IJCRR - 6(10), May, 2014
Pages: 23-27
Print Article
Download XML Download PDF
ASYMPTOMATIC PULMONARY ARTERIOVENOUS MALFORMATION: A CAUSE FOR PERIOPERATIVE HYPOXEMIA IN PREGNANCY WITH BRAIN ABSCESS - A CASE REPORT
Author: Dhanabagyam Govindarajulu, Ganesan C., Periyanarkunan Ramaiya Murugesan, Vinodhadevi Vijayakumar
Category: Healthcare
Abstract:Aim: The importance of clinical history, meticulous clinical examination, perioperative monitoring, team work in diagnosing and treating rare diseases for a better patient outcome. Case report: 26 year old Gravida 2 at term was admitted with sudden onset of severe bifrontal headache, vomiting and diagnosed to have frontal lobe abscess with mass effect. Considering that she was at term, Lower segment caesarean section (LSCS) was done prior to emergency craniotomy for better fetal outcome. Discussion: Due to persistent perioperative hypoxemia, post operatively the possibilities of congenital heart disease and deep vein thrombosis were ruled out. Computerized Tomographic pulmonary angiogram (CTPA) revealed multiple AVMs in left upper lobe and an AVM in the anterior segment of left lower lobe. On reevaluation history and clinical findings clinched the clinical diagnosis of Osler-Weber- Rendu Syndrome (OWR) or Hereditary hemorrhagic telangiectasia (HHT). Fortnight later she underwent surgical excision of PAVMs. Conclusion: This case report highlights the importance of clinical history, meticulous clinical examination, perioperative monitoring and team work in diagnosing rare entities like PAVM, Hereditary hemorrhagic telangiectasia, in a term pregnancy with cerebral abscess.
Keywords: Pulmonary Arteriovenous, Brain Abscess, LSCS
Full Text:
INTRODUCTION
Pulmonary arteriovenous malformation (PAVM) or pulmonary arteriovenous fistula (PAVF) is due to abnormal communications between pulmonary arteries and veins. PAVM is a rare congenital vascular anomaly, associated with Osler-WeberRendu syndrome (OWR) or Hereditary hemorrhagic telengiectasia (HHT). Although PAVMs are rare and therefore likely to be under diagnosed, they are present in 24% of patients with HHT. 1 The natural course of PAVM is not benign. These lesions can be associated with complications, such as hemothorax, hemoptysis, stroke and brain abscess. 2 Clinical manifestations can be subtle and may remain undiagnosed until complications arise in adulthood 3 as in our patient.
CASE REPORT
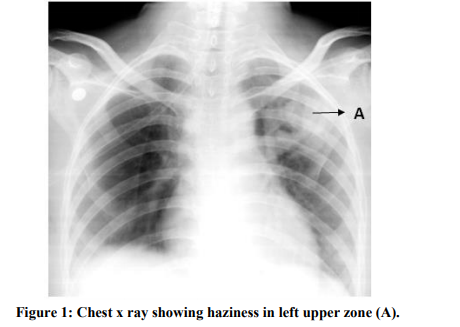
A 26 year old Gravida 2 Para 1 Live 1 at term on regular antenatal followup elsewhere, referred to our hospital with history of severe bifrontal headache and vomiting of sudden onset. There was no history of fever or focal neurological deficits. Her previous pregnancy and parturition was uneventful.On general examination she had grade II clubbing, Glasgow coma scale (GCS) was 15/15 with bilateral pupils size of 3mm reacting to light. Her heart rate was 62/min, blood pressure 130/90mmHg, respiratory rate 20/ minute with SpO? of 90% at room air and 96% with 6 litres of oxygen. On auscultation respiratoy system was clear. Other systemic and spine examination revealed no abnormalities. On abdominal examination uterus corresponded to 37 weeks of gestation with good fetal heart rate.Her blood investigations were normal. Hemoglobin was 14.3 grams/dl. Clinical findings were not suggestive of preeclampsia. Chest X-ray showed haziness in the left upper zone [Figure 1].
Magnetic resonance imaging of brain showed right frontal lobe abscess with mass effect. Clinically, Cardiologist ruled out cardiac abnormalities. Considering that the patient was at term and requiring emergency craniotomy for cerebral abscess evacuation, lower segment caesarean section (LSCS) was planned prior to craniotomy for better fetal outcome. On Preoxygenation with 100% oxygen, SpO2 improved to 96 - 97%. During general anesthesia with controlled ventilation she continued to have low oxygen saturation varying from 92% to 95% with Fraction of inspired O2 (FiO2) of 0.5. LSCS followed by right frontal craniotomy and evacuation of abscess was uneventful. At the end of surgery patient was fully awake, spontaneously breathing with regular respiratory efforts. As patient did not have respiratory distress
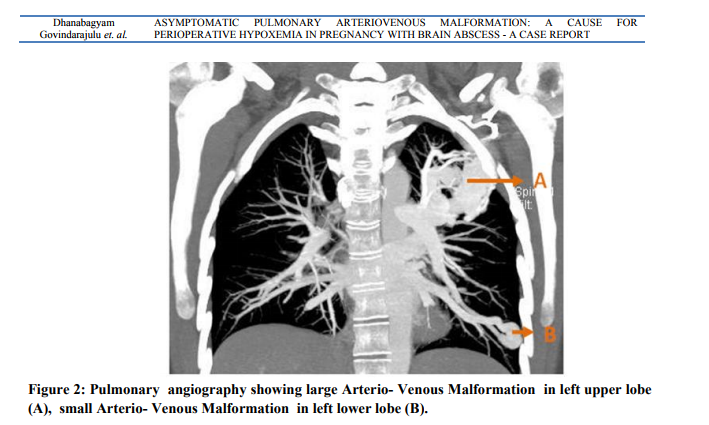
clinically and was maintaining SpO2 of 92-94% with FiO2 of 0.5, she was extubated on table. Postoperatively, repeat chest X ray showed persistent hazinesss in the left upper zone. ABG showed pH 7.395, PaCO2 36.1 mm Hg, PaO2 62 mm Hg, SaO2 91.6%, Lactate 2.6 mmol/lit with FiO2 of 0.6. Transthoracic echocardiography showed mild left atrial and left ventricular dilatation and no pulmonary artery hypertension. In view of persistent hypoxemia, opacities in the chest x ray, mild left atrial and left ventricular dilatation with no pulmonary hypertension and normal lower limb dopplers, Pulmonologist suggested computerized tomographic pulmonary angiogram(CTPA) suspecting PAVM. CTPA revealed multiple AVMs in left upper lobe and an AVM in the anterior segment of left lower lobe[Figure 2].
On reevaluating the patient, there was history of recurrent epistaxis, family history of epistaxis and mild central cyanosis clinched the clinical diagnosis of Osler-Weber- Rendu Syndrome (OWR) or Hereditary hemorrhagic telangiectasia (HHT).
In view of large AVM and non suitability for interventional closure she underwent left lung upper lobectomy [Figure 3] with left lower lobe anterior segmentectomy a fortnight later

 Post operatively her room air SpO2 improved to 99 % and was uneventful. On follow up she had two episodes of seizures and is on anti epileptics. There is no further pulmonary complications.
Post operatively her room air SpO2 improved to 99 % and was uneventful. On follow up she had two episodes of seizures and is on anti epileptics. There is no further pulmonary complications.
DISCUSSION
Osler-Weber-Rendu Syndrome (OWR) or Hereditary hemorrhagic telangiectasia (HHT) is an autosomal dominant disorder characterized by multiple telangiectasia of mucocutaneous tissues and various organs. The four diagnostic criteria for HHT are epistaxis, telangiectasia, visceral lesions and an appropriate family history. The HHT diagnosis is definite if three criteria are present. 4 A plain chest radiograph shows abnormalities in about 98% of patients. 5 A cerebral abscess may be the first manifestation in HHT of an otherwise asymptomatic PAVM. 6 Cerebral abscesses may be due to: 1) hypoxemia decreases resistance of cerebral tissue to infection; 2) arterial thrombosis due to secondary polycythemia causes cerebral ischemia/infarct which is optimal to bacterial growth; and 3) septic embolus through PAVM. 7 Risk of this complication increases during pregnancy because of greater cardiac output and increased level of progesterone that causes relaxation of arteriolar smooth muscle within the PAVM, reducing their resistance and further increasing blood flow through the PAVM. 8 Positive pressure ventilation likely worsens hypoxemia by increasing pulmonary capillary resistance and redistributing blood flow to the AVMs, thereby worsening right-to-left shunting. 9 This explains the cause for post intubation fall in SpO2 from 96 to 92% with FiO2 of 0.5 in our patient. Pulmonary angiography is considered the gold standard in detection of PAVMs. All symptomatic PAVMs and asymptomatic PAVMs larger than two cm, or if feeding arteries are larger than two mm, should be treated with surgery or embolisation because of the risk of paradoxical embolism.5. The purpose of treatment includes prevention of neurological complications, progressive hypoxia and its resultant effects and high output cardiac failure. Surgical resection of a PAVM is an acceptable option in those patients who are not amenable to embolisation. 10 Pulmonary AVM’s might have been the cause for right to left shunt producing mild central cyanosis, clubbing, polycythemia, relative left sided volume overload, failure of normal filtering mechanism of the lungs would have resulted in frontal lobe abscess in our patient. Due to large AVM’s and nonsuitability for interventional procedures she underwent left upper lobectomy with lower lobe anterior segmentectomy.
CONCLUSION
This case report highlights the importance of clinical history, meticulous clinical examination, perioperative monitoring and team work in diagnosing rare entities like Hereditary hemorrhagic telangiectasia, PAVM in a term pregnant patient with cerebral abscess and persistent hypoxemia. The decision making in craniotomy with concurrent LSCS followed by surgical excision of PAVMs resulted in successful materno-fetal outcome. Cerebral abscess in a young patient with asymptomatic persistent hypoxemia, polycythemia and clubbing, do consider PAVM after ruling out cyanotic congenital heart disease.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from Dept of anaesthesiology, neurosurgery and cardiothoracic surgery of PSG Institute of Medical Sciences and Research, Coimbatore.We also acknowledge .the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed
References:
REFERENCES
1. Kjeldsen AD, Oxhoj H, Andersen PE, Green A, Vase P. Prevalence of pulmonary arteriovenous malformations (PAVMs) and occurrence of neurological symptoms in patients with hereditary haemorrhagic telangiectasia (HHT). J Intern Med 2000;248(3):255-62.
2. Dinkel HP, Triller J. Pulmonary arteriovenous malformations: embolotherapy with superselective coaxial catheter placement and filling of venous sac with Guglielmi detachable coils. Radiology 2002;223:709-14.
3. Tse KC, Ooi GC, Wu A, Ho PL, Ip SK, Jim MH, et al. Multiple brain abscesses in a patient with bilateral pulmonary arteriovenous malformations and immunoglobulin deficiency. Postgrad Med J. 2003;79(936):597-9.
4. Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, et al. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-OslerWeber Syndrome). Am J Med Genet. 2000;91(1):66-7.
5. Dines DE, Arms RA, Bernatz PE, Gomes MR. Pulmonary Arteriovenous fistulas. Mayo Clin Proc 1974;49:460-5.
6. Harkonen M. Hereditary hemorrhagic telangiectasia (osler-weber-rendu disease) complicated by pulmonary arteriovenous fistula and brain abscess. Acta Med Scand 1981;209(1-2):137-9.
7. Meacham WF, Scott HW Jr. Congenital pulmonary arteriovenous aneurysm complicated by bacteroides abscess of brain: successful surgical management. Ann Surg 1958;147:404-8.
8. Elliott JA, Rankin RN, Inwood MJ, Milne JK. An arteriovenous malformation in pregnancy: a case report and review of the literature. Am J Obstet Gynecol 1985;152:85-8.
9. Friedman BC1, McGrath BJ, Williams JF. Pulmonary arteriovenous fistula: mechanical ventilation and hypoxemia. Can J Anaesth. 1992;39(9):963-5.
10. Khurshid I, Downie GH. Pulmonary Arteriovenous Malformation. Postgrad Med J 2002;78:191–7.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License