria (CHAN) and Manna Resource Development Center. The CSOs worked among the PLHIV in the state using Positive health dignity and prevention (PHDP) model which is the minimum package for PLHIV interventions under the continuum of care were used for this intervention. Programmatic components of Positive Health, Dignity and Prevention fall under the following eight (8) thematic areas namely Empowerment of people living with HIV and networks of PLHIV, Health promotion and access and Gender equality. Others are Human rights, Prevention of new infections, sexual and reproductive health and rights, social and economic support including measuring impact. Positive Health, Dignity and Prevention model is not just a new name for the concept of HIV prevention for and by people living with HIV, formerly known as ‘positive prevention’. Rather, PHDP is built upon a broader foundation that includes improving and maintaining the dignity of the individual living with HIV; supports and enhances the individual’s physical, mental, emotional and sexual health; and, which, in turn, among other benefits, creates an enabling environment that will reduce the likelihood of new HIV infections [11]. Positive Health, Dignity and Prevention encompasses the full range of health and social justice issues for people living with HIV, and espouses the fundamental principles that responsibility for HIV prevention should be shared and that policies and programmes for people living with HIV should be designed and implemented with the meaningful involvement of people living with HIV [11]. By linking the social, health, and prevention needs of the person living with HIV within a human rights framework, PHDP results in a more efficient use of resources, with outcomes that are more responsive to the needs of people living with HIV and more beneficial for their partners, families, and communities [11]. The specific activities carried out under this intervention are described below.
Income Generation Activities
Income Generation Activities (IGAs) were provided through vocational empowerment for PLHIV to ensure that PLHIVs learned how to work independently, as well as earn income on their own.
Advocacy and Community Dialogue
Advocacy visits were made, and community dialogues were held with leaders of PLHIV groups and other stakeholders at the community level particularly among gate-keepers and people affected by AIDS. This was done to educate community members on stigmatization and discrimination against PLHIV within the communities.
Peer Education Session
A total of 538 peer educators were selected and trained to provide peer education sessions to their peers on partner reduction, correct and consistent use of condom, good health seeking behaviour, basic infection control practices at home, management of general ailments and identification of signs and symptoms of health issues requiring immediate medical care. They were also provided with sessions on Positive Health Dignity and Prevention (PHDP) in Nigeria, HIV prevention at the community setting, basic facts about HIV/AIDS, HIV related stigma and discrimination, management of sexually transmitted infections (STIs) including where and how to access antiretroviral therapy. Each training session was attended by a minimum of 15 and maximum of 30 participants and each participant were mandated to step down the knowledge to not less than 10 colleagues which are mostly PLHIV and/or their relatives.
Counseling Support
Counselling support was provided by trained volunteers on a wide-range of issues (disclosure of HIV status, treatment education and adherence support, psycho-social support, nutrition, positive living and positive prevention, sexual and reproductive health issues such as pregnancy and family planning, home based care) through one-to-one counselling or couple/family counselling. Children and adolescents living with HIV were also provided with counselling services on HIV status disclosure, ART adherence, personal hygiene, eating healthy and hygienic food, coping with emotions etc.
PLHIV Support Group
Support group was formed for PLHIV with the aimed of providing a platform for them to share their concerns and learn from each other. Regular support group meetings were organized by trained volunteers and information on various themes are provided to build capacity of PLHIV to live quality life. Monitoring and evaluation officers of the implementing CSOs monitored support group meeting by attending the meeting to encourage regular meeting attendance of support group members, share experience and encourage proper adherence alongside the normal health talk during support group meeting.
Condom Promotion
Several condom messaging, sensitization and demonstrations was carried out at individual volunteer cohort level and special sessions at least twice in a month. Project monitoring team re-enforcing the activities of volunteers by organizing special sessions with cohort group members to carry out comprehensive condom promotion
Data Collection
Data were collected during peer-to-peer sessions by the peer educators. Also collected were the number of PLHIV who received support services, and those who completed referrals.
Data Analysis
Data were collected using various but uniform data collection and reporting tools. The data were collected from various activities carried out under enrollment pattern, structural and socio-economic intervention and positive health dignity and prevention. The data were entered into DHIS2 platform and exported into Microsoft excel. The results were analyzed using Microsoft Excel by comparing frequencies and percentages while carefully presented in tables.
Ethical Consideration
Prior to the commencement of the intervention, the proposal was subjected to a two-stage review and ethical approval to conduct the research was obtained from the National and the State Ethical Review Committee and Federal Ministry of Health, Nigeria. Also, permission was obtained from the leaders of the identified groups where necessary.
RESULTS
The findings are presented based on the levels of intervention: Enrollment pattern, Structural and socio-economic intervention and positive health dignity and prevention. The overall target population reached during this intervention was 38211 given a target reached of 222.5%.
Enrollment pattern of participants
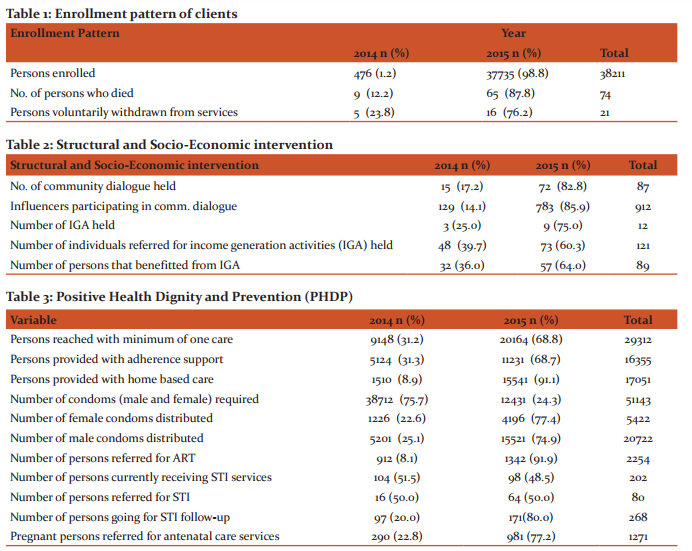
Out of the 38211 persons enrolled, 98.8% were enrolled in 2015. A total of 74 persons died and among these, 87.8% died in 2015. A total of 21 persons voluntarily withdrawn from this intervention without reason (Table 1)
Structural and Socio-economic Intervention
Out of the total of 87 community dialogues held, 82.8% were held in 2015 and a total of 912 influencers participated. A total of 12 income generating activities were held and the number of persons referred totaled 121 while only 89 persons benefitted (Table 2).
Positive Health Dignity and Prevention (PHDP)
Out of the 38211 reached with this intervention, a total of 29312 persons were reached with at least minimum of one care representing a 76.7%. A total of 16355 persons were support service and among these, 68.7% were reached in 2015. Out of the total of 51143 condoms required for this intervention, only 51.1% condoms were distributed. Among these, 20.7% and 79.3% were female and males condoms respectively. A total of 202 persons reported that they were currently receiving STI services and 80 persons were referred for STI. A total of 1271 pregnant women were referred for antenatal care services (Table 3).
DISCUSSION
This project was carried out among PLHIV in a bid to know the number of persons infected by the epidemic, as well as to ensure that they are catered for by the communities they belong to. This was brought to bear in the community dialogues, and advocacy meetings held with community members, and leaders, as well as with the leaders and members of existing PLHIV groups. Furthermore, support groups were worked with to enlighten them on the necessary issues of PLHIV care and support. Additionally, several care options were made available to those infected and who had enrolled, with clients being helped towards completion of referrals. Also, vocational empowerment was provided to ensure that PLHIV can cater for themselves financially when necessary. Many of the participants were provided with home based care. The World Health Organisation, the government of several countries as well as care givers of PLWHA have acknowledged home based care as a necessary component of HIV care and support [12-14]. Home based care programmes have been developed with a view to assisting families and care givers in providing HIV-related care to patients, and this has aided in reducing the burden on hospitals caring for PLWHA [15]. It has been estimated that up to 90% of illness care may be provided in the home by untrained family and associates [16]. In resource constrained settings burdened by HIV/AIDS such as found in sub-Saharan Africa, home based care plays a valuable and strategic role in complementing existing health care services by extending the continuum of care for PLWHA and their families into the home, thus bridging the gap between facility and home care [14;16;17]. However, in some instances, HBC is the only option available for many HIV/AIDS patients who do not have access to healthcare facilities for various reasons and it replaces hospital care [17]. Furthermore, such care is usually carried out by persons who have no training or contact with professional help. An effective HBC programme for PLWHA can yield major health and social benefits not only to the patients, but also to their families and therefore the community [18].
One of the most important phases of this intervention was the provision of PLHIV with adherence support. This was because PLHIV need to consider themselves as part of the solution rather than a part of the problem. Strict adherence to antiretroviral therapy (ART) is key to sustained HIV suppression, reduced risk of drug resistance, improved overall health, quality of life, and survival [19-20], as well as decreased risk of HIV transmission [21]. Conversely, poor adherence is the major cause of therapeutic failure. Achieving adherence to ART is a critical determinant of long-term outcome in HIV infected patients. It is unfortunate to note in this intervention that only a little more than half of the condoms required for this intervention were distributed when condoms are a critical component in a comprehensive and sustainable approach to the prevention of HIV and other sexually transmitted infections (STIs) [22]. Laboratory studies show that condoms provide an impermeable barrier to particles the size of sperm and STI pathogens, including HIV [23-24]. Condoms, when used consistently and correctly, are highly effective in preventing the sexual transmission of HIV. Research among sero-discordant couples (where one partner is living with HIV and the other is not) shows that consistent condom use significantly reduces the risk of HIV transmission both from men to women and women to men [25-27]. Consistent and correct use of condoms also reduces the risk of acquiring other STIs and associated conditions, including genital warts and cervical cancer. With a failure rate of about 2% when used consistently and correctly, condoms are very effective at preventing unintended pregnancy [28-29].
Implications for Programming
Preventing new HIV infections is the shared responsibility of everyone irrespective of HIV status. As such, this intervention includes people living with HIV in all aspects of project activities. It rejects the notion that people living with HIV are solely responsible for the health of those with whom they interact. It also acknowledges and addresses HIV-related stigma and other social determinants of health that influence the vulnerability of those affected. Furthermore, this intervention promotes programmes that help empower participants to take responsibility for their own health and well being. By doing so, this will have a positive impact on partners, families and communities. Sustainable finance and support is essential in order to ensure that the impacts of this intervention are not lost. In addition, it is further important for future interventions in like-mold to ensure that facilities, and care services are available to cater for more participants than previously estimated. This would help reduce incidences of disenfranchisement with such programmes, as well as ensure that all enrolled clients are adequately catered to, and the spread of HIV through PLHIV or the occurrence of deaths of PLHIV is well dealt with. It is important to further point out that more PLHIV than the estimated target population trooped out to avail themselves of the various services on offer during the intervention. This can be observed in the number of enrollees during the programme duration which as noted exceeded the target population, adding up to slightly more than two times the estimated expected target, leading to a situation of low coverage of clients who turned out for the intervention programme, with a variety of services. In other circumstances, this occurrence might have led to a chaotic situation wherein clients would return to their abodes hugely dissatisfied with the intervention programme, and this would in turn have spiral consequences on the health of many-a-client and the spread of HIV among the population.
CONCLUSION
This intervention had beneficial effects on people living with HIV, their partners, families, and communities, including reducing the likelihood of new infections. Social and economic support for people living with HIV within the context of positive health, dignity and prevention is perhaps the most difficult to address, as it depends in large measure on the broader national economic, social and social protection systems, which are underfinanced in this intervention. Employment and economic empowerment for people living with HIV- in particular, women and young people living with HIV requires ensuring that PLHIV have equitable access to education and employment.
Acknowledgment
The evaluation team wishes to acknowledge the World Bank and the National Agency for the Control of AIDS (NACA) for making available the funding for the evaluation and dissemination of this project intervention. Special appreciation goes Mrs. Philomena Daduut, Mrs. Aishetu J. Garang, Seign. Ango G. Abdullahi, Mr. Albert Fube Bewaran, Mr. Melchizedek Toma, Apollos Enoch and Dachollom Pam for their support and cooperation during this project implementation. Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/ publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of interest: None
References:
- United Nations Programme on HIV/AIDS (UNAIDS) (2010). Global report: UNAIDS report on the global AIDS epidemic 2010. Geneva: UNAIDS
- World Health Organization (WHO) (2008). Primary health care: now more than ever. Geneva, WHO. Available at: http://www.who.int/whr/2008/whr08_en.pdf
- Tillekeratne LG, Thielman NM, Kiwera RA, Chu HY, Kaale L, Morpeth SC, Ostermann J, Mtweve SP, Shao JF, Bartlett JA, Crump JA (2009). Morbidity and mortality among a cohort of HIV-infected adults in a programme for community home-based care, in the Kilimanjaro Region of Tanzania (2003–2005). Ann. Trop. Med. Parasitol. 103(3):263-273.
- United Nations Programme on HIV/AIDS UNAIDS (2014). HIV and AIDS in sub-saharan Africa regional overview. UNAIDS GAP Report 2014
- United Nations Programme on HIV/AIDS (UNAIDS). 2016 Prevention Gap Report
- United Nations Programme on HIV/AIDS (UNAIDS). The Gap Report. 2014
- National Agency for the Control of AIDS (NACA). Global AIDS Report Progress Report for Nigeria. 2015
- United Nations Programme on HIV/AIDS (UNAIDS). 2015 HIV and AIDS Estimates
- National Agency for the Control of AIDS (NACA). End of Term Desk Review Report of the 2010-2015 National HIV/AIDS Strategic Plan. 2015
- Plateau AIDS Control Agency (PLACA). 2015. HIV/AIDS Fund (HAF) Closing Report
- UNAIDS, GNP+. 2013. Positive Health, Dignity and Prevention: Operational Guidelines. Geneva and Amsterdam
- World Health Organisation (WHO)/ United Nations Programme on HIV/AIDS (UNAIDS) (2000). Key elements in HIV/AIDs care and support: Draft Working Document. UNAIDS.
- Pindani M, Maluwa A, Nkondo M, Nyasulu BM, Chilemba W (2013). Perception of People Living with HIV and AIDS Regarding Home Based Care in Malawi. J. AIDS Clin. Res. 4:201.
- Ibrahim K, Haroen H, Pinxten L (2011). Home-based Care: A need assessment of people living with HIV infection in Bandung, Indonesia. J. Assoc. Nurses AIDS Care 22(3):229-37.
- Makoae MG, Jubber K (2008). Confidentiality or continuity? Family caregivers’ experiences with care for HIV/AIDS patients in homebased care in Lesotho. SAHARA J. 5:36-46.
- Ogden J, Esim S, Grown C (2006). Expanding the care continuum: Bringing cares into focus. Health Policy Plann. 21(5):333-342.
- Aantjes C, Quinlan T, Bunders J (2014). Integration of community home based care programmes within national primary health care revitalisation strategies in Ethiopia, Malawi, South-Africa and Zambia: a comparative assessment. Glob. Health 10:85.
- Mupfurima IM (2013). Home based care for HIV and AIDS patients: A case of Rujeko C suburbs Masvingo urban Zimbabwe. Int. J. Acad. Res. Prog. Educ. Dev 2(2):99-112.
- Chesney MA. The elusive gold standard. Future perspectives for HIV adherence assessment and intervention. J Acquir Immune Defic Syndr. 2006;43 Suppl 1:S149-155. Available at http://www.ncbi.nlm.nih.gov/pubmed/17133199.
- World Heath Organization (WHO). Adherence to long term therapies—evidence for action. 2003. Available at http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf.
- McPherson-Baker S, Malow RM, Penedo F, Jones DL, Schneiderman N, Klimas NG. Enhancing adherence to combination antiretroviral therapy in non-adherent HIV-positive men. AIDS Care. 2000;12(4):399-404. Available at http://www.ncbi.nlm.nih.gov/pubmed/11091772.
- UNFPA, WHO and UNAIDS: Position statement on condoms and the prevention of HIV, other sexually transmitted infections and unintended pregnancy. July 2015
- Carey RF et al. Effectiveness of latex condoms as a barrier to human immunodeficiency virus-sized particles under conditions of simulated use. Sex Transm Dis 1992;19:230-4.
- WHO/UNAIDS. 2001. Information note on Effectiveness of Condoms in Preventing Sexually Transmitted Infections including HIV.
- Holmes K et al. Effectiveness of condoms in preventing sexually transmitted infections. Bulletin of the World Health Organization, 2004, 82 (6).
- Weller S et al. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev. 2002;(1):CD003255.
- Smith DK et al. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2015 Mar 1;68(3):337-44.
- Trussell J. Contraceptive efficacy, in: Hatcher RA et al., eds., Contraceptive Technology: Twentieth Revised Edition, New York: Ardent Media, 2011, pp. 779–863.
- Kost K et al. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception, 2008; 77:10-21.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License