IJCRR - 9(3), February, 2017
Pages: 01-07
Date of Publication: 10-Feb-2017
Print Article
Download XML Download PDF
Achievements and Implications of HIV Prevention Programme among General Population: A Systematic Evaluation of HAF II Project in Plateau State, Nigeria
Author: Ademola L. Adelekan1, 9*, Garos M. Bature2, Joyce Dakun3, Harrison Christian4, Nanmak Bali5, Hosea Onuche6, Rhoda Udanyi7, Temilade Adegoke8, Oladipupo S. Olaleye1, 9, Sunday M. Koka2, Beben W. Wukatda2
Category: Healthcare
Abstract:Background: Nigeria has the second largest HIV burden in the world and Plateau State is one of the states with highest prevalence in Nigeria. It is therefore necessary to ameliorate this problem. This paper therefore presents achievements and implications of HIV prevention programme among general population in Plateau State, Nigeria.
Method: This intervention project was carried out among male and female between the ages of 15-49 years. A total of five civil society organizations were engaged by Plateau State Agency for the Control of AIDS and trained to provide HIV prevention programmes under the HIV/AIDS Fund (HAF) II project. A total of 54,401 individuals were the estimated sample size for this intervention and the minimum prevention package intervention was adopted in the implementation of this project activities. Data collected were analyzed using Microsoft Excel and presented using descriptive statistics such as percentage, simple proportion and frequency.
Result: A total of 115 community dialogues/advocacies were carried out during this intervention and 5,528 male and 4,813 female influencers participated. A total of 52,417 male and 7,081 female condoms were distributed. A total number of 32,396 males and 28,121 females were counseled, tested and received result. Among these, 147 males and 180 females tested positive. A total number of 1,959 males and 111 females were referred for STI with almost all the referrals (99.4% male and 91.0% female) taking place in 2015. During this project, 16 pregnant women were also referred for antenatal care.
Conclusion: This intervention successfully scaled-up demand creation for condoms use and HIV counseling and testing through a mix of structural, behavioral and biomedical interventions. More engagement at all levels to ensure community ownership of the HIV response with a view to ensuring sustainability through increased funding should therefore be encouraged.
Keywords: HAF II project, General population, Minimum prevention package intervention, HIV/AIDS
Full Text:
INTRODUCTION
High incidence of HIV and AIDS has a disproportionately greater impact on sub-Saharan Africa, which constitutes about 10 percent of the world’s population but has the highest number of HIV infections. Twenty five million of the global estimates of about 40 million infected people live in this region of the World [1]. Out of the current estimated population of about 182.2 million people in Nigeria, between 3.2 and 3.8 million are reported to be infected and this figure is projected to increase to between 3.7 and 4.3 million by the year 2020. Nigeria has the second largest HIV epidemic in the world [2]. Although HIV prevalence among adults is remarkably small (3.1%) compared to other sub-Saharan African countries such as South Africa (19.2%) and Zambia (12.9%), the size of Nigeria's population means 3.5 million people were living with HIV in 2015 [3]. An estimated 60% of new HIV infections in western and central Africa in 2015 occurred in Nigeria together with South Africa and Uganda, the country accounts for almost half of all new HIV infections in sub-Saharan Africa every year [3]. This is despite achieving a 35% reduction in new infections between 2005 and 2013 [4]. Unprotected heterosexual sex accounts for 80% of new HIV infections in Nigeria, with the majority of remaining HIV infections occurring in key affected populations such as sex workers [2]. HIV prevalence is highest in Nigeria’s southern states (known as the South South Zone), and stands at 5.5%. It is lowest in the southeast (the South East Zone) where there is a prevalence of 1.8%. There are higher rates of HIV in rural areas (4%) than in urban ones (3%) [2]. Approximately 180,000 people died from AIDS-related illnesses in Nigeria in 2015 [5]. Since 2005, the reduction in the number of annual AIDS-related deaths has been minimal, indicative of the fact that only half (51%) of those living with HIV in Nigeria are accessing antiretroviral treatment (ART) [6].
Plateau state has been classified among states in the “hot zone” of HIV infections. The state is one of the 12 + 1 states contributing the highest HIV prevalence in Nigeria. The state had a prevalence of 7.7% in 2010 placing her in the 6th position in the country and the 2nd position among the states in the North Central zone [7]. The prevalence is higher in the urban areas than in the rural areas (10.5% as compared with 2%). HIV prevention efforts to date have overwhelmingly focused on reducing individual risk, with fewer efforts made to address structural factors, social norm and cultural believes that increase vulnerability to HIV. The approach known as “combination prevention offers the best prospects for addressing documented weaknesses in HIV prevention programming and for generating significant, sustained reductions in HIV incidence in diverse settings as it relies on the evidence informed, strategic, simultaneous use of complementary behavioral, biomedical and structural prevention strategies. This paper therefore presents achievements and implications of HIV prevention programme among general population in Plateau State, Nigeria
MATERIALS AND METHODS
Study Design
This intervention project was carried out among general population in Plateau State, Nigeria between the year 2013 and 2016. A total of five civil society organizations (CSOs) were engaged by Plateau State Agency for the Control of AIDS and trained to provide HIV prevention programmes under the HIV/AIDS Fund (HAF) II project. The CSOs engaged for this intervention are Fahariya Adolescent Development Network (FAANET), Adolescent Health Empowerment and Development Initiative Nigeria (AHEAD-NG), Relief and Hope foundation, Youth’s Information and Leadership Training Centre and Scripture Union West Africa (SUWA).
Study Area
This study was carried out in two randomly selected local government areas (LGAs) in Plateau States namely Shendam and Jos-North LGAs. The LGAs with the highest prevalence were Jos North (16.7%) and Shendam (4.6%) according to the 2010 National sero-prevalence study [7]. Plateau State is one of the 36 states of Nigeria located within the north central geopolitical Zone. The 2006 National Population Census put the population of Plateau State at 3,178,712 (1,593,033 males and 1,585,679 females) [8]. Shendam is an LGA with its headquarters in the town of Shendam at 8°53′00″ N 9°32′00″ E. It has an area of 2,477 km² and a population of 208,017. Jos-North on the other hand is an LGA with its headquarters in the city center of Jos. It has an area of 291 km² and a population of 429,300 [8].
Study Population
The project was carried out among male and female between the ages of 15-49 years in two local government areas
Sample size
A total of 54,401 (male and female) were the estimated sample size for this intervention
Intervention
The minimum prevention package intervention (MPPI) was adopted in the implementation of this project. Project interventions are categorized under the three components of MPPI which are structural, behavioural and biomedical interventions. Activities carried out under each of the component are summarized below situs slot ;
Structural Intervention
This area of intervention involves mobilizing community and individuals to address structural barriers such as cultural believes and practices that hinder peoples access and utilization of appropriate HIV prevention, treatment and care services. The implementing organizations organized series of community dialogues, outreaches, sensitization and awareness creation across all the project communities with the aim of sensitizing community stakeholders on the HIV/AIDS situation around them and to recruit community volunteers to be trained as peer educators. The session attracted a number of influencers who also participated in various awareness programs. They were introduced to the basics of HIV and AIDS which includes the mode of transmission and prevention as well as the cycle of HIV (how untreated HIV becomes AIDS). The aim was to bring community stake holders together, properly intimate them about the project to be implemented, discuss possible success routes for the project, and start making efforts towards community ownership of the project.
Behavioral intervention
This aspect involves change in behavior aimed at influencing beneficiaries to adopt healthy behaviors so as to reduce their risk for HIV infection. Such behaviors include partner reduction, correct and consistent use of condom, good health seeking behavior for prompt treatment of STIs, treatment referral, follow-up and HCT. Behaviors of the general population in the course of this project were targeted to be modified through the use of Peer Education (PEs) and Condom distribution.
Identification, Selection and Capacity Building for Peer Educators (PE)
The implementing organizations identified and trained voluntary peer educators (1200 males and 1550 females) among the general population who also reached a number of their peers on HIV and AIDS related issues. Three days training was designed purposely to build the capacity of PEs and improve their proficiency in carrying out effective HIV prevention intervention activities among their peers in their various communities. Using Peer Education manuals, the participants were taken through series of topics on HIV/AIDS issues and peer education strategies for balance ABC prevention intervention. Each modules and topics were presented using discussion, group works, role plays and various exercises and energizers. Also, pre and post-test evaluation of participants at the point of entry and at the end of training was conducted to measure the impact of the training on the trained peer educators. Topic covered during the training as designed in the seven (7) modules PEs guides include the following and many other: life skills, general knowledge of HIV/AIDs, sexually transmitted infections and types, HIV prevention and access to help, gender and sexuality, peer education characteristics and qualities, gender and HIV/AIDs. The peer educators were involved in contact making referrals, distribution of IEC materials, demonstration and distribution of condoms, running education and training sessions, mobilizing community members and advocacy. The peer educators ensured 2 to 3 regular contacts with their peers in 10 to 15 day interval within a period of 2 or 3 months.
Selection Criteria for PEs
The PEs were selected from community based organizations (barbers, fashion designers, patent medicine vendor and hair dressing associations), religion organization (Christian Association of Nigeria and Muslim Associations). Those who were recruited as PEs met certain criteria such as: been resident within the project community, been able to read and write and availability within the project community for a period of 18 months.
Condom Distribution
Condom messages were given on the importance and need for consistent and correct condom use. Proper and correct use of condom was demonstrated and a number of both male and female condoms were distributed within the project communities. Some PEs also did condom forecasting for their peers and distributed the commodity which was made available by the project management team. All these were to facilitate a change in attitude and behavior among the general population within the project communities.
Biomedical Intervention
HIV Counseling and Testing (HCT)
HCT was conducted by trained counselor tester using the client intake form for data documentation. The HCT has three distinct components: risk assessment and counseling before the blood or oral sample is taken, testing of the sample, and counseling and referral with the test results. These three components were properly followed in this project. The implementing organizations trained ad-hoc counselor tester and peer educator volunteers who conducted mobile HIV counseling and testing among the general population. In addition, some project management staff also organized community HCT outreaches. During this period, awareness was also created on the use of condom and condoms were also distributed.
Referral
Client needs for care and supportive services are assessed and prioritized while the clients are provided with assistance such as setting up appointments, providing transportation among others in accessing treatment and care services. Follow-up were also provided to participants to facilitate initial contact with care and support service providers. During the period of this project through the Ad-hoc testers and trained volunteers, several referrals were made for care and treatment in various health care facilities. Clients diagnosed for STIs and HIV were tracked and escorted to the health facilities for care/treatment.
Start-Up Training
Preceding the commencement of the intervention phase was a start-up training and capacity building for project staff and project management team and reviews of such meetings continued as the project progressed. Start-up training was held by the Plateau state agency for the control of AIDS together with key members of implementing organizations management team, staff and board members where they were well informed of the project and its processes. The aim of the training was to strengthen their capacity for better understanding of MPPI for optimum project implementation. They were trained on thematic areas including but not limited to implementation of HPDP in Nigeria, drivers of HIV/AIDS epidemic in Nigeria, care and services for people living with HIV (PLHIV), implementation plan for CSOs on the HAF II project, importance of community dialogues and advocacy visits, monitoring and evaluation system for prevention.
Monitoring and Evaluation (MandE) Visit
Several MandE visits and activities were carried out by the implementing situs judi slot online deposit pulsa tanpa potongan and other project team actors to ensure that activities were implemented as planned and that the data recorded and reported were accurate and valid. It was also to incorporate a system of analysis, supervision and review which led to remedial actions to improve performance. For the monitoring and supervision to yield reasonable success in the project locations, key questions were incorporated in a short precise MandE tool to attain useful and specific data during supervision and monitoring visits to the implementation sites. The responses retrieved provided an overview of the impact of interventions; highlighting areas of success and the major areas that required improvement.
Data Management and Analysis
Capacity Building on Data Entry
In order to ensure quality data, key project staff attended the DHIS training conducted by PLACA for uniform state platform collation of data. During the 5 days training, CSOs were coached on how to enter the collected data on the platform.
Data Quality Assurance (DQA)
DQA was carried out and this provided a platform for evaluating the performance and impact of the project implemented. During project management meeting, it was discussed how to carry out the DQA, which sites to visit, which PE conductor should be involved, logistics, location/sites, thematic areas and number of days to carry out the activity. Profiling the data to discover inconsistencies and other anomalies in the data, as well as performing data cleansing activities (e.g. removing outliers, missing data interpolation) to improve the data quality was also done.
Data Analysis
Data were entered on DHIS2 platform and later exported and analyzed using Microsoft Excel. Data were presented using descriptive statistics such as percentage, simple proportion and frequency.
Ethical consideration
It was ensured that there was confidentiality during HIV counseling and testing and permission was adequately sought from various community leaders before approaching the community members. Client intake forms used during the HCT were also kept where unauthorized person could not gain access to it.
RESULT
Structural Intervention
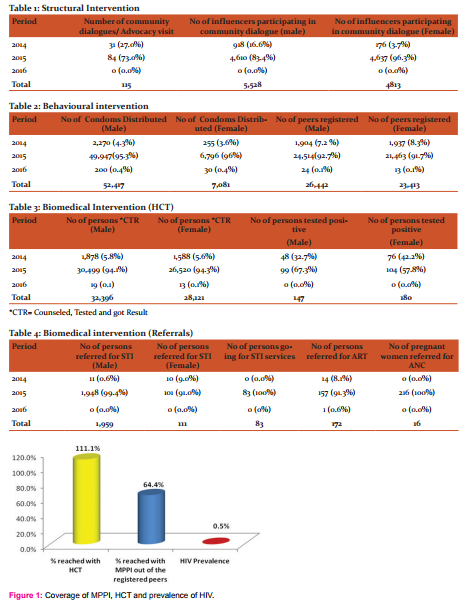
Table 1 presents the result of the structural intervention. Out of the total number of 115 community dialogues/advocacies carried out during the project period, 27.0% were carried out in 2014, 73.0% in 2015 while none took place in 2016. A total number of 5,528 male and 4,813 female influencers participated in the community dialogue with 16.6% of male and 3.7% of female participants in 2014, 83.4% of male and 96.3% of female participants in 2015.
Behavioural Intervention
The result of behavioral intervention is presented in table 2. A total number of 52,417 male condoms and 7,081 female condoms were distributed out of which 4.3% of male condom and 3.6% of female condom were distributed in 2014, 95.3% of male condoms and 99.4% of female condoms were distributed in 2015 and 0.4% of male and 0.4% of female condoms were distributed in 2016. A total number of 26,442 male peers and 23,413 female peers were registered during the project period. Out of this number, almost all peer registration was done in 2015 with 92.7% of male and 91.7% of female peers registered during this period while 7.2% of male and 8.3% of female peers was registered in 2014 and just 0.1% of both male and female peer registration was done in 2016.
Biomedical Intervention
The result of the biomedical aspect of the intervention which involves various activities such as HCT, referrals for sexually transmitted infections (STI), antiretroviral therapy (ART) and antenatal care (ANC) is presented in table 3 and 4. A total number of 32,396 males and 28,121 females were counseled, tested and received result (CTR). Among these, 147 males and 180 females tested positive (Table 3). A total number of 1,959 males and 111 females were referred for STI with almost all the referrals (99.4% male and 91.0% female) taking place in 2015 and 0.6% of male and 9% of female referrals for STI took place in 2014. Also, 83 people were going for STI services while 172 people were referred for ART out of which 8.1% were referred in 2014, 91.3% in 2015 and 0.6% in 2016. During this period, 216 pregnant women were also referred for ANC with all these referrals taking place in 2016 (Table 4).
Coverage of MPPI, HCT and Prevalence of HIV
A total of 32127 (64.4%) of the registered peers were reached with all the three stages of MPPI and 60517 (111.1%) were reached with only HCT. Among these, 327 (0.5%) were tested positive to HIV (Fig. 1).
DISCUSSION
The structural intervention of this program which included community dialogue/ mobilization was able to attract greater number of influencers in the year 2015 as compared to 2014. This difference could be as a result of the fact that almost thrice the number of community mobilization that took place in 2014 occurred in 2015. It was observed that no community dialogue took place in 2016 and this could be attributed to rounding off of the program while most activities have taken place during the previous years. Community dialogue in this project was very useful as it helped identify and enlist key individuals for sustainable partnership, helped solicit community participation, support and commitment to problem solving for sustainable behavioral change and promoted sharing of information and ideas between individuals of different cadres and backgrounds. Through facilitated sessions during the course of various community mobilizations, the program sparked critical thinking and open dialogue among participants which promoted mutual understanding of the epidemic and how to control it. In a similar attempt to evaluate the effectiveness of community dialogue in changing gender norms for HIV prevention in Tchova, Mozambique, Maria et, al [9] observed that community participation contributed significantly to observed changes in three of the underlying structural factors of HIV namely gender attitudes, gender roles, and HIV stigma. It was noted that the program also contributed to changing HIV prevention knowledge and behaviors that are associated with HIV infection, including discussion of HIV between sex partners.
The behavioral intervention of the program aimed at changing the behaviors of the general population incorporated both male and female condom distribution together with peer education. Most of the peer registration took place in 2015 and this probably explained why higher condom distribution occurred in 2015 as compared to 2014. Higher registration rate of peers and larger quantity of condom distribution that took place in 2015 can also be attributed to better access to resources both in financial and resource terms. It could also be that the system was more stabilized and organized subject to a wealth of experience gathered over the previous year. In all, more male condoms were distributed as compared to that of female condoms and this could be as a result of usual female attitude of evading stigma associated with collection of such commodity. However, adequate and effective awareness and education on condom use as a sustainable option for prevention of STIs prior to distribution could have removed such limiting barriers. Usage of condoms and especially if they are to be used consistently as a means of HIV prevention requires that people have access to them and are able to afford them. A reliable supply and distribution system of condoms during this project period provided accessibility and availability through mass distribution thus promoting uptake of the commodity. The use of peer educators in this project facilitated interactions between condom use and HIV prevention by communicating information on the effectiveness of condoms and by ensuring a sufficient and regular supply of condoms to those who require them. Condom promotion and distribution has been credited with large-scale successful programs in the developing world to control HIV and AIDS as noted in Thailand nationwide condom program aiming for 100% condom use in sexual encounters with sex workers. The program according to Levine [10] which provided condoms free of charge, provided education and promotion of condoms, and carefully monitored incidences of sexually transmitted infections to identify locations that were not in compliance with the initiative noted that sexually transmitted infections fell significantly and reported rapid rise in condom use. Most aspect of biomedical interventions such as number of people accessing counseling and testing and referrals for STI recorded the highest number in 2015 and this could be attributed to better resource mobilization and impact of activities of previous year. There was a good reflection of male to female ratio participation in counseling and testing and this reflects a good degree of women involvement in the project. However, more females tested positive as compared to males in this project. This reflects a higher prevalence of HIV infection among women than their male counterparts and this could be traced to the fact that women are at a greater biological risk of contracting HIV than men through various routes such as their greater mucosal surface area which is exposed to pathogens and infectious fluid for longer periods during sexual intercourse, low economic status which is associated with earlier sexual experience, lower condom use, multiple sex partners, and gender norms which promote multiple concurrent sexual partners for men among others. The 0.5% prevalence of HIV in this project marks a significant reduction when compared with 7.7% recorded for the state in 2010 [7]. This could have been as a result of various prevention activities that have been ongoing in the state to curb the epidemics. However, the impact of the combination prevention program undertaken in this project can only be felt by conducting a post prevention program analysis.
Implications for Programming
Effective and efficient prevention strategy that can lead to reduced incidence of HIV and AIDS must incorporate critical components of MPPI which include structural, behavioral and biomedical intervention as undergone in this project in selected local governments, however, extension of such intervention package to other local governments of the state cannot be overemphasized. Generally, the program was a success as HCT reached above its target. However, the percentage reached with MPPI was low compared to the target expected to be achieved in this programme despite the fact that a good number of the population were registered as peers for the behavioural intervention. This low achievement may be attributed to low turn-out of peers for the cohort session and not HCT or attrition of the peers, hence failure to meet up with the minimum of 6 contacts for cohort sessions before being said to be reached with MPPI. Future similar programmes among general population in the state should ensure more people are reached with behavioral intervention and MPPI by planning ahead to prevent such challenge even if it may involve the use of incentives. Considering that the program recorded great number of people reached with counseling and testing, it is evident that outreach workers and peer counselors/educators can be an important and effective resource to help clients identify needs and plan successful referrals. When peer education programmes are well designed and well implemented as a component of an overall HIV prevention strategy, they can contribute towards improving knowledge, attitudes and skills related to HIV. Successful peer education can motivate people to adopt and maintain safer sexual behaviour or minimize risk practices associated with sex and drug use. It can also reinforce behavior change, as the participant identified with a peer group where safer behaviour becomes the group norm. However, to enhance successful completion of referral and follow up, it is important to incorporate post-test support and services that advice those who test HIV-positive on the meaning of their diagnosis, and on referral to the treatment, care and support and prevention programmes and services available to assist them. This may go a long way in changing the attitude of people referred for STI to do proper follow up and complete their referrals.
CONCLUSION
This project successfully scaled-up demand creation for condoms and HIV counseling and testing among general population through a mix of structural, behavioral and biomedical interventions. The HIV minimum package prevention intervention provided suitable strategy for scaling up of the uptake of HCT, HIV peer education and condom promotion services. More engagement at all levels to engender political commitment and ownership of the HIV response (including State and LGA levels) with a view of ensuring sustainability through increased funding should also be encouraged.
Acknowledgment
The evaluation team wishes to acknowledge the World Bank and the National Agency for the Control of AIDS (NACA) for making available the funding for the evaluation and dissemination of this project intervention. Special appreciation goes Mrs. Philomena Daduut, Mrs. Aishetu J. Garang, Seign. Ango G. Abdullahi, Mr. Albert Fube Bewaran, Mr. Melchizedek Toma, Apollos Enoch and Dachollom Pam for their support and cooperation during this project implementation. Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
- Joint United Nations Programme on HIV/AIDS (UNAIDS) and World Health Organization (WHO). AIDS epidemic update (2007)
- National Agency for the Control of AIDS (NACA). Global AIDS Report Progress Report for Nigeria. 2015
- Joint United Nations Programme on HIV/AIDS (UNAIDS). 'Prevention Gap Report. 2016
- Joint United Nations Programme on HIV/AIDS (UNAIDS). 2014 The Gap Report
- Joint United Nations Programme on HIV/AIDS (UNAIDS). 2015 HIV and AIDS estimates
- National Agency for the Control of AIDS (NACA). ‘End of Term Desk Review Report of the 2010-2015 National HIV/AIDS Strategic Plan’
- Federal Ministry of Health (FMOH) Abuja: 2010. Technical report on National HIV Sero-prevalence sentinel Survey Among Pregnant Women Attending Antenatal Clinics in Nigeria.
- National Population Commission (NPC) [Nigeria] 2006 Population and Housing Census of the Federal Republic of Nigeria. Abuja, Nigeria: National Population Commission; 2006.
- Maria Elena Figueroa, Patricia Poppe, Maria Carrasco, Maria Dirce Pinho, Felisberto Massingue, Maria Tanque and Amata Kwizera. Effectiveness of Community Dialogue in Changing Gender and Sexual Norms for HIV Prevention: Evaluation of the Tchova Tchova Program in Mozambique, Journal of Health Communication, 2016. 21:5, 554-563, DOI: 10.1080/10810730.2015.1114050
- Levine, Ruth. 2007. Case 2: Preventing HIV and sexually transmitted infections in Thailand (PDF). In Case Studies in Global Health: Millions Saved. Sudbury, MA: Jones and Bartlett
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License