IJCRR - 6(10), May, 2014
Pages: 64-76
Print Article
Download XML Download PDF
COMPARISON OF 'CUT AND PASTE (USING FIBRIN GLUE)' VS 'CUT AND SUTURE (USING 8-0 VICRYL SUTURES)' TECHNIQUES OF PTERYGIUM SURGERY
Author: Kumar Nishant, Vireshwar Prasad, Asif Shahnawaz, Muazzam Ali Akbar
Category: Healthcare
Abstract:Background: In recent times, the universal trend toward simpler, quicker and more comfortable surgical procedures have fostered the development of suture-less techniques and hence use of fibrin glue for attaching conjunctival autograft after pterygium excision. Objectives: To assess and compare the mean surgical time, post-operative discomfort and recurrences among patients undergoing Pterygium excision and conjunctival autografting using fibrin glue; with Pterygium excision and conjunctival autografting using 8-0 Vicryl sutures. Materials and methods: 60 patients with primary pterygium randomized into two groups. Group A (n=30) underwent autografting using fibrin glue; Group B (n=30) underwent autografting using 8-0 Vicryl suture. P-value < 0.05 was considered statistically significant. Surgical times were noted as: Total surgical time from 1st conjunctival cut to removal of lid speculum, time for excision of pterygium and time to secure graft on the bed. Post operative discomfort was assessed using pretested questionnaires Results: Mean surgical time for Pterygium excision with conjunctival autografting using fibrin glue (15.86min) is significantly less as compared to sutures(27.93min); P=0.001. Post-operative discomfort was significantly less in cases of fibrin glue (10% patients) in comparison to suture group (56.6%patients). The observed difference between the recurrence rates in the group A (3.3%) and Group B (20%) was statistically significant. Conclusion: Fibrin glue reduces the surgical time, post-operative discomfort to the patients and has lower recurrence rates in comparison to conjunctival autografting using sutures following pterygium excision.
Keywords: Pterygium, Conjunctival autografting, 8-0 Vicryl suture, Fibrin glue
Full Text:
INTRODUCTION
Pterygium is one of the oldest diseases known in the history of medicine. It is a common condition in India, which is part of the ?Pterygium belt? described by Cameron1 . Besides the cosmetic appearance, the patient may complain of discomfort with recurrent redness of eye, swelling, tearing, burning sensation and occasionally pricking or gritty sensation. When the axial area of the cornea is invaded, vision gets increasingly affected. This occurs even before the Pterygium itself has reached the area, because of irregular astigmatism produced by corneal folds. In advanced Pterygium, ocular motility may be restricted leading to diplopia in certain field of gaze. Though the disease is known since time immemorial, no satisfactory treatment has yetbeen evolved up till now. Among the eye diseases which often are prone to recurrence, Pterygium is one of the commonest. The treatment of Pterygium is mainly surgical. A wide range of surgical maneuvers for removal of Pterygium have been reported. Bare sclera is the simplest method of Pterygium excision but is associated with a very high recurrence rate ranging from 24% to as high as 89%. Pterygium recurrence after bare sclera excision may be highly aggressive and in severe cases ocular morbidity may far exceed the primary lesion. To avoid this, adjunctive treatment such as ß-irradiation, Thiotepa, Mitomycin-C, 5-Fluorourail etc are used. Newer techniques include conjunctival autografting with or without limbal stem-cell transplantation and amniotic membrane grafting. Of all these newer methods, conjunctival autografting is most commonly performed and is associated with low rates of recurrences. The autograft can be attached to bare sclera with the help of 8-0 Vicryl suture; this is associated with increased surgical time, more post-operative pain, discomfort, watering and prolonged healing time. In recent times, the universal trend toward simpler, quicker and more comfortable surgical procedures have fostered the development of sutureless techniques and hence use of tissue adhesives for attaching conjunctival autograft. This technique claims to reduce the surgical time, cause less postoperative pain, irritation, watering, induce less inflammation, reduce healing time and recurrences. Fibrin glue is the most recent among all adhesives and is gaining acceptance world over for use in treatment of various ocular conditions. RelisealTM (manufactured by Reliance Life Sciences)is a two component tissue adhesive namely human fibrinogen and human thrombin. The resultant mixture simulates the natural physiological phenomenon of blood clotting at the bleeding site and forms a viscous clot. Thus, the formed clot acts like a seal to arrest bleeding or glue tissues. The fibrin clot also supports wound
healing process. It gets absorbed over several days to weeks by the naturally occurring endogenous fibrinolytic enzymes. Hence, a study was conducted to assess and compare the mean surgical time, post-operative discomfort and recurrences among patients undergoing Pterygium excision and conjunctival autografting using fibrin glue; with Pterygium excision and conjunctival autografting using 8-0 Vicryl sutures.
MATERIALS AND METHODS
In view of different techniques for Pterygium surgery, a prospective hospital based study has been conducted during March 2010 to September 2011to compare ?Cut and paste (Sutureless) technique‘ with ?Cut and suture technique‘ of pterygium surgery in terms of mean surgical time, postoperative discomfort and complications and recurrences. Written informed consent was obtained from all the participants before enrolment in the study and clearance from Institution‘s Ethics Committee was taken
Inclusion Criteria:
Study population was selected from the patients attending Ophthalmology Out-patient Department of the hospital with primary pterygium. Selected patients (total number 60) were randomly divided into 2 groups: Group A (n=30 patients): Corneo-scleral resection of pterygium with conjunctival autografting using Fibrin Glue. Group B (n=30 patients): Corneo-scleral resection of pterygium with conjunctival autografting using 8-0 Vicryl Sutures. Exclusion Criteria: 1. Cases with cystic, atrophic or inflamed pterygia. 2. Patients with associated ocular surface disorders like Sjogren‘s syndrome. 3. Patient with recurrent pterygia. 4. Pregnant patients and lactating mothers.All patients in the study were subjected to a thorough general and ocular examination.
METHODOLOGY
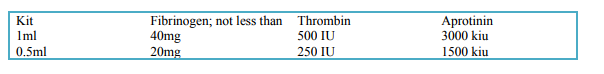
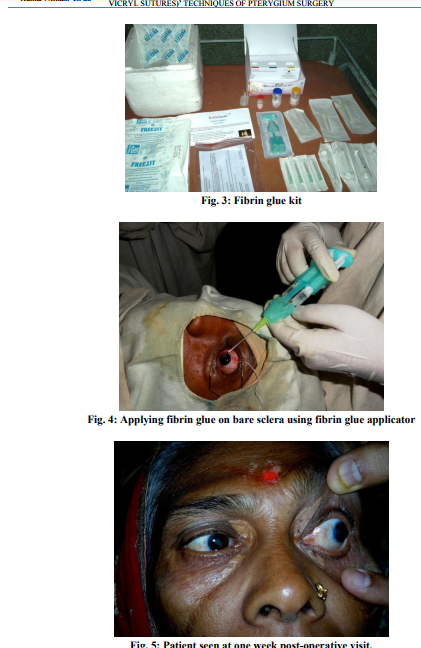
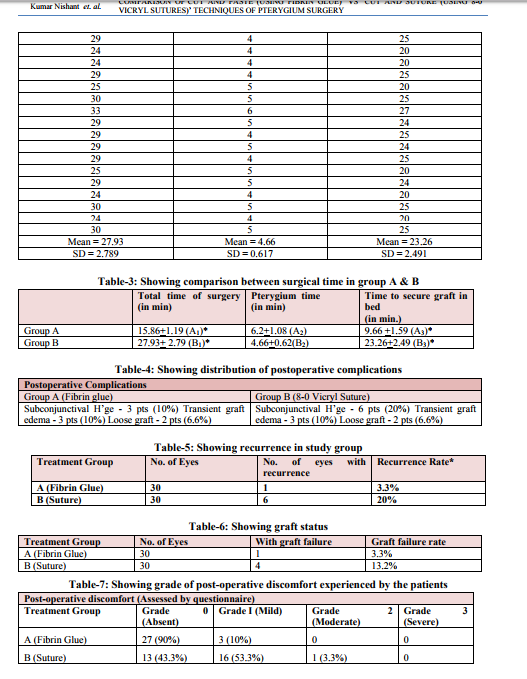
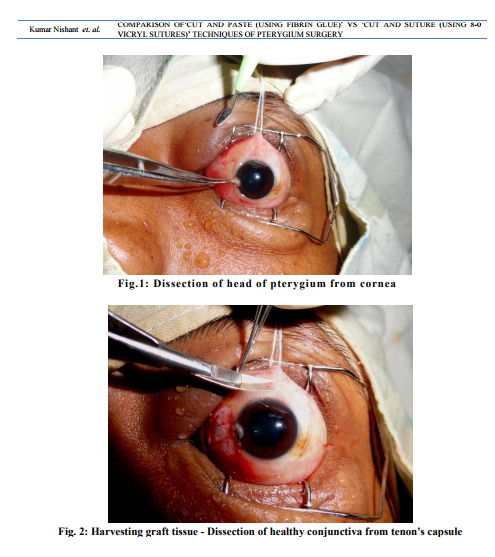
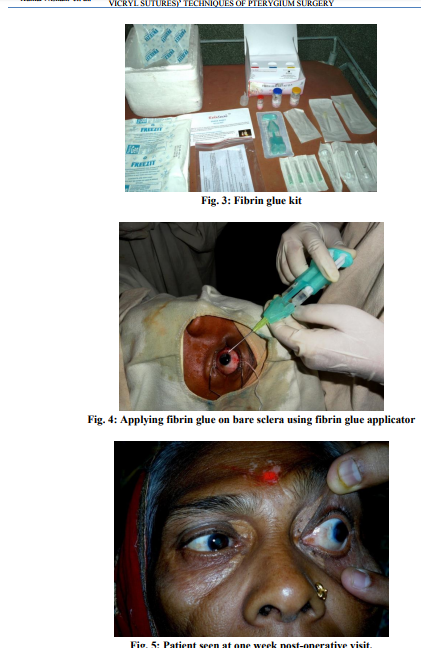
All surgeries were performed by a single experienced surgeon, always using the same equipments, technique and materials in each group except instead of using fibrin glue in Group A; 8-0 Vicryl sutures were used to fix conjunctival autograft on bare sclera in Group B. Surgical Steps: 1. Peribulbar block 2. Dressing and draping 3. Superior rectus bridle suture 4. Dissection of pterygium from apex to periphery 5. Dissection of conjunctival autograft from supero-temporal area 6. Graft secured either by 8-0 Vicryl sutures or by Fibrin Glue Securing the graft in bare sclera bed was done: A. With Sutures Once the graft is secured with the 4 cardinal sutures (8-0 Vicryl Suture) at the 4 corners, the forniceal edge can then be sutured with further interrupted sutures which need not include the episclera. These help fix the graft in position and avoid displacement of the graft, which can occur as the tissue around the sclera beds contracts and retracts in the postoperative period. B. With Fibrin Glue The Fibrin glue kit (RelisealTM, manufactured by Reliance Life Sciences Laboratories, India) contains 2 major components in separate vials: 1) Freeze dried human fibrinogen 2) Freeze dried human thrombin The kit also contains: 1) Aprotinin solution (Bovine) — 3000 and 1500 kallikrein inhibitor units (kiu/ml) in 1ml and 0.5ml units respectively. 2) 1 × 5 ml ampoule of sterile water for injection 3) 4×2ml syringes for reconstitution and application, 4) 4×21G sterile needles for aspiration of the two components; 2×20G blunt application needles. 5) Fibrin glue applicator with two mixing chambers and 1 plunger guide.
Safety and viral inactivation of the product: The product is screened for HIV 1 and 2, Hepatitis B virus, HCV, Parvo virus and HAV. Solvent Detergent Technology is used to inactivate lipid coated viruses. Though, there is a remote possibility of an unknown infectious agents be present in these products.
PHARMACOLOGY
The fibrin adhesion system initiates the last phase of physiological blood coagulation cascade.
The locally applied mixture quickly sets to form a milky white to translucent mass which continues to gain strength within 2 hrs following application. As wound healing progresses, increased fibrinolytic activity is induced by plasmin and decomposition of fibrin to fibrin products is initiated. Proteolytic
degradation of fibrin is inhibited by Aprotinin (A plasmin inhibitor). The graft is excised and placed on the cornea – with the stromal side facing the surgeon and the limbal edge of the graft adjacent to the limbus of the scleral bed. The reconstituted components of fibrin glue are mixed just at the site of application of the recipient surface by specially designed ?Fibrin Glue Applicator‘. The ensuing reaction results in the formation of sticky fibrin, which anchors the graft to the sclera bed. The graft is smoothed into position and the edges are co-apted to bring about a secure adhesion of the graft to the bed and the conjunctival edges. The process of adhesion usually takes about 45 to 60 seconds, which is time enough for the surgical manipulations. The rest of the procedure is as described before. Each 1 ml reconstituted solution was used in 6-8 patients. Postoperative Care
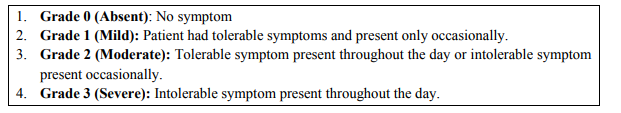
At the conclusion of surgery, 0.5cc dexamethasone and gentamycin is injected subconjunctivally and the eye is firmly patched with antibiotic eye ointment for 24 hours. Starting the next day, topical steroids are used at 2 hourly intervals and then tapered gradually over the next 6 weeks. Antibiotic eye ointment is also used frequently in the postoperative period. Surgical time was noted as follows: 1. Total surgical time from 1st cut of conjunctival to removal of lid speculum 2. Time for excision of pterygium 3. Time to secure graft on the bed (Surgical time was approximated to nearest round figures in minutes.) Post-operatively patients were examined on 1st postoperatively day, after 7 days, one month, three months and six months. On 1st post-operatively day following were observed: Grading of postoperative discomfort(graded on scale 0 to 3 using pretested questionnaires):
 Graft success was defined as an intact graft by 4th week after surgery Graft failure was defined as detachment of graft by 4 th week after surgery. Recurrence was defined as proliferating conjunctival tissue extending across the limbus more than 1 mm onto the cornea within surgical field. Graft status: properly placed or displaced or lost. In subsequent visit following things were assessed. 1. Appearance of the graft (any sign of rejection or misplacement) 2. Any sign of recurrence 3. Patients‘ comfort.
Graft success was defined as an intact graft by 4th week after surgery Graft failure was defined as detachment of graft by 4 th week after surgery. Recurrence was defined as proliferating conjunctival tissue extending across the limbus more than 1 mm onto the cornea within surgical field. Graft status: properly placed or displaced or lost. In subsequent visit following things were assessed. 1. Appearance of the graft (any sign of rejection or misplacement) 2. Any sign of recurrence 3. Patients‘ comfort.
Statistical Analysis
Data analysis has been done as: All data has been summarized as frequency tables and percentages have been worked out. The mean, standard deviation and the standard error of difference have been calculated. Student T-test and Z-test have been applied wherever appropriate to find out the difference between the two groups. Asymptomatic significance (P-value) is calculated for all the variables through these statistical tests. A ?Pvalue‘ of less than 0.05 has been considered significant.
RESULTS
Of the 60 patients enrolled in study, 40 (66.67%) were male and 20 (33.33%) were female. The age distribution of the patients shows that the majority of the patients are between 31-40 years of age. (Table 1) In group A mean total surgical time for excision of pterygium and graft placement was 15.86 minutes with SD 1.187 Mean pterygium excision time was 6.2 minutes and SD 1.082 Mean time to secure graft in bed was 9.66 minutes and SD 1.588 (Table 2) In group B mean total surgical time for excision of pterygium and graft placement was 27.93 minutes with SD = 2.789 Mean pterygium excision time was 4.66 minutes and SD = 0.617 Mean time to secure graft in bed was 23.26 minutes and SD 2.49 (Table 3) Comparing (A1 B1), P value = 0.001 i.e. the total time taken for operation is comparable and highly significant* i.e. notably less in A1. Comparing (A2 B2), P value = 0.24 i.e. it is not significant. Comparing (A3 B3), P value = 0.013 and is significant* i.e. time taken to secure graft to bed is much less than that of sutures. (Table 4) Three patients (10%) in Group A and 6 patients (20%) in Group B developed subconjunctival haemorrhage which resolved completely within 4th postoperative week. Three patients (10%) in each Group A and B developed transient graft edema which gradually resolved upon treatment with topical corticosteroid within 4th post-operative week. Two patients (6.6 %) in each Group A and B had loose graft on 1st post-operative day out of which 1 patient in each group developed graft failure by 4th post-operative week while remaining 1 patient in each group showed spontaneous healing and reattachment. (Table 5) In group A, out of 30 eyes of patients, 1 patient developed recurrence, so recurrence rate in group A is 3.3%
In group B, out of 30 eyes of patients, 6 developed recurrences, and so recurrence rate in group B is 20%. The difference of recurrence rate between two groups A and group B is statistically significant or not was tested by following formula. The standard error of difference is 8.0 where as observed difference (20 – 3.3) was 16.7. The observed difference between the two groups is more than twice the S.E. of difference i.e. 2 X 8 = 16.0. Therefore observed difference between recurrence rates was significant*. (Table 6) Group A showed graft failure rate of 3.3% while group B showed graft failure rate of 13.2. Standard error of difference is 6.99 where as observed difference (13.2 – 3.3) is 9.9 which is less than twice of standard error of difference. (Not statistically significant). (Table 7) In Group A, 27 patients (90%) out of 30 experienced no post-operative discomfort while 3 patients (10%) experienced mild post-operative discomfort (Grade 1, assessed using questionnaires) In group B, 13 patients (43.3%) out of 30 experienced no post-operative discomfort while 16 patients (53.3%) experienced mild (Grade 1) postoperative discomfort. 1 patient (3.3%) experienced moderate severity of discomfort (Grade 2). None of the patients in either group experienced any Grade 3 (severe) post-operative discomfort.
DISCUSSION
The present study was carried out to assess and compare the mean surgical time, post-operative discomfort and recurrences among patients undergoing Pterygium excision and conjunctival autografting using fibrin glue; with Pterygium excision and conjunctival autografting using 8-0 Vicryl sutures. Surgical time - comparison between group A and B In group A (Fibrin glue group); the mean total surgical time for excision of pterygium and graft placement was 15.86 minutes with SD 1.187 in comparison to Group B (8-0 Vicryl Suture) where
it was 27.93 minutes with SD 2.789 (P = 0.001; Highly significant). Mean pterygium excision time in Group A and B were 6.2 minutes (± 1.082 SD) and 4.66 minutes (± 0.617SD) respectively (P = 0.24; Not significant). Mean time to secure graft in bed was 9.66 minutes (± 1.588SD) in Group A and 23.26 minutes (± 2.49 SD) in Group B (P=0.013, Significant) [Table 1 and Table 2] Thus, it is seen that time taken for surgery is definitely less for the fibrin glue group i.e. Group A (Table 3). These findings corroborate with studies performed by Koranyi et al (2003)2 on 43 patients with pterygium. Average time was 9.6minutes for glue and 18.5 min. for sutures (p < 0.001). Jiang J, Yang et al (2008)3 also found that the average operating time was significantly shorter (p < 0.001) in fibrin sealant group as compared to suture group. Bahar I, Weinberger D et al (2007)4 noted average operating time to be 16 minutes (range 14-16 minutes) in the fibrin glue group and 28 minutes in Vicryl suture group. Post-operative complications In this study subconjunctival haemorrhage was found to be more commonly associated with conjunctival autografting using 8-0 Vicryl studies, in contrary to the study by Srinivasan S et al (2009)5 which did not find any significant difference. Increased incidence of subconjunctival haemorrhage in group B may be attributed to greater traumatizing of conjunctiva during suturing process (Table 4). In this study, no other complications were found to be more common in a particular group.
RECURRENCE
The observed difference between the recurrence rates in the 2 groups was statistically significant (Table 5). This may be attributed to better and smooth anatomical approximation of conjunctival autograft on recipient bed on application of fibrin glue. Also, edges may be co-apted to bring a secure adhesion to the bed using fibrin glue promoting early graft epithelialization. Moreovergraft positioning might be easier in case of fibrin glue in contrast to Group B wherein graft may have been inadvertently scrolled up resulting in inversion of surfaces leading to graft failure. There were no new cases of recurrence at 6th month postoperative visit. Thus, all recurrences were observed within 3 months post-operatively. The observation corroborates with the study performed by Farid M, Pimazar JR (2003)6 wherein they found recurrence rate in Tisseel group was 3.7% as compared to 20% in sutured group (P = 0.035). The average time of recurrence was 3.13 months. Hall RC et al (2009)7 also found that at 3 months, there were no recurrences in the glue group and 2 recurrences in the suture group. Karalezli a et al (2008)8 also observed recurrence in 1 case (4%) in the fibrin glue group as compared to 3 eyes (12%) in the suture group (p < 0.05).
Graft status Graft failure was seen 4 times more commonly in suture group than in fibrin glue group. Graft failure rate in Group A was 3.3% while in Group B was 13.2% at 4th week post-pterygium surgery [Table-6]. All cases of graft failure ultimately lead to recurrence of pterygium. The three and six month graft failure rate was unchanged and not significantly different between glue and suture groups. Post-operative discomfort In Group A (Fibrin glue group), 27 patients (90%) out of 30 experienced absolutely no post-operative pain or discomfort while in Group B (Suture group), only 13 patients (43.3%) experienced the same [Table-7]. In Group A, 10 % patients had tolerable symptoms in form of foreign body sensation, watering or itching and were present only occasionally in whole day (graded as mild discomfort) on first post-operative day. None of the patients complained of Grade 2 (moderate) or Grade 3 (severe) discomfort.In Group B, a major fraction of patients (56.6%) experienced some form of ocular post-operative discomfort. 16 patients out of 30 (53.3%) complained of mild discomfort while 1 patient complained of moderate / grade 2 discomfort in the form of persistent watering and foreign body sensation throughout the day which gradually subsided on its own. None of the patient in the group complained of any severe/ grade 3 symptoms. In subsequent visits of the patient at 1 week, 1 month, 3 months and 6 months; none of the patients from either group complained of any ocular discomfort. This study supports the observation made by Karalezli A et al (2008)8 wherein they found the intensity of postoperative pain foreign body sensation irritation and epiphora were significantly lower in the fibrin glue group than in the suture group (p < 0.001) Kim H, Mun H J et al (2008)9 also observed that subjective symptoms disappeared in 23 out of 36 eyes (64%) in one week after surgery and all discomforts subsided within two weeks after surgery in all patients. Bahar I, Weinberger D et al (2007)4 also observed satisfaction to be higher in the fibrin glue group (p < 0.05) than in the suture group. Similar observations were also made by Uy HS, Reyes JM et al (2005)10 .
CONCLUSION
This study shows that pterygium excision with conjunctival autografting using Fibrin Glue reduces the surgical time as compared to securing graft using 8-0 Vicryl Sutures. Also, the post operative discomfort and recurrence rate is significantly less in cases with Fibrin Glue as compared to 8-0 Vicryl Sutures..This may be attributed to biocompatible nature of fibrin glue which avoids complications derived from sutures and diminishes the sensation of a foreign body in the eye following surgery. Thus, patient comfort and satisfaction is significantly higher when fibrin glue is used for
conjunctival autograftingbut the cost of Fibrin Glue makes it an expensive procedure than conjunctival autografting using Vicryl sutures. Another comparative study may be required to study the feasibility of performinga relatively expensive technique (using fibrin glue) when an inexpensive technique using sutures has been in vogue since long especially in a developing country like India. In due course of time, the cost of fibrin glue is likely to come down; making this novelpterygium surgery technique: ?the procedure of choice of the day‘.
ACKNOWLEDGEMENTS
This dissertation would be wholly incomplete if it did not carry a sincere word of thanks to everyone who has helped us during the course of this study. We wish to express my deep andheartful gratitude to our teachers of Upgraded Department of Ophthalmology Darbhanga Medical College and Hospital, Laheriasarai for their enthusiastic support, keen interest, constant encouragement, patient and friendly guidance at every step of this study.. Wealso thank our colleaguesand supportive juniorsand O.T. staffs of the Upgraded Department of Ophthalmology, Darbhanga Medical College and Hospital, Laheriasarai, whose cooperation and encouragement has helped us to complete this study. We must thank Superintendent Dr. Suraj Nayak and Principal Dr. S.N. Sinha, D.M.C.H, Laheriasarai, for their kind permission to carry out this work. Authors acknowledge the immense help received from the scholars whose articles are cited and included in reference of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature of this article has been reviewed and discussed. We would fail in my duty if we do not thank all the subjects who volunteered for the study.Last but not the least; we must thank Mr. Manoj Kumar, New Bihar Press, Laheriasarai, Darbhanga for his invaluable co-operation and typing the manuscript of this thesis.
References:
REFERENCES
1. Anduze AL, Merritt JC. Pterygium: Clinical Classification and management in Virgin Islands. Ann Ophthalmol 1985; 17: 92-5.
2. Arora Ritu, Goel Monika et al. Fibrin glue Vs Vicryl suture in limbo conjunctival autograft in the management of primary pterygium; a prospective comparative study. AIOC, abstracts. 2010; 262-263.
3. Arrfa R C. Pterygium in: Graysons Disease of the cornea. Mosby year book. 1991:342-5
4. Ashaye AO. Refractive astigmatism and pterygium. Afr J Med Sci 1990;19:225-8.
5. Bahar I, Weinberger D, Dan G, Avisar R. Pterygium surgery: fibrin glue versus Vicryl sutures for conjunctival closure. Cornea.2006 Dec;25(10):1168-72.
6. Bahar Irit, Weinberger Dov, Dan D Gaton and Rahamim Avisar. Fibrin glue versus Vicryl Sutures for Primary conjunctival Closure in Pterygium surgery: Long Term Results. Current Eye Research; 2007, Vol 32, no-5, pages 399- 405.
7. Chan SM, Boisjoly H. Advances in the use of adhesives in ophthalmology. Curr Opin Ophthalmol.2004 Aug;15(4):305-10.
8. Cornand G. Le pterygium in; Terrien F Chirurgie de loeil et des annexes. 1921:376-383.
9. D‘Ombrain A. The Surgical Treatment of pterygium. Br J Ophthalmol 1948; 32: 65-71.
10. Dal Pizzol MM, Roggia MF, Kwitko S, Marinho DR, Rymer S.Use of fibrin glue in ocular surgery. Arq Bras Oftalmol.; 2009 May-Jun;72 (3):308-12.
11. De Kaizer RJ, Swart Vain der Bergh. Results of Pterygium Excision with Sr 90 irradiation, lamellar keratoplasty and conjunctival flaps. Doc ophthalmo 1987; 67:33-44.
12. de Wit D, Athanasiadis I, Sharma A, Moore J. Sutureless and glue-free conjunctival autograft in pterygium surgery: a case series. Eye (Lond) : Epub 2010 Jun 4, 2010 Sep; 24(9):1474-7
13. Dushku N, Tyler N, Reid TW. Immunohistochemical evidence that pterygia arise from altered limbal epithelial basal stem cells. Invest Ophthalmol Vis Science 1993; 34: 1013-20.
14. Farell PL, Smith RE. Bacterial corneoscleritis complicating pterygium excision. AJO 1989 May; 107 (50:515-7)
15. Farid M, Pirnazar JR. Pterygium recurrence after excision with conjunctival autograft: a comparison of fibrin tissue adhesive to absorbable suture. 2009 Jan;28(1):43-5.
16. Fernandes M, Sangwan V S, Bansal A K, Gangopadhaya N, Srihar M S, Garg P, Aasuri M K, Nutheti R and Rao G N. Outcome of Pterygium Surgery: Analysis over 14 years Eye (2005); 19, 1182-1190. Doi:10.1038/sj.eye.6701728; published online 29 October 2004.
17. G Koranyi, S Seregard, E D KoppCut and paste: a no suture, small incision approach to pterygium surgery. Br J Ophthalmol 2004;88:911-914.
18. Goran DH, Hollows FC. Pterygium and ultraviolet radiation: a positive correlation. Br J Ophthalmology. 1984; 68:343.
19. Hall RC, Logan AJ, Wells AP. Comparison of fibrin glue with sutures for pterygium excision surgery with conjunctival autografts. Clin Experiment Ophthalmol. 2009 Aug;37(6):584-9.
20. Hilgers JM. Pterygium its incidence, heredity and etiology. Am Journal Ophthalmology 1995; 119:236-37.
21. Hirst LW, Battisttutta D, Green A. Risk Analysis in development of pterygia. Ophthalmology 1992 Jul; 99(7): 1056-61.
22. Jap A, Chan C, Lim L, Tan DT. Conjunctival Rotation autograft for pterygium. Ophthalmology 106: 67-71, 1991.
23. Jiang J, Yang Y, Zhang m, Fu X, Yao K. Comparison of fibrin sealant and sutures for conjunctival autograft fixation in pterygium surgery; one year follow up. 2008; 222(2): 105- 11.
24. Kamel S. Pterygium: Its nature and new line of Treatment. Br J Ophthalmology 1946; 30: 549- 63.
25. Karalezii Kucukerdonmez A, Akova Y A, R Altan, Yaycioglu, Borazan. Fibrin glue versus sutures for conjunctival autografting in Pterygium surgery: A Prospective comparative study. Br J Ophthalmology. 2008; 92 (9):1206- 1210.
26. Kim HH, Mun HJ, Park YJ, Lee KW, Shin JP. Conjunctivolimbal autograft using a fibrin adhesive in pterygium surgery. Korean J Ophthalmol.2008 Sep;22(3):147-54.
27. Kunimoto N, Mori. Studies on Pterygium part IV. Nippon Ganka Gakkai Zasshi Acat Societatis Ophthalmologicae Japonica. 1963; 67:601-7.
28. Lewallen S. A randomized trial of conjunctival autografting for Pterygium in the tropics. Ophthalmology. 1989;96:1612.
29. Lucio Burrato, Robert I Phillips, Guiseppe Carito, Pterygium Surgery. 1st edition, Pub. Slack Inc USA pg 15-18.
30. M Ankur, J Poonam et al. Pterygium excision and limbal conjunctival autograftingAstigmatism and Cosmetism. www.aios.org / proceed09 / paper2009 / EXT / Ext7
31. Maheshwari S. Effect of pterygium excision on pterygium induced astigmatism. Indian J Ophthalmology 2003; 51: 187-8.
32. Marticorena J, Rodriguez-Ares MT, Tourino R, Mera P, Valladares MJ, Martinez-de-la-Casa JM, Benitez-del-Castillo JM. Pterygium surgery: conjunctival autograft using a fibrin adhesive. 2006 Jan : 25(1) : 34-6
33. Neal AJ, Irwin C, Hope-Stone HF. Strontium beta irradiation in the management of pterygium. Clin Onc Coll Rad 1991 Mar; 3(2): 105-109.
34. Ozdama Y, Mutevelli S, Han U, IIei D, Onal B, Karahaya J, Eye Research Institute Ankara Turkey. A comparative study of tissue glue and Vicryl sutures for closing limbal conjunctival autograft and histological evaluation after Pterygium excision. 2008 July; 27(6): 663-7
35. Pinkerton OD, Hokama Y, shigemura LA. Immunological basis for the pathogenesis of Pterygium. Am Journal Ophthalmology 1984; 98: 225-28.
36. Prabhasawat P, Barton K, Burkett G, Tseng SC. Comparison of Conjunctival Autografts, amniotic membrane grafts and primary closure of conjunctival grafts ophthalmology 104; 974- 85, 1997.
37. Rajiv S, Mittla S, Sood AK. Pterygium and dry eye, a clinical correlation. Indian J Ophthalmology. 1991 Jan-Mar: 39(1); 15-6.
38. Sarnicola V, Vannozzi L, Motolese PA. Recurrence rate using fibrin glue-assisted ipsilateral conjunctival autograft in pterygium surgery: 2-year follow-up. Cornea: 2010 Nov; 29(11):1211-4.
39. Sebban A, Hirst L W. Pterygium Recurrence Rate at the Princess Alexandra Hospital. Aust NZ J Ophthalmol 1991; 19: 203-6a.
40. Srinivasan S, Dollin M, McAllum P, Berger Y, Rootman DS, Slomovic AR. Fibrin glue versus sutures for attaching the conjunctival autograft in pterygium surgery: a prospective observer masked clinical trial. Br J Ophthalmol.2009 Feb;93(2):215-8.
41. Uy HS, Reyes JM, Flores JD, Lim-Bon-Siong R. Comparison of fibrin glue and sutures for attaching conjunctival autografts after pterygium excision. Ophthalmology.2005 Apr;112(4):667- 71.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License