IJCRR - 6(12), June, 2014
Pages: 72-75
Date of Publication: 23-Jun-2014
Print Article
Download XML Download PDF
PLEURAL IMPLANT OF THYMOMA CYTOMORPHOLOGY - A CASE REPORT
Author: Brahmaiah Chari, Vinay H. Shankar, Geetha V. , Chethana S. Babu, Brij Mohan Kumar Singh
Category: Healthcare
Abstract:Though recurrence of thymoma is rare, yet pleural dissemination has been described by few authors. We present a 37 year old patient who was diagnosed as thymoma WHO classification type B3, stage III on Masoaka staging and underwent complete thymectomy. Two years later she presented with recurrent myasthenic symptoms.On evaluation a pleural nodule was identified .CT guided fine needle aspiration suggested a recurrence.Asrecurrence is rare and no definitiveguidelinesregarding therapy; cytological morphology would be of great help in recognizing recurrence. This would also serve to reduce the requirement of thoracoscopic surgery and its related mortality and morbidity.
Keywords: Thymoma , FNAC(Fine needle aspiration cytology), WHO-World health organization, CT- Computed Tomography
Full Text:
INTRODUCTION
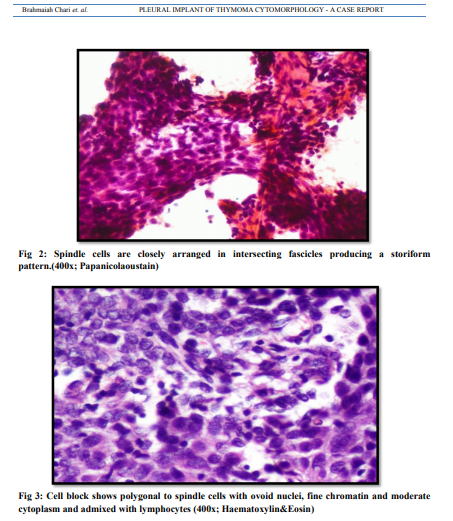
Thymoma is a thymic epithelial neoplasm exhibiting organoid features, accompanied by variable numbers of reactive lymphoid cells.1Cytological diagnosis of thymoma is one of the difficult task encountered in mediastinal lesions,the reason being the rarity of the tumour and the difficulty in getting proper and adequate sampling which is highly dependant on the technical skill of interventional radiologist. Additional characteristic histopathological features that helps in diagnosis of thymoma, such as organotypical differentiation, lobule formation, dilated perivascular spaces can be completely missed in aspiration slides. As there is no standard protocol for the treatment of recurrences, most of the authors in the literature proposed thetreatment that would be multimodal based on evidence based practice.2 Invasive thymoma is characterized by microscopic invasion through fibrous capsule or frank invasion into pericardium, great vessels, and lung. Some thymomasshow multiple implants on pleural and pericardial surfaces.3An invasive thymoma behaves as a malignant tumor despite its benign histologic appearance.A frequent pattern of dissemination of thymoma is by formation of pleural implants.4
CLINICAL FEATURES
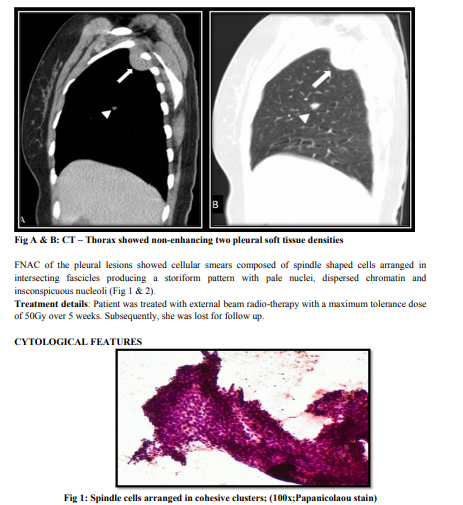
A 37 year old female patient was admitted for evaluation of a chest nodule, detected on regular follow up with CT thorax. Past history was significant for myasthenia gravis and thymoma which was diagnosed 2 years earlier. She had undergone a resection of tumour with histopathological diagnosis as thymoma type B3 according to WHO classification 2004. Systemic examination was within normal limits. Her currentCT scan showed non-enhancing soft tissue density, two pleural lesions. One, measuring 3.6x1.4cms in third intercostal space and another noted along minor fissure 8x16mms(Fig A & B).
DISCUSSION
The distinction between benign and invasive thymoma depends on the demonstration of local invasion or extrathymicmetastasis.2Benign or invasive thymomasshow perivascular space rosette-like formation and gland-like formation seen in contrast to thymic carcinoma.3 Keen and Libshitz6 and Zerhouni et al 5 documented 94% and 91% accuracies of invasion to great vessel and/or pericardium, lung, and pleura on thin-section CT scans.Local invasion by thymomacan involve the chest wall, lower neck, pleura, great vessels and pericardium. They may also spread by pleural seeding.7,8 The reason for the appearance of pleural implants, so called ‘droplet metastases’, after many years of the resection of a non-invasive thymoma is not clear.7The 5-year and 10-year survivals in the series of Verley and Hollmann were 85% and 80% for the group with noninvasive thymomas and dropped to 50% and 35% for the group with invasive thymomas.6,7
CONCLUSION
FNA cytology is a rapid and useful technique in confirming the presence of pleural deposits in a thymoma and cell block when available can be used for IHC studies for confirmation and avoid unnecessary thoracic surgeries and its related morbidity
Conflicts of interest – Ni
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
REFERENCES
1. WahCheuk , John K, C.Chan. Tumors of lymphoreticular system, The Thymus. In:Diagnostic Histopathology of Tumors . Christopher Flitcher (editor); Third Edition.Church Hill Livingstone Elsevier,China: 1315
2. Lucchi M, Mussi A. Surgical treatment of recurrent thymomas. J Thorac Oncol.2010 Oct;5(10 Suppl 4):S348-51
3. Hao-Chun Hung Tan Lee San-Kan LeeDifferential Diagnosis of Invasive Thymoma and Thymic Carcinoma by CT Findings Chin J Radiol 1999; 24(5):179-184.
4. Suster S, Moran CA. Thymoma classification: current status and future trends. Am J ClinPathol. 2006;125:542-554.
5. Zerhouni EA, Scott WW Jr, Baker RR, Wharam MD, Siegelman SS. Invasive thymoma: diagnosis and evaluation by computed tomography. J Comput Assist Tomogr 1991; 15: 429-433.
6. Keen SJ, Libshitz HI. Thymic lesions: experience with computed tomography in 24 patients. Cancer 1987; 59: 1520-1523
7. Verley JM, Hollmann KH. Thymoma: a comparative study of clinical stages, histologic features and survival in 200 cases. Cancer 1985; 55: 1074-1086
8. Marco Lucchi, Fulvio Basolo and Alfredo Mussi Surgical treatment of pleural recurrence from thymomaEuropean J CardiothoracSurg 2008;33:707-711
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License