IJCRR - 6(13), July, 2014
Pages: 64-69
Date of Publication: 12-Jul-2014
Print Article
Download XML Download PDF
HYPERTRIGLYCERIDEMIA IN CHRONIC KIDNEY DISEASE - A CLINICALLY RELEVANT STUDY
Author: Sanjay H. Kalbande, Takkallapalli Anitha
Category: Healthcare
Abstract:Background: Cardiovascular disease is the major cause of mortality and morbidity in patients with chronic kidney disease [CKD] Hypertriglyceridemia may contribute to the progression of atherosclerosis and it is considered to be an independent risk factor for patients of chronic kidney disease. Aim: To study the effects of hypertriglyceridemia, especially in males and females suffering from chronic kidney disease, to comparative evaluation of serum triglyceride levels in patients of chronic kidney disease undergoing hamodialysis and patients on conservative therapy. Methodology: Our study included 100 patients of chronic kidney disease, of which 66 were males and 34 were females. Results: On decade wise grouping, we found maximum number of patients of chronic kidney disease between 51-60 years (42.8%) followed by 61-70 years (40%). The most common cause of chronic kidney disease was found to be type II diabetes mellitus (38%), followed by hypertension (32%) and hypertension 18%. The mean triglyceride levels in both males and females were less than 150 mg/dl in 40% of patients followed by borderline high in 32% and very high in 28% of chronic kidney disease patients. The mean serum triglycerides in patients on conservative therapy was 151.2\?35.31 and in patients undergoing haemodialysis, the mean serum triglycerides was 205.8 \? 69.72. Conclusion: Our study shows that patients of chronic kidney disease have elevated serum triglycerides, in patients on Haemodialysis there is hypertriglyceridemia which could contribute to atherosclerosis and cardiovascular disease.
Keywords: Chronic kidney disease [CKD], Maintenance haemodialysis, [MHD] Serum triglycerides.
Full Text:
INTRODUCTION
Chronic renal failure is the permanent and significant reduction in glomerular filtration rate, or chronic irreversible destruction of kidney tissue [1]. Cardiovascular disease is the leading cause of death in chronic kidney disease patients. Both traditional and non-traditional factors play a role in increased cardiovascular mortality. Among traditional risk factors, diabetes, hypertension and dyslipidemia are the leading causes. Anemia, inflammation, oxidative stress, disorders of calcium and phosphorus metabolism, arterial stiffness and malnutrition can be stated as nontraditional risk factors [2]. Chronic renal failure is often associated with dyslipoproteinemia, high levels of cholesterol and triglycerides, as well as decrease in the polyunsaturated fatty acids. Each of these abnormalities has been identified as an independent risk factor for atherosclerosis [3]. Hypertriglyceridemia is a common phenomenon in chronic renal failure and is associated with endothelial dysfunction. Plasma triglycerides, but not cholesterol, is increased in most patients with advanced renal failure. A high triglyceride concentration predicts coronary heart disease independently from other known factors [4]. Cardiovascular disease begins in the early stages of renal disease. Therefore it is imperative to screen all patients of chronic kidney disease for dyslipidemias and treat them intensively before they develop End stage renal disease.
MATERIALS AND METHODS
The present study was conducted in patients admitted to the department of nephrology, at the chalmeda Anand Rao Institute of Medical Sciences, Bommakal, Karimnagar during the period of 2012-2013. Inclusion Criteria:-Patients of chronic kidney disease, who have previous normal lipid profile. Diagnostic Criteria of chronic kidney disease: 1) Clinical sings and symptoms of Uremia 2) Patients with serum creatinine >1.5 mg/dl 3) Bilateral shrunken kidney / loss of cortico medullary differentiation on ultrasonography of abdomen. Exclusion Criteria:-patients of dyslipidemia due to other causes like hypothyroidism, ethanol, liver disease, known dyslipidemic diabetic patients, HIV patients, patients with genetic disorders were excluded from the study.
METHOD
Informed consent was obtained from all the 100 patients including 66 males and 34 females. All selected patients were subjected to detailed history and complete physical examination. The data collected was noted serially in a predesigned proforma. After 12 hours of fasting, blood samples of patients on conservative therapy as well as patients undergoing haemodialysis were collected and sent for serum triglyceride analysis.
OBSERVATIONS
The following criteria have been taken into consideration for interpretation of the results.
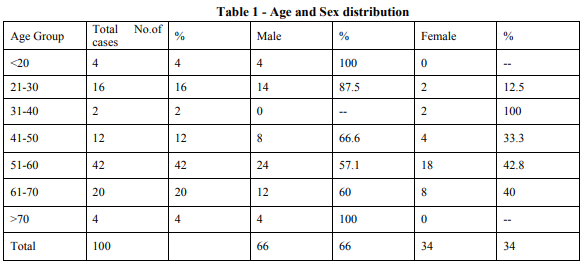
1) Age and sex of chronic kidney disease patients
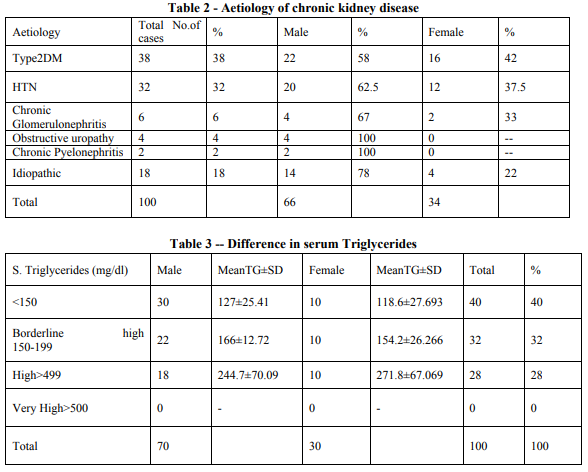
2) Aetiology of chronic kidney disease
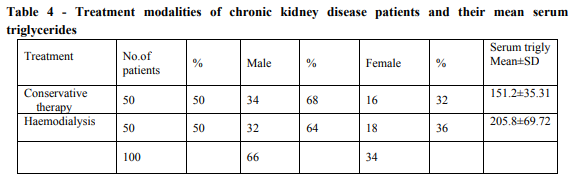
3) Evaluation of serum triglycerides in males and females
4) Treatment modalities of chronic kidney disease patients and estimation of their serum triglycerides.
RESULTS
In our study, 100 patients of chronic kidney disease were included of which 66 were males and 34 were females. On decade wise grouping we found maximum number of patients between 51- 60 years (42%) followed by 61-70 years (20%). The mean age of total number of patients was 51.26. The mean age for male patients was 49.60±16.43 and the mean age for female patients was 4.47±10.26 (table no.1). The most common cause of chronic kidney disease was found to be type II DM [38%] followed by hypertension [32%] (table no.2). The mean triglyceride levels in both males and females were less than 150mg/dl in 40% patients, followed by borderline high in 32% and very high in 28% of chronic kidney disease patients. Mean total triglyceride level was found to be 175.9±57.73. In males it is 170.2±47.85 and females it is 188.35±73.40 (table no.3) The mean serum triglyceride levels in patients undergoing haemodialysis was found to be higher i.e 205.8±69.72 than the patients on conservative therapy i.e 151.2±35.31
DISCUSSION
Patients with chronic kidney disease are at an increased risk of cardiovascular (CVD) disease and have higher prevalence of hyperlipidemia than the general population [5]. The risk of cardiovascular disease varies on the type of lipid abnormalities, the target population, the cause of renal disease and the degree of reduction on glomerular filtration rate [6]. The present study was conducted in 100 chronic kidney disease patients. The mean age of male patients was 49.60 and for females patients was 54.47 years. The overall male to female ratio was 1.94:1. Feast YG et. al. and smith SR [7] analysed age, sex and racial difference, and the incidence of renal disease in american population and found lowest incidence in children(10 years) and highest in the elderly (>40 years). In our study, the maximum numbers of patients is between 51-60 years and males are more commonly affected than females (table no.1). Wing Aj [8] studied causes of chronic kidney disease in different parts of the world and found that geographical variation occurs in different parts of the world. According to United States Renal Data System 1999, the most common cause of chronic kidney disease is Diabetes mellitus (33.2%), followed by hypertension (24%). In the present study, the leading cause of chronic kidney disease was diabetes mellitus (38%) followed by hypertension (32%) [table no.2]. Moreover, the concentration of triglycerides rises with increasing albumin excretion rate in parients with type 1 diabetes. In addition, there is increase in Low Density Lipoprotein mass and atherogenic small dense Low Density Lipoprotein particles, which correlates with the plasma triglyceride concentrations [9]. In the patients of diabetes and hypertension with chronic kidney disease, micro albuminuria is predictive of future proteinuria, progressive decline in renal function, accelerated atherosclerosis and increased cardiovascular mortality [10]. The hypertriglyceridemia is the most common plasma lipid abnormality in patients with renal failure and it is considered as an important risk factor for atherosclerotic vascular disease [11]. Shah et. al. [12] showed that significant hypertriglyceridemia does develop in a majority of chronic kidney disease patients. Anderson et. al. [13] suggested that when lipoprotein pattern in chronic kidney disease was analysed, hypertriglyceridemia was found in 43% of patients. In the present study 60% of patients presented with elevated serum triglycerides [table no.3]. Progressive renal failure, especially that associated with proteinuria, is accompanied by abnormalities of lipoprotein transport. Typically, the dyslipidemia is reflected predominantly in increased serum levels of triglycerides with high levels of very low density lipoprotein, apo B and pre-B high density lipoprotein, and low levels of high density lipoprotein and of apo A [14]. Impaired clearance of chylomicrons and very low density lipoprotein has emerged as the dominant factor for the increased serum triglyceride concentration. Lipoprotein lipase (LPL) is the rate limiting step in lipolysis of chylomicrons and very low density lipoprotein. Lipoprotein lipase binds to heparin sulfate proteoglycans on the cell surface of endothelium. In proteinuric renal diseases a down regulation of Lipoprotein lipase protein abundance and enzymatic activity was found [14]. Experimental data support the notion that triglyceride rich lipoproteins of lower densities are atherogenic and thrombogenic due to abnormal receptor mediated interactions with fibroblasts, macrophages and endothelial cells. It also has been suggested that the increased levels of Lipoprotein (a) in chronic kidney disease patients could represent a risk factor for atherogenesis in these patients. In their study, Cressman et. al. [15] have provided evidence that in haemodialysis patients, elevated Lipoprotein (a) is an independent risk factor for clinical events attributed to coronary artery disease. In our study, the serum triglycerides were found to be significantly higher in Haemodialysis patients as compared to the patients on conservative therapy. Similar hypertriglyceridemia was also observed in several other studies including the CHOICE study [12, 16] Furthermore, Hahn et al [17] have found that dialyzed patients with cardiovascular disease have a 50% increase in the triglyceride levels in comparison with unaffected individuals on dialysis. The recent K/DOQ guidelines on the management of dyslipidaemias suggest the following: 1) For those chronic kidney disease patients with triglycerides ≥200mg/dl and non-high density lipoprotein cholesterol ≥ 130mg/dl, the aim is to achieve non- high density lipoprotein cholesterol < 130 mg/dl. Initial treatment comprises lifestyle changes plus a low-dose statin which is increased as required [18]. 2) In patients with high fasting triglycerides ≥500mg-dl, the initial goal of treatment is to prevent acute pancreatitis. The target is to achieve triglyceride level < 500mg/dl and suggested treatment is with therapeutic lifestyle changes which includes diet, weight reduction, increased physical activity and abstinence from alcohol followed by a fibrate or niacin [18].
CONCLUSION
Patients of dyslipidemias will require lifestyle modification and lipid lowering therapy. All patients with hypertriglyceridemia considered as high risk should be screened and treated accordingly.
ACKNOWLEDGMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to author / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Dewardener, H.E, An outline of normal and abnormal function. In: The kidney 4th edition. Churchill Livingstone New York 1986;181- 235
2. Munter P, He J, Astor BC, Folsom AR, Coresh J. Traditional and non-traditional risk factors predict coronary heart disease:results from atherosclerosis risk in communities study J.Am. soc Nephrol.2005;16[2]:529-38
3. Assman G, Schulte H, Relation of high density lipoprotein cholesterol and triglycerides to incidence of atherosclerotic coronary artery disease (the PROCAM experience). Prospective cardiovascular Munster study. Am J cardio. 1992;70:733-737
4. Castelli;wp. The triglyceride issue: a view from fremingh am, Am Heart J 1986:112:432- 7.
5. Kasiske BL. Hyperlipidemia in patients with chronic renal disease. Am J kidney Dis. 1998;32:S142-S156
6. Weiner DE, Tighiouart H. stark PC, Amin MG, Macleod B, Griffith JL et al. kidney disease as a risk factor for recurrent cardiovascular disease and mortality Am J kidney Dis 2004; 44:198-206.
7. Feast TG and smith SR: Incidence of advance CRF and need for end stage renal replacement. BMJ / 1990;301,897-900
8. Wing AJ: Courses on end stage renal failure Oxford textbook of clinical nephrology. Oxford university press:1227-36:1992
9. Marrie M, Bouhanick B, Berrut G: Micro albuminuria. Curr opin nephrol Hypertens 3; 558-563, 1994
10. Hillege HL, Fidler V, Diercks GF, Van Gilst WH, dezeecw D, van veldhuisen DJ, Gans RO, Janssen WH, Grobbee DE, de Jong PE: Urinary albumin excretion predicts cardiovascular and non cardiovascular mortality in general population. Circulation, 2002; 106: 1777-1782
11. Green D, stone NJ, Krumlowsky A. Putative atherogenic factors in patients with chronic renal failure. Prog cardiovascular Dis. 1983; 26: 133-144 [pub Med]
12. Shah B, Nair S, Sirsat RA, Ashavaid TF, Nair KG, Dyslipidemia in patients with chronic renal failure and in renal transplant patients. J. Post grad Med. 1994;40[2];57-60
13. Anderson AJ : Lipoprotein pattern in chronic renal failure (moyo CLIN proc.1976 oct; 51910); 660-4)
14. Vaziri ND: Molecular mechanisms of lipid disorders in nephrotic syndrome. Kidney Int 63; 1964-1976, 2003
15. Cress man MD, Heyka RJ, Paganini EP, et al Lipoproterin(a) is an independent risk factor for cardio vascular disease in haemodialysis patients. Circulation 1992; 475-82
16. Longenecker JC, coresh J, Powe NR. Traditional cardiovascular disease risk factor on dialysis patients compared with the general population: The CHOICE study.J Am SOC Nephrol 2002; 13(1); 1918-27
17. Hahn R, Oette K, Mondorf H, Finke K, Sieberth HG. Analysis of cardiovascular risk factor in chronic haemodialysis patients with special attention to hyper lipoproteinemias. Atherosclerosis 1983;48: 279-88
18. K/DOQI clinical practice guidelines for management of dyslipidemias in patients with kidney disease. AM J kidney Dis2003;41(4 SUPPL):I-IV,S1-S91.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License