IJCRR - 6(10), May, 2014
Pages: 126-133
Print Article
Download XML Download PDF
PTERYGOSPINOUS BAR AND MULTIPLE CIVININI FORAMEN- A RARE ANATOMICAL VARIANT AND ITS CLINICAL IMPLICATIONS
Author: Thomson Jones Ebenraj, NagarajanVishali
Category: Healthcare
Abstract:Objectives: Our aim is to study the prevalence of Pterygospinous bar and analyzemorphometrically the homonyms foramen in a collection of existing skulls and discuss their clinical implications. Methods: 90 dried adult human skulls were used for the study. The base of the skull was examined both macroscopically and radiologically for the presence of abnormal osseous structures extending from the lateral pterygoid plate. Average diameter of the Civinini's foramen, width of the lateral pterygoid plate, width of the extending bar from the pterygospinous process and sphenoid spine were measured using the vernier caliper. Results: Out of 90 skulls reviewed, only 5 skulls showed the presence of complete pterygospinous bar with enclosed Civinini's foramen, in which 2 skulls showed the multiple Civinini's foramen. 58 skulls showed the presence of incomplete pterygospinous bar. Conclusion: It is obvious from the results that the incomplete pterygospinous bar is more prevalent, which may lead to altered course of the structures passing through foramen ovale and foramen spinosum. Some of the structures may also be entrapped in the enclosed Civnini's foramen there by resulting in neural and vascular complications. Hence, the vivid knowledge of such presence is highly beneficial to anaesthetists, dental and maxillo \? facial surgeons in day to day clinical practice.
Keywords: pterygospinous ligament, pterygospinous bar, civinini’s foramen, lateral pterygoid plate, spine of the sphenoid.
Full Text:
INTRODUCTION
The cranial base is an important region for it provides attachments to muscles of mastication, deep muscles of neck and also for the presence of foramina which provides the means by which vessels and nerves enters or leaves the cranial cavity. The abnormal bony growths such as spines, spurs, tubercles or bony plates may be due to abnormal ossification or overgrowths of surrounding parts of the bones around the foramen of base of the skull, which may lead to ischemia, necrosis and potential paralysis of the parts of the body being supplied, drained or innervated by its contents. There were many ligaments in the exocranial region. One such ligament is the pterygospinous ligament, described by Civinini in 1829 (1), that connects the spinous process of the sphenoid bone to the Civinini’s spine located in the posterior margin of the lateral pterygoid lamina of the sphenoid bone. Complete ossification of the pterygospinous ligament is known as pterygospinous bar (2).When completely ossified the pterygospinous ligament form the Civinini’s foramen. (3; 4;) Ossification of these ligaments can be important as to relate with the adjacent anatomic structures. In adults, these unique ossification leads to spoil the interrelationships of the anatomic configuration. Such abnormal osseous structures may alter the normal course of the mandibular nerve or its branches and they can cause serious implications in accessing the oval foramen in a therapeutic approach, in any surgical intervention in the region and may lead to false neurological differential diagnosis. Therefore, the anatomical knowledge of physician should be accurate to overcome the anatomic variations and diversity so as to provide success. Accordingly, the present study was designed to find out the osseous structure especially the pterygospinous bar in the available dry human skulls.
MATERIALS AND METHODS
The study was carried out using 90 dried adult human skulls irrespective of age and gender, were obtained from Department of anatomy, Asan memorial dental college and Hospital and Karpaga Vinayaga institute of dental sciences. Skulls that are evident of abnormalities such as distress or obvious morphological asymmetries were expelled from this study. The base of the skull was examined both the sides macroscopically for the presence of anomalous osseous structures from the lateral pterygoid plate. The presence of a rare variant ossified ligament connecting the spine of the sphenoid and the lateral pterygoid plate was noted in all these bone specimens. As described by Suazo et al.,2010; the following descriptions are given for ossification of the ligament: Type I: Complete ossification of pterygospinous ligament: there is a bony bridge that leads from the pterygospinous process to the apex of the sphenoid spine. In this case, it is the pterygospinous foramen or Civinini’s foramen. Type II: Incomplete ossification of pterygospinous ligament: there is anexpansion of the pterygospinous process, but fails to contact the sphenoid spine. In this case, the pterygospinous foramen is partly formed. The specimen with ossified pterygospinous ligament was photographed and compared to that of the normal and the same was also subjected to radiological study. In case, there was complete ossification as in Type I the average diameter of its enclosed Civinini’s foramen was measured using a vernier caliper. The bar extending from the spine of the sphenoid and from the lateral pterygoid plate was also measured in Type II variety. Even the small gap left between the two bars making it incomplete pterygospinous bar was also noted using the Vernier Caliper. With the data obtained, prevalence rates of the two proposed types were estimated, differentiating the bilateral, left and right presentations.
RESULTS
Among the ninety skulls studied, twenty seven (30%) of the skulls did not have any abnormal osseous structures extending from the lateral pterygoid plate. Normal bone No bony projection from the plate of lateral lamina of the pterygoid process of the sphenoid bone. The lateral pterygoid plate was thin, flat and everted. The maximum width of the lateral pterygoid plate was measured to be 1.4 cm
Anomalous Osseous structure
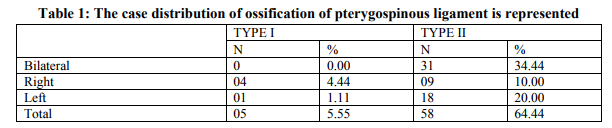
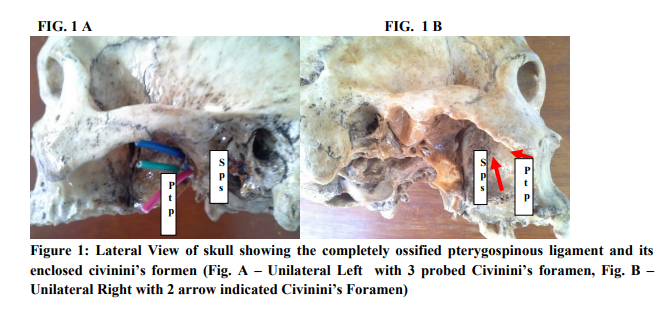
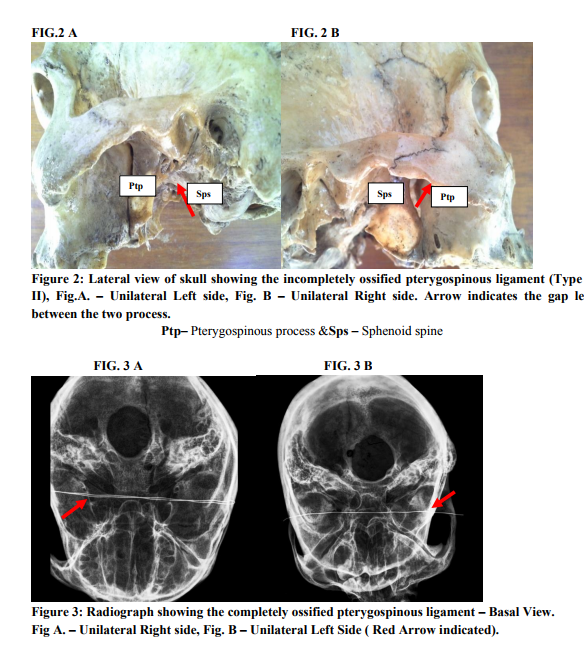
from the Lateral pterygoid plate:pterygoid plate: The following osseous structures were observed macroscopically and morphometrically extending from the lateral pterygoid plate: Type I i. In three(3.33%) skulls,unilateral (right side) complete pterygospinous ligament was noted. Ossified Pterygospinous ligament are present medial to the Foramen Ovale. Since the bar is complete, it presented a complete Civinini’sforamen with an average diameter of 0.66mm (Fig.1). ii. In one (1.11%) another skull, unilateral (right side) complete pterygospinous ligament was noted. But it showed instead of a single Civinini’s foramen, it showed two variable foramen with an average diameter of about 0.7mm and 0.2 mm (Fig. 2) iii. In one another (1.11%) skull, unilateral (left side) complete pterygospinous ligament was noted. This skull also showed multiple Civinini’s foramen of variable size with an average diameter of about 0.6 mm, 0.4 mm and 0.3 mm (Fig. 3) Type II i. Rarely, in thirty one (34.44%) skulls, bilateral incomplete pterygospinous ligament was observed. The bony projection from the lateral pterygoid plate was pointing towards the spine of the sphenoid which we presume, is the ossified part of the pterygospinous ligament which is incomplete as there was asmall gap between the spine of the sphenoid
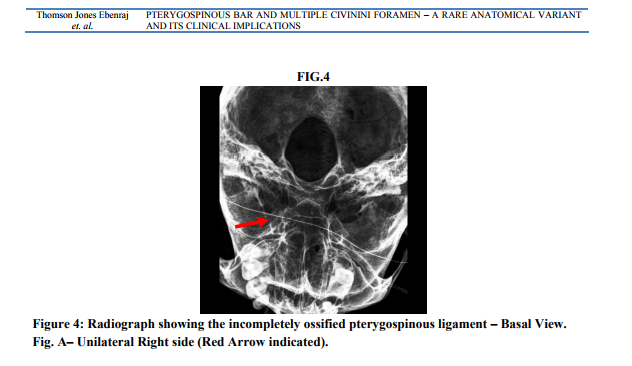
and the posterior border of the lateral pterygoid plate. ii. The nine (10.00%) skulls showed unilateral (right side) incomplete pterygospinous ligament, in which one skull showed their presence inferior to the foramen ovale so that it is divided into medial and lateral compartments. iii. In 18 (20.00%) skulls, unilateral (left side) incomplete pterygospinous ligament was observed. Of which 10 – 12% of the variety showed the presence of the bar overlying the foramen spinosum dividing it into medial and lateral compartments. iv. The projection from the lateral pterygoid plate measured 7 mm, while the projection from the spine measured 4.6 mm. Thus two projections from the lateral projection plate and the spine of sphenoid approached each other and left a deficit of 6 mm between them.
DISCUSSION
In the cranial base there are strings of intrinsic ligaments in relation to sphenoid bone: interclinoid, caroticoclinoid, pterygospinous and pterygoalar ligaments. Ossification process with different clinical implications has been reported for all. The incidence of pterygospinous bony bridges has beenreported by different authors with different results. Wood-Jones (1931) reported an 8% pterygospinous ligament ossification inHawaiian skulls. Nayak et al. (2007) indicated that such bridges were completelyossified in 5.76% of the cases analyzed by them. Pekeret al. (2002)reported the presence of this bridge in 8.8% skulls of an Anatolianpopulation. In this study, the prevalence of complete pterygospinousligament ossification was only 5.55%, lower than those reported by 6 and 7; and much closer to Nayak et al(2007) studies. The study also confirmed the presence of incomplete pterygospinous bar of a greater range (64.44%). This could be attributed to the age of this sample(average 52.4years), as the emergence of ossification process isassociated with increasing
age of subjects (8) and incomplete presence can be ascribed to the incomplete process of ossification. Although there are reports on the presence of ossified pterygospinous ligament, there is dearth of literature on the radiological study of the pterygospinous ligament. The earliest description of the ossified pterygospionous ligament radiologically was done by De Froe and Wagener,1935 (10) . The complexity of the pterygomaxillary region may not have prompted too many scientists to explore the region radiographically. The present study analyzed both morphologically and radiologically the presence of total or partial pterygospinous ligaments ossification and its enclosed Civinini’s foramen. The present study also exposed the presence of multiple Civinini’s foramen which may be involved in multiple complications involving both vascular and nervous compression. The present observation on unilateral presence of pterygospinous bar in 5 skulls out of 90 cases (i.e. 5.55 % incidence) makes the study clinically important. The maximum width of the lateral pterygoid plate in the anomalous bone was 2.1 cm, where as in the normal cases it was 1.4 cm. These results clearly state that the lateral pterygoid plate was very much wider in the anomalous bone specimen. Theosseous bar formations are present deep in the infra temporal fossa establishing important relationships with the two foramen and structures passing through it such as mandibular nerve and its branches through foramen ovale, the middle meningeal artery and vein passing through foramen spinosum, and other structures in the region include the otic ganglion, the chorda tympani nerve, the medial and lateral pterygoideus muscles. These structures are compressed against bone formations and are capable of generating clinically important alterations(11;12). It has been reported that the mandibular nerve has some of its branches passing through the Civinini’sforamen formed as a result of presence of such osseous bar (ossification of pterygospinous ligament) and may compress upon the branches of the mandibular nerve (13). In view of the close relationship of the chorda tympani nerve, it may also be compressed by the anomalous bar of bone (11). Involvement of the chordatympani nerve would then result in the impairment of the taste sensation to the anterior two – third of the tongue. This would lead to a clinical condition like lingual numbness, speech impairment and mandibular neuralgia (14). The incomplete bars formed are in relation to either foramen ovale or spinosum dividing it into medial and lateral compartments. The lingual nerve, the inferior alveolar branch of mandibular nerve and the middle meningeal vessels in the region of the infratemporal fossa are forced to take a long curved course in presence of a large pterygoid plate (12) and during contraction of the pterygoid muscles, these nerves and vessels are subjected to compression(15).Hence, the presence this large lamina of the lateral pterygoid plate causes clinical symptoms (12) It has to be remembered that while applying conductive anaesthesia on mandibular nerve by lateral subzygomatic route, one may encounter variable ossified formations at lateral pterygoidplates’s posterior border of pterygoid process thereby acing as an obstacle to high - quality conductive anaesthesia (13). Thus, lateral pterygoid plate forms an important landmark for mandibular anaesthesia and any anomalies in the lateral pterygoid plate is bound to confuse anaesthetists (16). A research study had also advocated that a distance of approximate 0.25 cm beyond the distance to the lateral pterygoid plate be taken, while performing maxillary block by the lateral extraoral approach (17). Its presence may also cause the failure of anaesthesia during the treatment of trigeminal neuralgia as reported by an earlier research (18). It is also been reported that thermo-coagulation of the trigeminal ganglion becomes difficult in the presence of this bar (16). The presence of the ossified pterygospinous ligament means that there would be less accessible
space to gain entry into para and retro pharyngeal spaces (12). The skiagram (Fig.3A, 3B and 4) obtained in the present case depicts that there is very little space for surgeons to gain entry into para and retropharyngal space.
CONCLUSION
The presence of ossified pterygospinous ligament is an unusual finding, which may not be detected unless indicative, the cause of which may be very difficult to establish. The incidence of the ossified pterygospinous ligament has been reported by different authors with different results. The disparity could be attributed to the age of the sample (avg. 50) as the emergence of ossification process is associated with increasing age of subjects. The awareness on the anatomical variations in this region is very important for surgeons, anaesthetists, radiologists and neurologists. As the ossified pterygospinous ligament which can be complete or incomplete, is a very rare finding and can produce various symptoms depending upon the nerve compression. The presence of such osseous bar can produce nerve entrapment syndrome and can interfere with surgical or anaesthetic procedures. The knowledge increases the successful rate of the surgical procedures and helps in curing painful conditions which results from nerve compression. The present study also reported the presence of multiple Civinini’s foramina which would result in many clinical complications relatively nervous or arterial as the structures compressed passing through such abnormal enclosed foramina. As per our knowledge such abnormal osseous variations with many such enclosed foramina were not reported in the modern medical literature. Thus, the anatomical knowledge of such ossified pterygospinous ligament may be beneficial for anaesthetists, dental and maxilla – facial surgeons in day – to - day clinical practice.
ACKNOWLEDGEMENT
Dr. GirijaSivakumar, Head of the Department, Karpaga Vinayaga Institute of Dental Sciences for providing us the additional study material. Dr. K. Jagannathan, Principal, Asan Memorial Dental College and Hospital for the constant support rendered during the proceeding of this work.
References:
REFERENCES
1. Tebo HG. The pterygospinous bar in panoramic roentgenography. Oral Surg Oral Med Oral Pathol 1968; 26: 654-657.
2. Antonopoulou M, Piagou M, Anagnostopoulou S. An anatomical study of the pterygospinous and pterygoalar bars and foramina – their clinical relevance. JCraniomaxillofacSurg 2008; 36:104-108.
3. Nayak SR, Saralaya V, Prabhu LV, Pai MM, Vadgaonkar R, D’Costa S. Pterygospinous bar and foramina in Indian skulls: incidence and phylogenetic significance. SurgRadiol Anat. 2007; 29: 5-7.
4. Shaw JP. Pterygospinous and pterygoalar foramina: a role in the etiology of trigeminal neuralgia? Clin. Anat. 1993; 6: 173-178.
5. Suazo, G. I.; Zavando, M. D.; Smith, R. L. Anatomical study of the pterygospinous and pterygoalar bony bridges and foramens in dried crania and its clinical relevance. Int. J. Morphol., 2010; 28(2):405-408.
6. Wood-Jones, F. The non-metrical Morphological Characters of the Skull as Criteria for Racial Diagnosis: Part II: The nonmetrical Morphological Characters of the Hawaiian Skull. J. Anat., 1931; 65(3):368-78.
7. Peker, T.; Karakose, M.; Anil, A.; Turgut, H. B. andGulekon, N. The incidence of basal sphenoid bony bridges in dried crania and cadavers; their anthropological and clinical relevance. Eur. J. Morphol., 2002; 40(3):171- 80
8. Cammisa, M.; De Serio, A. andGuglielmi, G. Diffuse idiopathic skeletal hyperostosis. Eur. J. Radiol., 1998; 27(1):S7–11.
9. De Froe A and Wagenaar J.H., Die Bedeutung des PorusCrotaphiticobuccinatorius and des foramen pterygospinosum for Neurologic and Rontgenolgie. Fort GebRontgenstr, 1935; 52: 64 -69.
10. Srijit Das and Shipra Paul. Ossified Pterygospinous ligament and its clinical implications. BratislLekListy 2007; 108 (3): 141 -143.
11. Peuker, E. T.; Fischer, G. and Filler, T. J. Entrapment of the lingual nerve due to an ossifedpterygospinous ligament. Clin. Anat. 2001; 14(4):282-4.
12. Von Ludinghausen, M.; Kageyama, I.; Miura, M. andAlkhatib, M. Morphological peculiarities of the deepinfratemporal fossa in advanced age Morphological peculiarities of the deep infratemporal fossa in advanced age. Surg. Radiol. Anat., 2006; 28(3):284-92.
13. Kapur, E.; Dilberovic´, F.; Redzepagic´, S. andBerhamovic´, E.Variation in the lateral plate of the pterygoid process and the lateral subzygomatic approach to the mandibular nerve. Med. Arh., 2000; 54(3):133-7.
14. Kim SY, Hu KS, Chung IH, Lee EW, Kim HJ, Topographic anatomy of the lingual nerve and variations in communication pattern of th mandibular nerve branches. SurgRadiolAnat 2004; 26, 128 -35.
15. Krmpotic´-Nemanic, J.; Vinter, I.; Hat, J. andJalsovec, D. Mandibular neuralgia due to anatomical variations. Eur. Arch.Otorhinolaryngol., 1999; 256(4):205-8.
16. Lang J., Skull base and related structures.Schattauer, Stuttgart, 1995: 300 - 311. 17. Singh B., Srivastava SK., Dang R., Anatomic Considerations in relation to the maxillary nerve block. Reg. Anesth Pain Med 2001; 26: 507 – 511.
18. Sweet WH. The treatment of trigeminal neuralagia (tic douloureux). New Engl J Med 1986; 315: 174 -177.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License