IJCRR - 6(12), June, 2014
Pages: 64-71
Date of Publication: 23-Jun-2014
Print Article
Download XML Download PDF
AESTHETIC INTERDISCIPLINARY MANAGEMENT OF AGGRESSIVE PERIODONTITIS - A CASE REPORT
Author: Priyanka K. Cholan, P. Ragavi, P. Rajapriya, Mangaiyarkarasi Subramanian
Category: Healthcare
Abstract:Aggressive periodontitis is a type of periodontal disease and is further classified based on their etiology and pathogenesis as: Localized aggressive periodontitis (LAP) and Generalized aggressive periodontitis (GAP). GAP is characterized by generalized interproximal loss of attachmentinvolving at least three permanent teeth other than firstmolars and incisors. This case report describes the periodontal and the aesthetic management of a patient with generalized aggressive periodontitis.
Keywords: Aggressive periodontitis, flap surgery, implants, smile correction
Full Text:
INTRODUCTION
Aggressive periodontitis, as the name implies is a type of periodontitis where there is rapid destruction of periodontal ligament and alveolar bone which occurs in otherwise systemically to healthy individuals of a younger age group but older patients maybe rarely involved in it1,2 . Its etiology is highly correlated due to the presence of Aggregatibacteractionmycetemcomitans3 and host response defects and also possibly related to a genetic inheritance4 .Though there is no widely accepted treatment protocol for Generalised Aggressive periodontitis, this article presents the clinical management of the periodontal and esthetic aspects of a patient with aggressive periodontitis and smile designing for the same. Clinical relevance to interdisciplinary dentistry A multidisciplinary approach to provide improved aesthetics and function. A combinational approach by a team of periodontist, endodontist and prosthodontist helped in the periodontal and esthetic management of a patient with aggressive periodontitis. Management included full mouth flap debridement, implant placement and fixed prosthesis and aesthetic management of protruded teeth and facial profile.
CASE REPORT
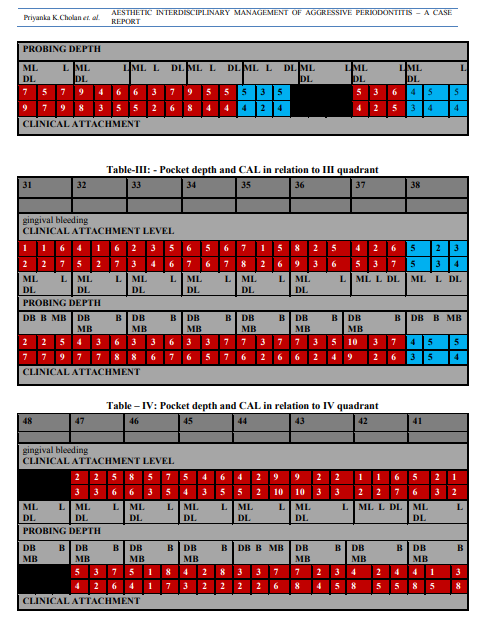
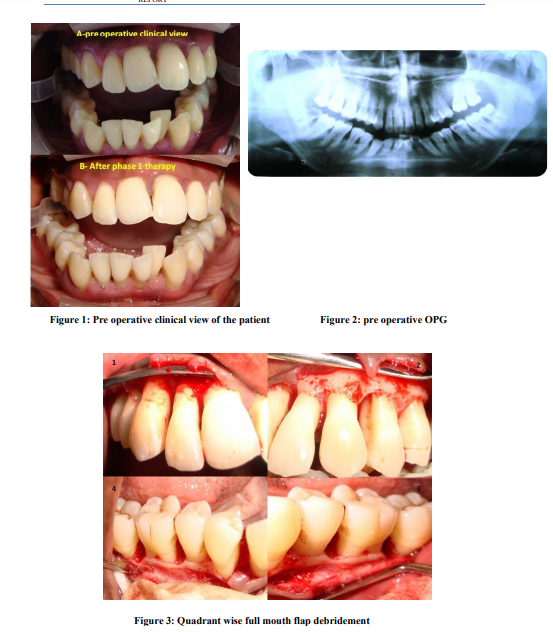
A 24 year old female patient reported to the Department of Periodontics with the chief complaint of forwardly placed teethwith spacing which has increased over the years and bleeding gums for the past 6-7 years. The patient noticed the flaring of anterior teeth few years before, after which she noticed it to be gradually increasing and associated with intermittent episodes of gingival bleeding. There were no related complaints other than a cosmetic concern from the patient. Her medical history appeared non-contributory, as she was not taking any medication, referred no allergies, and had no history of episodic illness or orofacial trauma. Familial history reveals brother with mobile anterior teeth and periodontally compromised dentition. Clinical oral examination, showedgeneralised gingival recessionassociated with deep periodontal pockets as shown in tables I, II, III and IVwith Millers grade I mobility in 11,12,21,22,26,23,24,36,37,38,47 and Millers grade III mobility in 31,41,32 and 42 (Figure 1). The panoramic X-ray (Figure 2) and full mouth IOPAs revealed generalized moderate to severe bone loss which was a combination of both horizontal and vertical bone loss and the severity of bone loss in correlation to the age of the patient suggested a rapid rate of disease progression. The patient was referred for a complete medicalevaluation to rule out any underlying systemic disease. Her complete blood count was within normal limits, including basal glucose and creatinine levels. Absolute monocyte and neutrophil counts were slightly elevated. Due to the age of the patient, familial history, the severity of bone loss, the lack of a detectable systemic disease and rapid rate of disease progression, the diagnosis of Generalized Aggressive Periodontitis was made.Treatment plan was categorized under the following phases including non-surgical phase, surgical phase, restorative phaseand maintenance phase. The major challenges faced in treating this particular case were, compromised periodontal status with advanced attachment and bone loss, gingival recession, unaesthetic gingival display, proclined upper incisors and spacing between the teeth. The treatment options proposed wereorthognathic surgery, orthodontic treatment, rehabilitation with implants and endodontic treatment. The patient was reluctant for orthodontic treatment and orthognathic surgery, due to the prolonged duration of treatment and major surgery associated fear and anxiety. Hence a full mouth periodontal management with extraction of hopeless prognosis teeth and rehabilitation with implants with aesthetic endodontic correction was planned.
CASE DISCUSSION
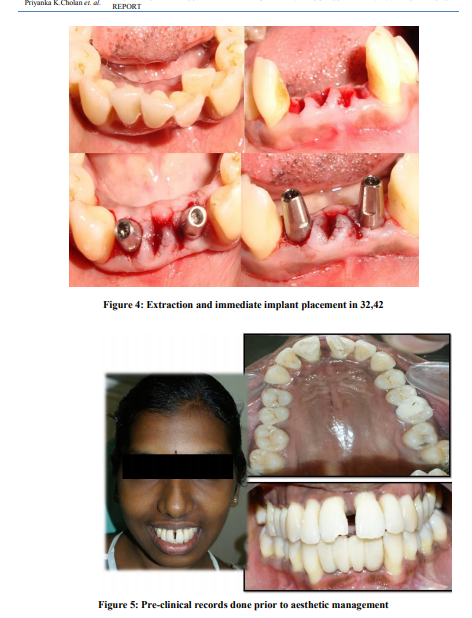
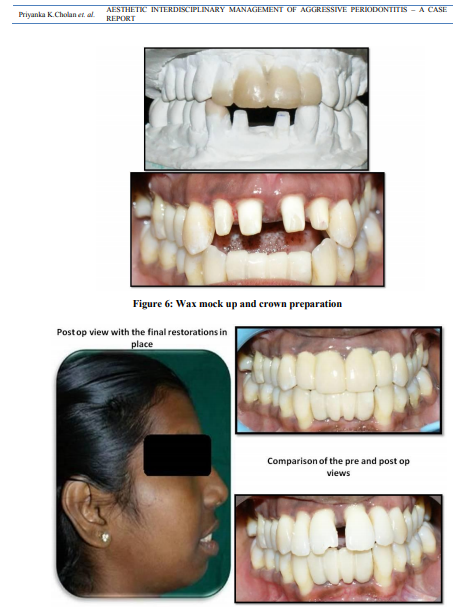
The periodontal management included supragingival and subgingival scalingand root surface debridementand the patient was motivated for better plaque control. Full mouth disinfection with chlorhexidine gelsupplemented with systemic antimicrobial therapy was followed for a period of 8 days. The patient was recalled after 2 weeks for evaluation of the response to treatment5,6 . Persistent high bacterial counts and the presence of periodontal pathogens at surgery adversely affect clinical attachment level gains, meticulous initial therapy and good oral hygiene are considered to be prerequisites for successful periodontal surgery7 . In the surgical phase,a quadrant-wise full mouth flap debridement (Figure 3)was done with bone grafting in relation to upper and lower molar regions. Extraction of hopeless prognosis teeth 31, 32, 41, 42 were done with immediate implant placement. Life care implants 2.8×10 mmwas placed in relation to 32, 42 region (Figure 4)and temporary crowns were given.A postsurgical evaluation done 3 weeks later showed satisfactory healing and probing depths within normal limits. The patient was put on regular recall appointments for evaluation of the gingival and periodontal status and maintenance therapy. Since the patient was concerned about the esthetic appearance of the anterior teeth, she was advised to undergo aesthetic endodontic management. Targets to be achieved in Aesthetic management include: 1. Correction of labial proclination and spacing, which was done stepwise by targeting the required outcome of diastema closure 2. Reduction of theproclined upper incisors 3. Reduction of excessive incisal exposure 4. Rectification of the smile line8 In order to appropriately execute the treatment plan, proper pre-operative photographs were taken
(Figure 5) and awax mock up was done on the study cast (figure 6).9,10Duplication of the wax mock uphelped in both evaluating the possible treatment outcome and aided in providing the patient an understanding of the probable outcome of the treatment. It also helped in obtaining the template to provide proper temporaries during treatment course 9,11. Due to the excessive proclination, the tooth preparation in upper incisors would result in pulpal exposure which indeed led to the intentional root canal treatment for 11, 12, 21 and 22. The tooth preparation was done for full veneer crown in upper incisors 11, 12, 21 and 22 (figure 6). During the tooth preparation the proclination had to be reduced and the incisal height had to be decreased, so the tooth preparation was done more on the labial aspect. The incisal reduction was done excessively to reduce the crown height and the preparation margins were done above DEJ(dentinoenameljunction) inorder to reduce the excessive incisal exposure. The temporaries were given with the help of the available template for the upper incisors, the treatment outcome was evaluated and the high points, mainly canine recountouring was done for 33 and further adjustments were made on the temporaries. Following this an impression was taken with the temporaries which acted as a guide for the final porcelain fused metal crowns. Since the periodontal status was compromised, the full veneer crownsfor 11, 12, 21 and 22 were done as a single unit which acted as a splint supporting the mobile teeth. The permanent crowns were then luted in place with type 2 GIC (figure 7). This case was followed upto two years to evaluate any relapse or further bone resorption is related to rehabilitation of teeth resulted in full satisfaction.
CONCLUSION
Even though the occurrence of aggressive periodontitis is much lower than the chronic Periodontitis, the management ofaggressive periodontitis is more demanding compared to that of chronic periodontitis because of its strong geneticpredisposition as an unmodifiable risk factor. In the present scenario the key to a wholesome management of aggressive periodontitis lies in the early diagnosis of the disease process, rigorous treatment modalities and scrupulous life- long maintenance therapy.

References:
REFERENCES
1. Armitage G C. Development of a classification system for periodontal diseases and conditions.AnnPeriodontol 1999;4:1-6.
2. American Academy of Periodontology, “Parameter on aggressive periodontitis,” Journal of Periodontology, 2000:71(5): 867– 869.
3. Fine DH, Markowitz K, Furgang D, Fairlie K, Ferrandiz J, Nasri C, et al. Aggregatibacteractinomycetemcomitans and its relationship to initiation of localized aggressive periodontitis: longitudinal cohort study of initially healthy adolescents. J ClinMicrobiol 2007;45:3859-69.
4. Kinane DF, Shiba H, Hart TC. The genetic basis of periodontitis. Periodontol 2000 2005;39:91-117.
5. M. G. Jorgensen and J. Slots, “Practical antimicrobial periodontal therapy,” Compendium of Continuing Education inDentistry, 2000;21(2):111–124.
6. Roshna Tand Nandakumar K. Generalized aggressive periodontitis and its treatment options:case reports and review of the literature. Case reports in medicine October 2012, Article ID 535321.
7. Jung M H, Park J W, Suh J Y and Lee J M. Clinical case report on treatment of generalized aggressive periodontitis. J Periodontal Implant Sci 2010;40:249-253.
8. Goldstein RE. Esthetics in Dentistry.Philadelphia, PA: JB Lippincott Co 1976:7.
9. Davis N C. Smile Design. Dent Clin N Am 2007;51:299-318
10. Bhuvaneswaran M. Principles of smile design.J Conserv Dent 2010;13:225-32
11. Harry F. Albers. Tooth - colored restoratives: Principles and Techniques, Ninth edition.
12. Goldstein RE. Esthetics in Dentistry.Philadelphia, PA: JB Lippincott Co 1976:7.
13. Chalifoux PR. Anterior porcelain veneers, three-quarter crowns, and full crowns. Contemporary Esthetics and Restorative Practice. 1998;2(1):52-61.
14. Kinsel R P, Capoferri D.Full crowns in the esthetic zone.Dental Dialogue 2005; Volume 5(4). 15. Abbott SJ. Metal-ceramic restorations. Adv Dent Res. 2003;17:55-60.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License