IJCRR - 6(9), May, 2014
Pages: 01-10
Print Article
Download XML Download PDF
COMMUNITY-ACQUIRED METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS
Author: Veni Emilda J. K., Shrikala Baliga, Shenoy M., Gopalkrishna Bhat K.
Category: General Sciences
Abstract:Methicillin resistant S.aureus (MRSA) has emerged as an important pathogen first in hospitals and then in the community. Community - acquired MRSA (CA-MRSA) has recently emerged as a significant pathogen, mainly causing skin and soft tissue infections in immunocompetent individuals residing in the community. It may also cause serious infections such as pneumonia. Person to person spread of CA-MRSAoccurs mainly due to overcrowding, skin to skin contact, compromised skin integrity, sharingcontaminated materials and poor hygiene. Possession of staphylococcal cassette chromosome mec type IV (SCCmec IV) encoding for mecA gene, susceptibility to non \?-lactam antibiotics and a pvl gene encoding Panton-Valentine Leukocidin (PVL) primarily distinguish CA-MRSA from healthcare-associated MRSA. In addition to PVL, CA-MRSA produces many other virulence factors which play important role in its pathogenicity.
Keywords: Community-acquired MRSA, Panton - Valentine Leukocidin, Staphylococcal cassette chromosome mec IV
Full Text:
NTRODUCTION
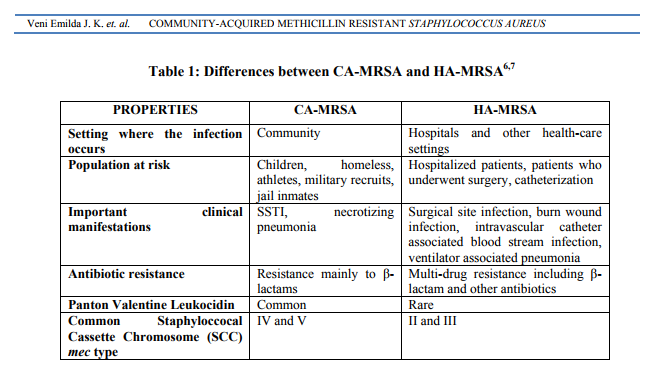
Staphylococcus aureus continues to be an important pathogen due to its versatility of diseases caused, virulence factors and drug resistance. Methicillin resistant S. aureus (MRSA) emerged in the 1960s, making S. aureus resistant to many antibiotics.1 MRSA is a significant pathogen causing both health care-associated (HAMRSA) and community-acquired (CA-MRSA) infections. HA-MRSA has been a serious problem in hospitals and health care facilities worldwide including India.1,2 In the 1990s, MRSA, which was once confined to hospital setting was seen to affect immunocompetent people with no health care risk factors such as athletes and other sportsmen.3CAMRSA then gained importance as a serious threat following the death of 4 children in North Dakota and Minnesota with severe CA-MRSA infection.4 In the recent years, there have been increasing reports of CA-MRSA from various parts of the world. Initially, it was believed that CA-MRSA emerged fromHA-MRSA since clonal relation was seen among them.5However, with epidemiological and molecular profiling, it was observed that CAMRSA are different from HA-MRSA in terms of risk factors associated, drug susceptibility pattern, virulence factors and molecular properties.1 Comparison of CA-MRSA and HA-MRSA is shown in Table 1.6,7
DEFINITION
According to CDC, CA-MRSA is defined based on the following criteria.8 ? Diagnosis of MRSA in the outpatient setting or by positive culture within 48 hours of hospital admission. ? No history of MRSA infection or colonization. ? No following history in the previous year 1. Hospitalization/Admission to a nursing home, skilled nursing facility or hospice 2. Dialysis 3. Surgery ? No permanent indwelling catheters or medical devices that pass through the skin into the body. CA-MRSA is usually susceptible to trimethoprim / sulfamethoxazole, clindamycin and gentamicin, possess staphylococcal cassette chromosome mec(SCCmec) type IV and Panton-Valentine Leukocidin (PVL).9,10There is still a lot of confusion regarding the prevalence of MRSA in the community due to difficulty in differentiating HA-MRSA and CA-MRSA.5A person may have become a carrier of MRSA during a hospital stay or following exposure to healthcare facility and transmit the pathogen in the community when he enters it.11 Such infections can be rightly called as community-onset MRSA rather than CA-MRSA.12
Epidemiology
Patients infected with CA-MRSA and carriers are the most common sources of infection. Infections are commonly seen among children and young adults.13According to CDC, athletes and other sports participants, military recruits, children, Pacific islanders, Alaskan natives, Native Americans, men who have sex with men and prisoners are at increased risk of CA-MRSA infections.7 Factors associated with spread of CAMRSA are overcrowding, sharing of contaminated items and surfaces, skin to skin contact, cuts and abrasions on skin and improper maintenance of hygiene and personal cleanliness.14,15 MRSA carriage is a significant risk factor for subsequent development of skin and soft tissue infection (SSTI).15 High CA-MRSA carrier state is seen in people living in mud-thatch houses where there is overcrowding, lack of hygiene, space and ventilation.16 A single clone of CA-MRSA is present in few regions whereas many clones may be responsible for infections in other parts of the world.17The most common clone prevalent in North America is pulse-field type USA300 mostly causing SSTI, bacteraemia, necrotizing fasciitis and severe pneumonia.18-20 USA400 is the second most common clone predominant in Alaska causing SSTI and fulminant sepsis.21 Most common clones seen in Europe and Australia are ST80 MRSA IV and ST93 MRSA IV respectively.17 ST59 MRSA IV/V is seen in Taiwan. However, limited data is available from Asia.17 In spite of all the differences in definitions of CAMRSA and limited number of population based studies, high incidence of CA-MRSA has been reported.5Cynthia and colleagues observed a rise in prevalence of CA-MRSA from 17% in 1999 to 56% in 2003.22 Previous studies have shown a difference in the rate of CA-MRSA infections varying from 10.9% to 29%.11,23,24 In an international surveillance study conducted by Song et al., prevalence of CA-MRSA in Asian countries was 25.5% of which India accounted for 4.3%.25 The study also suggested that CA-MRSA with various genotypic characteristics have spread from community to hospitals and major endemic HA-MRSA strains have spread from hospital to community in some Asian countries.25
Virulence Factors
CA-MRSA is known to produce many virulence factors
1. Cell wall polymers
Cell wall polymers include peptidoglycan and teichoic acid which have been implicated in shock.26,27
2. Cell wall proteins
Adherence of CA-MRSA to host tissue is mediated by cell surface proteins called Microbial Surface Components Recognizing Adhesive Matrix Molecules (MSCRAMMs).27 MSCRAMMs like clumping factor, fibronectin-binding proteins and protein A bind to host cell components like fibrinogen, fibronectin and Fc portion of Immunoglobulin G respectively.27 Other cell surface proteins include iron regulated proteins, polysaccharide intercellular adhesins and capsular polysaccharides.28MSCRAMMs are implicated in bone and joint infections and endovascular infections.27 One of the important MSCRAMMs in CA-MRSA, collagen adhesin protein is important in the pathogenesis of septic arthritis and osteomyelitis.29,30The microcapsule present in a few clinical isolates of CA-MRSA help in evading host defenses by its antiphagocytic activity and induce abscess formation.31A novel gene cluster bsa (bacteriocin of S.aureus) helps in invading an established microbial community and is implicated in quorum sensing and intercellular communication.27,32 CA-MRSA also have better tolerance to salt which may help colonization on skin
3. Enzymes
CA-MRSA has the ability to produce different enzymes like coagulase, staphylokinase, lipase, deoxyribonulease, protease and elastases which contribute to the pathogenesis of this organism.27 USA300 harbours a genomic island termed “arginine catabolic mobile element” (ACME) which encodes an arginine deaminase pathway.27 Arginine deaminase, a known virulence factor may further enhance the pathogenesis of CAMRSA
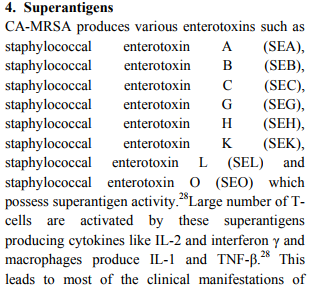
staphylococcal food poisoning, toxic shock syndrome (TSS) like illness and also epidemic furunculosis and necrotizing pneumonia.5,26 Superantigens SEB, SEC, SEA and SEH are produced by most of CA-MRSA isolates.5 SEB and SEC are implicated in non-menstrual TSS.28
5. Cytotoxins
Cytotoxins like α, β, γ, δ toxins and PVL are produced by CA-MRSA, which are hemolytic and toxic to leukocytes respectively.28
Panton-Valentine Leukocidin (PVL): Most CAMRSA carry pvl genes encoding for the PVL toxin, suggesting its role in virulence.33PVL is an extracellular bi-component toxin produced as two non-associated secreted proteins LukS-PV and LukF-PV.33 LukS-PV is dimerized with LukF-PV after connecting to the polymorphonuclear cell membrane forming a heptamer.5 PVL targets and induces leukocyte death by creating pores in the cell membrane releasing cytokines and intracellular proteases.1 PVL at low concentration causes apoptosis by forming pores in mitochondrial membrane.34 Horizontal transmission and clonal expansion of pvl genes leads to spread among CA-MRSA isolates.35 However studies reveal that PVL negative CAMRSA infections result in a worse outcome of SSTI when compared to PVL positive CAMRSA.36 Few β-lactam antibiotics enhance PVL production while antibiotics like clindamycin inhibit its production.37 α-toxin is a pore-forming toxin similar to PVL and causes dermonecrosis.5 It does not target neutrophils but lyses other cells like RBCs, macrophages, lymphocytes, platelets and fibroblasts.6,38
6. Epidermolytic / Exfoliative toxins CA-MRSA also produce exfoliative toxins such as exfoliative toxin A and B (eta and etb) that cause staphylococcal scalded skin syndrome and bullous impetigo.39
Molecular Properties
Hartman and colleagues described the mechanism of methicillin resistance attributed to PBP 2a – an altered penicillin binding protein with reduced affinity to methicillin.40 SCCmec, a mobile DNA element carries the mecA gene in a mec gene complex, which encodes PBP2a.41 It also carries direct repeat sequences, integration site sequence and chromosome cassette recombinase (ccr) gene in a ccr gene complex which integrates and excises SCCmec. 41 Eight SCCmec types have been identified – Type I to VIII depending on the class of mecA gene and the type of ccr gene complex.41 No drug resistant determinants other than mecA has been associated with types I, IV and V, while multiple drug resistance determinants are seen in types II and III.5 Due to the small size of SCCmec IV, it can be transferred horizontally to other species resulting in a higher degree of methicillin resistance amongCA-MRSA whereas SCCmec II and III, due to their large size, can be transferred vertically on selective antibiotic pressure as seen in HAMRSA.42Horizontal exchange of genes among Staphylococci has been further supported by identifying a few sequences of SCCmec IV identical in S.epidermidis.43 CA-MRSA that carry SCCmec IV also grow faster and reach high numbers in an infection.44 Theyare susceptible to a wide range of non β lactam antibiotics with susceptibility profile similar to that prevalent among methicillin susceptible S. aureus (MSSA).6,44 CA-MRSA associated with SCCmec IV cause SSTI (87.6%) and are recovered in high numbers in children than adults.45
Clinical Significance
Infections caused by CA-MRSA are similar to those caused by S. aureus except for a few that have arisen in epidemic proportions like SSTI and necrotizing pneumonia.6 Skin infections are the most common clinical manifestation seen with CA-MRSA. The appearance of red lesions is usually confused with spider bites and may be ignored by the clinicians.14 Such lesions have the tendency to develop necrotic areas.14 Furunculosis is the most common clinical presentation associated with CAMRSA.5However, in a previous study done in Mangalore, deep abscesses were seen in 83% of patients in comparison to 16.7% patients with superficial skin infections.46 Several cases of impetigo, bullous impetigo due to CA-MRSA have been described although 17-20% of S.aureus isolated from bullous impetigo in Japan were PVLnegative CA-MRSA.47,48 PVL producing CAMRSA is responsible for another major clinical presentation- necrotizing pneumonia leading to septic shock and respiratory distress syndrome with high mortality.49 CA-MRSA also causes necrotizing fasciitis, musculoskeletal infections and septic arthritis.50-52Toxins are also responsible for post antibiotic diarrhoea.53
Laboratory Diagnosis
CA-MRSA should be considered in the differential diagnosis of purulent SSTI.8Clinical specimens should be collected based on the site and type of infection and processed without delay. Gram stain of the specimen can give an immediate clue of staphylococcus infection. Further, culture of the specimen on blood agar is needed to isolate the organism. Once isolated, S.aureus is identified by standard procedures involving colony morphology, gram stain, catalase test and coagulase test.54 Clinical Laboratory Standards Institute (CLSI) recommends disk diffusion test using cefoxitin (30 µg) disc for identifying methicillin resistance as it is a better inducer of mecA gene.55Alternative methods include latex agglutination test for PBP2a and agar screen method using Mueller-Hinton agar with 6 µg/ml oxacillin and NaCl (4% w/v).56 Chromogenic media like ChromID MRSA, MRSASELECT can also be used for detection of methicillin resistance among isolates.57 PCR can be used for the detection of mecA gene that encodes for altered PBP.57 Further typing of CA-MRSA can be done using various methods like SCCmec typing, pulsed-field gel electrophoresis (PFGE), multilocus sequence typing (MLST) and S.aureus protein A (spa) typing.58 SCCmec typing is done using PCR for the detection of the class of mecA gene complex and the type of ccr gene complex.54
Treatment of CA-MRSA Infections
A new approach in empiric antibiotic therapy and management of staphylococcal infection is needed due to the emergence of MRSA in the community.5 For severe life-threatening infection and for infections among patients with associated risk factors,vancomycin should be used for empiric therapy.5 In low CA-MRSA prevalent regions,less severe infections and for patients with absence of healthcare risk factors, empirical therapy with first generation cephalosporin is adequate.5 Infections are generally not treated with fluoroquinolones as first line due to the risk of developing drug resistance.14 High resistance of MRSA to quinolones was reported in a previous study.59Clindamycin is one of the most common antibiotics used for empiric therapy of CA-MRSA infections, co-trimoxazole is preferred when inducible clindamycin resistance is detected.5 However, co-trimoxazole must be avoided in paediatric cases less than 8 years due to the reported contraindications.14 Non-antibiotic management of CA-MRSA infections have to be considered as drainage can manage many SSTI and must be considered as an adjunct to drug therapy.5 Simple skin infections caused by CA-MRSA can be treated with hot soaks, elevation, topical therapies, incision and drainage.6 Proper drainage and debridement can resolve cutaneous abscesses. Hospitalization and parenteral therapy may be necessary for more severe CAMRSA infections.5 Efforts should be made to collect appropriate specimens for culture and susceptibility testing in areas with high MRSA prevalence and / or in
Prevention
Basic principles for prevention of CA-MRSA infection as recommended by CDC include hand hygiene, avoiding sharing of personal hygiene items, covering draining wounds, early management of infections, environmental cleanliness and sterilization.14Patients should be isolated with implementation of contact precautions if confirmed positive for MRSA infection or colonization.5 Since nasal colonization is associated with recurrent pyoderma, nasal culture can be done for individuals at high risk.5Due to high mortality and morbidity associated with systemic invasive CAMRSA infections, it is better to screen and treat colonization with mupirocin among individuals with recurrent skin infections and their contacts.5 This however is not recommended for general population due to the possibility of the development of drug resistance.5
CONCLUSION
CA-MRSA has emerged in recent years as an important community acquired pathogen. To date, the true incidence of CA-MRSA infection is not known in many countries because most studies have characterized this organism in a relatively small group of patients over a short, fixed time interval. CA-MRSA differs from HA-MRSA in producing PVL, the type of infections caused and antibiotic resistance pattern. Normally, CA-MRSA is more susceptible to antibiotics such as tetracyclines, clindamycin, co-trimoxazole and gentamicin. It usually causes SSTIs, but can also cause severe deep seated infections such as necrotizing pneumonia. Early diagnosis and prompt treatment help in the management of the cases. In recent years, there have been reports of CA-MRSA causing hospital infections. Transmission of SCCmec IV via plasmids or bacteriophages could create bacteria that have antibiotic resistance of HA-MRSA and the virulence of CA-MRSA.
ACKNOWLEDGEMENT
The authors are thankful to Manipal University for providing continuous academic support. Authors are thankful to the Head of the Institution and Head of the Department of Microbiology, Kasturba Medical College, Mangalore (A constituent college of Manipal University) for their encouragement and support. The authors acknowledge the immense help received from the scholars whose article are cited and included in the references of this manuscript. The authors are also grateful to authors / editors / publishers of all these articles, journals and books from where the literature to this article has been reviewed and discussed.
References:
REFERENCES
1. Wijaya L, Hsu LY, Kurup A. Communityassociated methicillin-resistant Staphylococcus aureus: overview and local situation.Ann Acad Med Singapore 2006; 35:479-86.
2. Ray P, Goutam V, Singh R. Methicillinresistant Staphylococcus aureus (MRSA) in developing and developed countries: implications and solutions.Regional Health Forum 2011; 15:74-82.
3. Otto M. Community-associated MRSA: A dangerous epidemic. Future Microbiol 2007; 2:457-9.
4. Centers for Disease Control and Prevention. Four paediatric deaths from communityacquired methicillin-resistant Staphylococcus aureus – Minnesota and North Dakota, 1997- 1999. JAMA 1999; 282:1123-5.
5. Zetola N, Francis JS, Nuermberger EL, Bishai WR. Community-acquired methicillin-resistant Staphylococcus aureus: an emerging threat. Lancet Infect Dis2005; 5:275–86.
6. Shenoy MS, Bhat GK, Kishore A, Hassan MK. Significance of MRSA strains in community associated skin and soft tissue infections. Indian J Med Microbiol 2010; 28:152-4.
7. Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) - Fact Sheet. [Internet] Department of Health, New York. (Reviewed 2013). Available from: http://www.health.ny.gov/diseases/communica ble/staphylococcus_aureus/methicillin_resistant /community_associated/fact_sheet.htm
8. Diagnosis and Testing of MRSA Infections [Internet]. Centers for Disease Control and Prevention 2010 (updated 2010 December 02). Available from: http://www.cdc.gov/mrsa/diagnosis/index.html
9. Vandenesch F, Naimi T, Enright MC, Lina G, Nimmo GR, Heffernan H, et al. Communityacquired methicillin-resistant Staphylococcus aureus carrying Panton-Valentine leukocidin genes: worldwide emergence. Emerg Infect Dis 2003; 9:978–84.
10. O’Brien FG, Lim TT, Chong FN, Coombs GW, Enright MC, Robinson DA, et al. Diversity among community isolates of methicillinresistant Staphylococcus aureus in Australia. J Clin Microbiol 2004; 42:3185–90.
11. Krishna BV, Patil AB, Chandrasekhar MR. Community-acquired methicillin-resistant Staphylococcus aureus infections in a South Indian city. Southeast Asian J Trop Med Public Health 2004; 35:371-4.
12. Salgado CD, Farr BM, Calfee DP. Communityacquired methicillin-resistant Staphylococcus aureus: A meta-analysis of prevalence and risk factors. Clin Infect Dis 2003; 36:131–9.
13. Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, et al. Comparison of community- and health careassociated methicillin-resistant Staphylococcus aureus infection. JAMA 2003; 290:2976–84.
14. Gorwitz RJ, Jernigan DB, Powers JH, Jernigan JA, Participants in the CDC Convened Experts’ Meeting on Management of MRSA in the Community. Strategies for clinical management of MRSA in the community: Summary of an experts’ meeting convened by the Centers for Disease Control and Prevention.[Internet] 2006. Available at http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca.ht ml.
15. Fritz SA, Epplin EK, Garbutt J, Storch GA. Skin infection in children colonized with community-associated methicillin-resistant Staphylococcus aureus. J Infect 2009; 59:394– 401.
16. Chatterjee SS, Ray P, Aggarwal A, Das A, Sharma M. A community-based study on nasal carriage of Staphylococcus aureus. Indian J Med Res 2009; 130:742-8.
17. Chua K, Laurent F, Coombs G, Grayson ML, Howden BP. Not community-associated methicillin resistant Staphylococcus aureus (CA-MRSA)!– A clinician’s guide to community MRSA- Its evolving antimicrobial resistance and implications for therapy. Clin Infect Dis 2011; 52:99-114.
18. Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, et al. Invasive methicillinresistant Staphylococcus aureus infections in the United States. JAMA 2007; 298:1763–71.
19. Tenover FC, Goering RV. Methicillin-resistant Staphylococcus aureus strain USA300: origin and epidemiology. J Antimicrob Chemother 2009; 64:441–6.
20. Hidron AI, Low CE, Honig EG, Blumberg HM. Emergence of community- acquired methicillin-resistant Staphylococcus aureus strain USA300 as a cause of necrotising community-onset pneumonia. Lancet Infect Dis 2009; 9:384–92.
21. David MZ, Rudolph KM, Hennessy TW, Boyle-Vavra S, Daum RS. Molecular epidemiology of methicillin-resistant Staphylococcus aureus, rural southwestern Alaska. Emerg Infect Dis 2008; 14:1693–9.
22. Maree CL, Daum RS, Boyle-Vavra S, Matayoshi K, Miller LG. Communityassociated methicillin-resistant Staphylococcus aureus isolates causing health care associated infections. Emerg Infect Dis 2007; 13:236-42.
23. Natarajaseenivasan K, Shanmughapriya S, Latha R, Artiflavia GB, Kanagavel M, Pragash DS. Prevalence of community acquired methicillin resistant Staphylococcus aureus (CA-MRSA) in skin and soft tissue infections among cases from Puducherry, India. J Public Health 2012; 20:593-7.
24. Nagaraju U, Bhat G, Kuruvila M, Pai GS, Jayalakshmi, Babu RP. Methicillin-resistant Staphylococcus aureus in community-acquired pyoderma. Int J Dermatol 2004; 43:412-4.
25. Song JH, Hsueh PR, Chung DR, Ko KS, Kang CI, Peck KR, et al: ANSORP study group. Spread of methicillin-resistant Staphylococcus aureus between the community and the hospitals in Asian countries: an ANSORP study. J Antimicrob Chemother 2011; 66:1061- 9.
26. Humphreys H. Staphylococcus. Greenwood D, Barer M, Richard S, Irving W editors. Medical Microbiology. A guide to microbial infection: Pathogenesis, immunity, laboratory investigation and control. 18th edition. Churchill livingstone.
27. Gordon RJ, Lowy FD. Pathogenesis of methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis 2008; 46:350–9.
28. Schlievert PM, Stransberd KL, Lin Y, Peterson ML, Leung DYM. Secreted virulence factor comparison between methicillin resistant and methicillin sensitive Staphylococcus aureus, and its relevance to atopic dermatitis. J Allergy Clin Immunol 2010; 125:39-49.
29. Elasri MO, Thomas JR, Skinner RA, Blevins JS, Beenken KE, Nelson CL, et al. Staphylococcus aureus collagen adhesin contributes to the pathogenesis of osteomyelitis. Bone2002; 30:275–80.
30. Patti JM, Bremell T, Krajewska-Pietrasik D, Abdelnour A, Tarkowski A , Ryden C, et al. The Staphylococcus aureus collagen adhesin is a virulence determinant in experimental septic arthritis. Infect Immun1994; 62:152–61.
31. Tzianabos AO, Wang JY, Lee JC. Structural rationale for the modulation of abscess formation by Staphylococcus aureus capsular polysaccharides. Proc Natl Acad Sci U S A 2001; 98:9365–70.
32. Miller M, Bassler B. Quorum sensing in bacteria. Annu Rev Microbiol2001; 55:165–99.
33. Watkins RR, David MZ, Salata RA. Current concepts on the virulence mechanisms of methicillin-resistant Staphylococcus aureus. J Med Microbiol 2012; 61:1179-93.
34. Genestier AL, Michallet MC, Pre´ vost, G, Bellot G, Chalabreysse L, Peyrol S, et al. Staphylococcus aureus Panton-Valentine leukocidin directly targets mitochondria and induces Bax-independent apoptosis of human neutrophils. J Clin Invest 2005; 115:3117–27.
35. O’Hara FP, Guex N, Word JM, Miller LA, Becker JA, Walsh SL, et al. A geographic variant of the Staphylococcus aureus PantonValentine leukocidin toxin and the origin of community-associated methicillin-resistant S.aureus USA300. J Infect Dis 2008; 197:187– 94.
36. Bae IG, Tonthat GT, Stryjewski ME, Rude T H, Reilly LF, Barriere SL, et al. Presence of genes encoding the Panton-Valentine leukocidin exotoxins is not the primary determinant of outcome in patients with complicated skin and skin structure infections due to methicillin resistant Staphylococcus aureus: results of a multinational trial. J Clin Microbiol 2009; 47:3952–7.
37. Dumitrescu O, Choudhury P, Boisset S, Badiou C, Bes M, Benito Y, et al. Beta-lactams interfering with PBP1 induce Panton-Valentine leukocidin expression by triggering sarA and rot global regulators of Staphylococcus aureus. Antimicrob Agents Chemother 2011; 55:3261– 71.
38. Rybak MJ, LaPlante KL. Communityassociated methicillin-resistant Staphylococcus aureus: A review. Pharmacotherapy 2005; 25:74-85.
39. Yamaguchi T, Yokota Y, Terajima J, Hayashi T, Aepfelbacher M, Ohara M, et al. Clonal association of Staphylococcus aureus causing bullous impetigo and the emergence of new methicillin-resistant clonal groups in Kansai district in Japan. J Infect Dis2002; 185:1511-6.
40. Hartman B, Tomasz A. Altered penicillinbinding proteins in methicillin-resistant strains of Staphylococcus aureus. Antimicrob Agents Chemother 1981; 19:726-35.
41. Teruyo Ito. International Working Group on the Classification of Staphylococcal Cassette Chromosome Elements (IWG-SCC). Classification of Staphylococcal cassette chromosome mec (Sccmec): Guidelines for reporting novel SCCmec elements. Antimicrob Agents Chemother 2009; 53:4961–7.
42. Berglund C, Mo¨lling P, Sjo¨berg L, So¨derquist B. Predominance of staphylococcal cassette chromosome mec (SCCmec) type IV among methicillin-resistant Staphylococcus aureus (MRSA) in a Swedish county and presence of unknown SCCmec types with Panton-Valentine leukocidin genes. Clin Microbiol Infect 2005; 11: 447–56.
43. Mongkolrattanothai K, Boyle S, Murphy TV, Daum RS. Novel non-mecA containing staphylococcal chromosomal cassette composite island containing pbp4 and tagF genes in a commensal staphylococcal species: a possible reservoir for antibiotic resistance islands in Staphylococcus aureus. Antimicrob Agents Chemother2004; 48:1823–36.
44. Okuma K, Iwakawa K, Turnidge JD, Grubb WB, Bell JM, O’Brien FG, et al. Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community. J Clin Microbiol2002; 40: 4289–94.
45. Kilic A, Li H, Stratton CW, Tang YW. Antimicrobial susceptibility patterns and staphylococcal cassette chromosome mec types of, as well as panton valentine leukocidin occurrence among methicillin-resistant Staphylococcus aureus isolates from children and adults in Middle Tennessee. J Clin Microbiol 2006; 44:4336-40.
46. Mandelia C, Shenoy S. Community associated-methicillin resistant Staphylococcus aureus in skin and soft tissue infections. J Clin Diagn Res 2010; 4:2673-7.
47. Liassine N, Auckenthaler R, Descombes MC, Bes M, Vandenesch F, Etienne J. Communityacquired methicillin-resistant Staphylococcus aureus isolated in Switzerland contains the Panton-Valentine leukocidin or exfoliative toxin genes. J Clin Microbiol2004; 42:825–8.
48. Takizawa Y, Taneike I, Nakagawa S, Oishi T, Nitahara Y, Iwakura N, et al. A PantonValentine leucocidin (PVL)-positive community-acquired methicillin-resistant Staphylococcus aureus (MRSA) strain, another such strain carrying a multiple-drug resistance plasmid, and other more-typical PVL-negative MRSA strains found in Japan. J Clin Microbiol 2005; 43:3356-63.
49. Lina G, Pie´mont Y, Godail-Gamot F, Bes M, Peter MO, Gauduchon V, Vandenesch F, et al. Involvement of Panton-Valentine Leukocidin– producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis 1999; 29:1128–32.
50. Miller LG, Perdreau-Remington F, Rieg G, Mehdi S, Perlroth J, Bayer AS, et al. Necrotizing fasciitis caused by communityassociated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med 2005; 352:1445-53.
51. Thangarajah T, Neal TJ, Kennedy TD. An unexpected diagnosis of methicillin-resistant Staphylococcus aureus septic arthritis. Orthop Rev 2009; 1:e13.
52. Martinez-Aguilar G, Avalos-Mishaan A, Hulten K, Hammerman W, Mason EO Jr, Kaplan SL. Community-acquired, methicillinresistant and methicillin-susceptible Staphylococcus aureus musculoskeletal infections in children. Pediatr Infect Dis J 2004; 23:701-6
53. Gravet A, Rondeau M, Harf-Monteil C, Grunenberger F, Monteil H, Scheftel JM, et al. Predominant Staphylococcus aureus isolated from antibiotic-associated diarrhea is clinically relevant and produces enterotoxin A and the bicomponent toxin LukE-lukD. J Clin Microbiol 1999; 37: 4012–9.
54. Lo J YC. Laboratory Diagnosis of CA-MRSA. The Hong Kong Medical Diary 2007; 12:1-3.
55. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial disc diffusion tests; Twenty-Third Informational Supplement. CLSI document M100-S232. CLSI 2013.
56. Laboratory detection of oxacillin/methicillin resistant Staphylococcus aureus.[Internet] Centers for Disease Control and Prevention (2010), Available at : http:www.cdc.gov/mrsa/lab/lab-detection.html.
57. Matouskova I, Janout V. Current knowledge of methicillin-resistant Staphylococcus aureus and community-associated methicillin resistant Staphylococcus aureus. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2008; 152:191-202.
58. Aires-de-Sousa M, Boye K, de Lencastre H, Deplano A, Enright MC, Etienne J, et al. High interlaboratory reproducibility of DNA sequence-based typing of bacteria in a multicenter study. J Clin Microbiol 2006; 44:619-21
59. Chacko J, Kuruvila M, Bhat GK. Factors affecting the nasal carriage of methicillin resistant Staphylococcus aureus in human immunodeficiency virus-infected patients. Indian J Medical Microbiol 2009; 27:146-8.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License