IJCRR - 6(10), May, 2014
Pages: 37-44
Print Article
Download XML Download PDF
CASE REPORT OF PATIENT WITH DESMOPLASTIC AMELOBLASTOMA
Author: Gopal Sharma, Reema Rao, Preeti Talreja, Mahesh B Pokle, Resha Sawla, Sameer Zope
Category: Healthcare
Abstract:Aim: Presenting a case of Desmoplasticameloblastoma with an attempt to differentiate it from fibro-osseous lesion and ameloblastoma Case Report: In this paper we present a case report of a 50yr male who patient presented with a painless swelling in the lower left jaw since 1year. Discussion: Desmoplasticameloblastoma (DA) was included in the World Health Organization Classification of Head and Neck Tumors (WHO-2005) as a variant of ameloblastoma with specific clinical, histological and radiological features to differentiate it from other entities. Radiological and Cone beam volumetric imaging (CBVI) was performed which showed a mixed lesion suggestive of fibro-osseous lesion whereas Incisional biopsy was suggestive of DA. Hence we have attempted to differentiate the three lesions to avoid further misdiagnosis. Conclusion: Desmoplasticameloblastoma cannot be differentiated based only on clinical or only radiological features. A proper collaboration between the physician, radiologist and pathologist is necessary for a proper diagnosis.
Keywords: Ameloblastoma, Cone beam volumetric imaging, fibro-osseous lesion.
Full Text:
INTRODUCTION
Ameloblastomas are categorized as benign epithelial odontogenic tumours though malignant forms exist, they represents about 1% of all oral epithelial odontogenic tumours and 11% of all odontogenic tumors.(1) The annual incidence rates per million for ameloblastomas are 1.96, 1.20, 0.18 and 0.44 for black males, black females, white males and white females respectively.(2) Clinically and radiographically ameloblastomas are classified into three main kinds a) Solid or multicystic (conventional) ameloblastoma which is radiographically multilocular b) Unicystic ameloblastoma which is radiographically multilocular (mural ameloblastoma) c) Peripheral ameloblastoma i.e. ameloblastoma present in the soft tissue Histologically, ameloblastoma has been classified as follicular, plexiform, acanthomatous, granular cell, desmoplastic, and basal cell.(3)The age of primary presentation ranges from 17 to 83 years with a mean age of 41.9 years (males: 44.6 years, females: 39.0 years) and a median age of 42.0 years. Though the first case of Desmoplastic Ameloblastoma (DA) was cited in by Eversol in 1984who called it an "ameloblastoma with pronounced desmoplasia” there are very few
INTRODUCTION Ameloblastomas are categorized as benign epithelial odontogenic tumours though malignant forms exist, they represents about 1% of all oral epithelial odontogenic tumours and 11% of all odontogenic tumors.(1) The annual incidence rates per million for ameloblastomas are 1.96, 1.20, 0.18 and 0.44 for black males, black females, white males and white females respectively.(2) Clinically and radiographically ameloblastomas are classified into three main kinds a) Solid or multicystic (conventional) ameloblastoma which is radiographically multilocular b) Unicystic ameloblastoma which is radiographically multilocular (mural ameloblastoma) c) Peripheral ameloblastoma i.e. ameloblastoma present in the soft tissue Histologically, ameloblastoma has been classified as follicular, plexiform, acanthomatous, granular cell, desmoplastic, and basal cell.(3)The age of primary presentation ranges from 17 to 83 years with a mean age of 41.9 years (males: 44.6 years, females: 39.0 years) and a median age of 42.0 years. Though the first case of Desmoplastic Ameloblastoma (DA) was cited in by Eversol in 1984who called it an "ameloblastoma with pronounced desmoplasia” there are very few
reported cases.(4,5) the incidence of DA among ameloblastomas ranges from 0.9% to 12.1% in different races. Though ameloblastoma in general are more common in the posterior region, Desmoplastic ameloblastoma are located anterior to premolar. The incidence were 82.4% of lesion in the maxilla and 54.8% of lesion in mandible were present in the anterior region.(6) It has also been recently included in the World Health Organization’s Classification of Head and Neck Tumors.(7) Radiographically the diagnosis of DA presents a challenge as it is often mistaken for a fibroosseous lesion.(8) Keeping all this in mind the purpose of this paper is to report a case of desmoplastic ameloblastomaand to highlight the differences between ameloblastoma, desmoplastic ameloblastoma and fibro-osseous lesion, thus making the diagnosis of DA simpler.
CASE REPORT
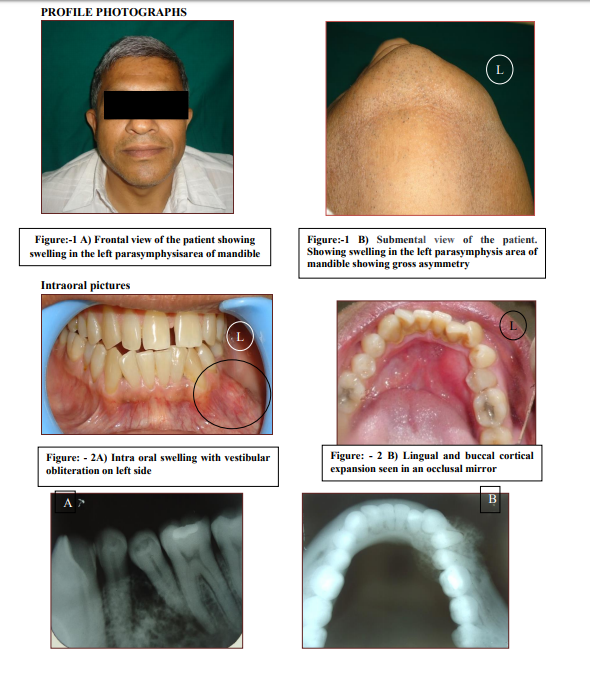
A 50 yrs male patient reported to the department of oral medicine and radiology, YMT Dental College and hospital, Kharghar, Navi Mumbai with a chief complain of swelling in the lower left region of jaw since 1yr. The patient reported that the swelling was smaller in size 1yr back, which increased to its present sizesince the last 3months. There is no associated pain, paresthesia or loss of sensation in the area. The patient’s medical history revealed that he is a diabetic and is on medication (Tab. Gluconol 120mg) since 13 yrs. Extra-orally there is a gross facial asymmetry with an oval swelling in the left parasymphysis region of the jaw (Figure. 1A and 1B) measuring approximately about 3 X 3 cm in size. It extends anteriorly from the symphysis region to 3cm posteriorly over the body of mandible. Superiorly it is extends from line joining the angle of mouth to tragus to 1cm above the inferior border of the mandible. Skin over the region is stretched and there is no change of colour of overlying skin. It is bony hard and nontender on palpation with no
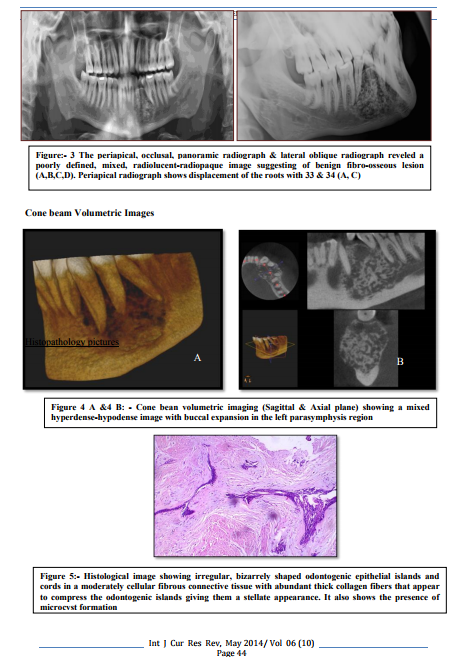
local rise of temperature, patient is afebrile with no cervical lymphadenopathy. Intraorally there is vestibular obliteration extending from the distal aspect of 33 to the distal aspect of 36(Figure. 2A). Cortical expansion seen which is round to oval on both the sides (buccal and lingual) in relation with 33, 34, 35, 36 (Figure. 2B). Maximum expansion was seen with 34 and 35. The mucosa appears of normal colour, textureand consistency. The teeth in relation with swelling i.e. 33, 34, 35, 36 were vital and immobile. There is displacement seen with 34 in mesial direction and 35 in distal direction. The periapical radiograph shows mixed radiolucent and radioopaque image and it shows displacement of the roots with 33, 34 and 35. (Figure 3A) Occlusal radiograph shows cortical expansion equal on buccal and lingual sides teeth displacement is seen over the buccal aspect. (Figure 3B) Panoramic radiograph and lateral oblique radiograph reveled poorly defined, mixed, radiolucent-radiopaque image suggesting of benign fibro-osseous lesion (Figure 3C and 3D). Cone beam volumetric imaging (CBVI) has been performed for the mandibular arch extending from the mandibular left 1st molar to the mandibular right 2nd premolar region to determine the proper extension and for surgical planning of the lesion (Figure 4A and 4B). Section shows a well defined expansile lesion in the body of mandible extending from the left mandibular canine region to the left mandibular 1st molar region. The interior of the lesion appears to be multilocular with multiple granular appearing septae. There is significant expansion of the buccal and lingual cortical plates. The outline of the inferior alveolar nerve canal is not seen clearly within the lesion. The mental foramen is also not traceable. The inferior cortical plate appears to be intact. The mandibular 2nd premolar appears to be displaced (Figure.4A). All these findings suggest a diagnosis of benign tumor in the mandible. With a differential diagnosis of ameloblastoma and odontogenic myxoma is given.
Incisional biopsy was performed and the histopathological evaluation of the specimen (Figure 5A and 5B) shows irregular, bizarrely shaped odontogenic epithelial islands and cords in a moderately cellular fibrous connective tissue with abundant thick collagen fibers that appear to compress the odontogenic islands giving them a stellate appearance. It also shows the presence of microcyst formation. Based on all these findings final diagnosis of Desmoplastic Ameloblastoma (DA) was given. A segmental resection from teeth 33 to 36, maintaining the lower border of the mandible, was performed under general anesthesia.
DISCUSSION
In the WHO classification, desmoplastic ameloblastoma (DA) is considered as a rare variation of ameloblastoma.According to an English literature review carried out by Sun et al.(9) in 2009, there are 115 casesreported of DA. The DA occurs more frequently in the4th and 5th decades of life, and presents nopredilection toward either gender. It affects maxilla and mandible equally, whereas ameloblastoma shows a marked predilection for the mandible in ratio of 5:1(mandible: maxilla). DA shows a marked predilection for anterior (anterior premolar region) region of mandible and maxilla, whereas ameloblastoma is more common in posterior region of the mandible.(10) Clinically, maxillary lesions are more dangerous than mandibular ones as they can invade the adjacent sinus and orbit and involve vital structures. Additionally, the thin maxillary bone is a weak natural barrier for tumors as compared to the thicker mandible.(11) DA differs from the solid/multicystic ameloblastomas, whichare more prevalent in mandibular molar or ramus regions, with variable sizes of swelling; pain tends to be rare, but rootresorption of adjacent teeth is common.(12, 13) Desmoplastic ameloblastoma exhibits a more aggressive behavior than other types of ameloblastoma. This aggressiveness may be due to 1) a potential to
grow to a large size; 2) the common location in the maxilla leading to an early invasion of adjacent structures; 3) the diffuse radiographic appearance, and 4) histological finding of bone invasion. (14) Tooth displacement is a common feature in desmoplastic ameloblastoma in almost 92% of the cases and root resorption is seen in just 33% of the cases.(15) As reported in prior literature, the present case of DA was also found and located in the anterior premolar region of the mandible, presenting as a painless swelling withbuccal expansion and tooth displacement but no root resorption.(16,17,18) Radiographically, desmoplastic ameloblastoma may show either a multilocular, mixed radiolucent/ radioopaque appearance or multifocal appearance of minute flecks of bone similar to that seen in benign fibro osseous lesions. The mixed radiolucent / radioopaque appearance of DA can be attributed to the infiltrative growth pattern of tumour cells into surrounding marrow spaces and simultaneous vigorous osteoblastic activity leading to number of bony flecks.(19) It may also present as a massive expansible osteolytic lesion with honeycomb, mottled or multilocular appearance. According to Philipsen et al, radiographicaly illdefined borders suggest an infiltrative process with propensity to recur.(20) The panoramic radiograph, conventional computed tomography and magnetic resonance images of desmoplastic ameloblastoma are not specific; they are compatible with those of fibro-osseous lesions and can mimic the radiographic appearance of fibrous dysplasia, chronic sclerosing osteomyelitis, and if well-circumscribed, an ossifying fibroma. Therefore, it is necessary to include these in the differential diagnosis. CT scan can delineate the internal structure of the lesion more accurately and is particularly helpful in determining its margins and extension into adjacent structures.(11) MRI shows heterogeneous low to intermediate signal intensity on T1W images, heterogeneous high signal intensity on
Histologically, solid / multicystic ameloblastomas contain two main histopathologic patterns: follicular and plexiform. These patterns consist of proliferating, irregularly shaped islands of the narrow cords of odontogenic epithelium embedded in a connective tissue stroma. By contrast, DA has appeared as irregularly shaped odontogenic epithelial islands surrounded by a narrow zone of loose-structured connective tissue embedded in desmoplastic stroma. (19,20) The tumor cells of desmoplastic ameloblastoma have shown positive immunoreactivities for cytokeratin (CK), CK 8, 13, 19, filaggrin and
ameloblastoma antibodies, retaining the odontogenic epithelial characteristics.(22) The management of solid/multicystic ameloblastomas and DA has been controversial due to the high rate of recurrence, especially in conservative treatments (enucleation and/or curettage).(23) Sun et al.(9) (2009) identified a 15.9% rate of recurrence in DA cases treated by enucleation and/or curettage, with an average recurrence period of 36.9 months. The majority of DA cases reported in the literature have been treated by resection, most likely due to ill-defined borders, thus suggesting an infiltration process and an aggressive biological behavior, which has also been reported by some authors.(24,25) Resection is the most preferred treatment option for desmoplastic ameloblastoma although some cases were treated by enucleation and/or curettage. However curettage leaves islands of tumor within bone, which later manifest as recurrences. Keszler et al.(25) reported a higher recurrence rate (21.4%) for desmoplastic variant than the other types (10.1%) of ameloblastoma. In the present case report, the patient is currently showing no signs of recurrence.
CONCLUSION
Thus, we conclude on the available information that since desmoplastic ameloblastoma shows radiographic appearance resembling fibro osseous lesions, diagnosis is based not only on the clinical and radio graphical appearance but also on the histopathological findings. In spite of the apparent and gross circumscription of the desmoplastic lesion, they have the potential for recurrence because they fail to produce a capsule; it is therefore recommended that DAs should always be treated by complete surgical resection. Further investigation of a larger number of more cases must be carried out in an attempt to predict the behavior and prognosis of this entity.
ACKNOWLEDGEMENT
We acknowledge the immense help received from the scholars whose article are cited and included in references of this manuscript. We are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed
References:
REFERENCES
1. White and Pharoah. Oral radiology, Principle and Interpretation. Fifth edition. New Delhi, Elsevier : 2006
2. Shear M, Singh S. "Age-standardized incidence rates of ameloblastoma and dentigerous cyst on the Witwatersrand, South Africa". Community Dent Oral Epidemiol1978 6 (4): 195–9
3. Kishino M, Murakami S, Fukuda Y, Ishida T. Pathology of the desmoplastic ameloblastoma. J Oral Pathol. 2001; 30: 35-40
4. Eversol LR, Leider AS, Hansen LS. Ameloblastomas with pronounced desmoplasia. J Oral Maxillofac Surg. 1984; 42:735-40.
5. Savitri V, Janardhan M, Suresh R, Kumar RV. Desmoplastic ameloblastoma with osteoplasia: Review of literature with a case report. J Oral Maxillofac Pathol 2013; 17:298-301
6. Sun Z J, WuYR,Cheng N,Zwahlen R A,Zhao Y F. Desmoplastic ameloblastoma – A review, Oral Oncology 45 (2009) 752–759
7. Barnes L, Eveson JW, Reichart PA, Sidransky D. World Health Organization classification of tumors pathology and genetics of tumours of the head and neck. Lyon: IARC; 2005
8. Kawai T, Kishino M, Hiranuma H, Sasai T, Ishida T. A unique case of desmoplastic ameloblastoma of the mandible: report of a case and brief review of the English language literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 87(2):258–63.
9. Sun ZJ, Wu YR, Cheng N, Zwahlen RA, Zhao YF. Desmoplastic ameloblastoma- A review. Oral Oncol. 2009; 45:752-9
10. Beckley ML, Farhood V, Helfend LK, Alijanian A. Desmoplastic ameloblastoma of the mandible: A Case report and review of literature. J Oral Maxillofac 2002; 60:194-8.
11. Rastogi R, Jain H. Case report: desmoplastic ameloblastoma. Head Neck Radiol. 2008; 18: 53-5.
12. Manuel S, Simon D, RajendranR, Naik BR. Desmoplastic ameloblastoma: a case report. J Oral Maxillofac Surg. 2002;60: 1186-8
13. Wakoh M, Harada T, Inoue T. Folliculardesmoplastic hybrid ameloblastoma with radiographic features of concomitant fibro-osseous and solitary cystic lesions.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:774-80.
14. Mintz S, Velez I. Desmoplastic variant of ameloblastoma: report of two cases and review of the literature. J Am Dent Assoc 2002;133:1072-5
15. Shashikanth MC, Neetha MC, Ali IM, Shambulingappa P. Desmoplastic ameloblastoma in the maxilla: a case report and review of literature. Indian J Dent Res 2007;18:214-7
16. Kawai T, Kishino M, Hiranuma H, Sasai T, Ishida T. A unique case of desmoplastic ameloblastoma: report of a case and a brief review of the English language literature. Oral Surg Oral Med Oral Pathol Oral Radio Endod. 1999;87:258-63
17. Durmus E, Kalayci A, Ozturk A, Gunhan O. Desmoplastic ameloblastoma in the mandibleCraniofac Surg. 2003;14:873-5
18. Smullin SE, Faquin W, Susarla SM, Kaban LB. Peripheral desmoplastic ameloblastoma: report of a case and literature review. Oral Surg Oral Med OralPathol Oral Radiol Endod 2008;105:37 40
19. Kishino M, Murakami S, Fukuda Y, Ishida T. Pathology of desmoplastic ameloblastoma. J Oral Pathol Med. 2001; 30:35-40.
20. Philipsen HP, Ormiston IW, Reichart PA. The desmo and osteoplastic ameloblastoma. Histologic variant or clinicopathologic entity? Case reports. Int J Oral Maxillofac Surg 1992; 21:352-7.
21. Minami M, Kaneda T, Yamamoto H, Ozawa K, Itai Y, Ozawa M. Ameloblastoma in the maxillomandibular region: MR imaging. Radiology. 1992; 184: 389-93
22. Kumamoto H, Kamakura S, Ooya K. Desmoplastic ameloblastoma in the mandible: Report of a case with an immunohistochemical study of epithelial cell markers. J Oral Med Pathol. 1998; 3: 45-8.
23. Nakamura N, Higuchi Y, Mitsuyasu T, Sandra F, Ohishi M. Comparison of long-term results between different approaches to ameloblastoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:13-20.
24. Ng KH, Siar CH. Desmoplastic variant of ameloblastoma in Malaysians. Br J Oral Maxillofac Surg. 1993;31:299-30
25. Keszler A, Paparella ML, Dominguez FV. Desmoplastic and non-desmoplastic ameloblastoma: a comparative clinicopathological analysis. Oral Dis. 1996; 2:228–31.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License