IJCRR - 6(13), July, 2014
Pages: 58-63
Date of Publication: 12-Jul-2014
Print Article
Download XML Download PDF
STUDY OF VISUAL OUTCOME AND POSTOPERATIVE COMPLICATIONS IN SCLERAL FIXATED POSTERIOR CHAMBER INTRAOCULAR LENS IMPLANTATION
Author: Sangeetha T., Narendra P. Datti
Category: Healthcare
Abstract:Purpose: To assess the visual outcome and complications in patients after scleral fixated posterior chamber intraocular lens implantation. Materials and methods: This hospital based prospective study was conducted at R.L. Jalappa Hospital and Research Centre, Tamaka, Kolarbetween November 2011 and May 2013. Study included 50 patients fulfilling inclusion criteria. All cases were worked up according to the protocol.Andall patients underwent mandatory anterior vitrectomy followed by Ab \?externo scleral fixated posterior chamber intraocular lens implantation.10-0 Proline sutures were used for transscleral fixation of lens haptics. Patients were followed up at 1st day, 1st week, 1st month, 3rd month and 6th month. Postoperative evaluation included best corrected visual acuity, Slit lamp Biomicroscopy and Indirect ophthalmoscopic evaluation and Biomicroscopic assessment of macula. Results: Best corrected visual acuity improved in 28 (56%) patients in the range 6/6-6/12 while 18(36%) patients in the range 6/18-6/36. The most common complication observed were striaekeratopathy, iritis and secondary glaucoma; which subsided by two weeks with postoperative medications. Conclusion: Ab\?Externo scleral fixated posterior chamber intraocular lens was found to have stable implantation and a true posterior chamber location in eyes having no capsular or zonular support with a low intra and post-operative risk profile. This technique also showed favourable postoperative visual outcome in aphakic eyes.
Keywords: Aphakia, absence of capsule support, intraocular lens, AC-IOL, PC-IOL, Iris fixation, sclera fixation, secondary intraocular lensimplantation.
Full Text:
INTRODUCTION
Cataract surgery has become the most commonly performed intraocular procedure worldwide, with constantly improving outcomes. Planned extracapsular cataract extraction (ECCE) with posterior chamber intraocular lens (PC-IOL) implantation became more widespread1 and is the “Gold Standard” procedure for managing cataracts. Refinements in surgical techniqueshave givenway to newer techniqueslike manual small incision cataract surgery and phacoemulsification with, inthe-bagPC-IOL implantation which have become the procedure of choice in the management of cataracts.The essential pre-requisite for PCIOLimplantationis the presence of adequate capsulozonular support and ideally the IOL is placed in the capsular bag, which affords stable fixation at a position closest to the nodal point of the eye. However, in the absence of this support it becomes a great challenge for a surgeon, who is faced with manydecisions including when to implant the intraocular lens and which type of intraocular lens should be implanted leaving the patient aphakic. Secondary IOL implantation provides favorable visual outcome offering superior visual rehabilitation in comparison to aphakic spectacles or contact lens, as these lenses have many advantages over both of these techniques.They permit a betterelimination of perceptual problemsand reduceimage size disparity. Hence secondary implantation of intraocular lenses has become the standard procedure in the aphakic eyes. Placing an anterior chamber intraocular lens in aphakics have been discouraged as it carries a high risk of postoperative complications like corneal endothelial damage, pupillary block glaucoma, hyphema, uveitis and cystoid macular edema. Another method where the intraocular lens was sutured to the iris resulted in iris chafing, uveitis and pupillary constriction2 . To avoid these complications and still achieve a posteriorly placed lens position, scleral fixation of posterior chamber intraocular lens to the ciliary sulcus which lies about 1.0mm posterior to limbus3,4, are commonly used which have good visual outcome and less complications.
MATERIALS AND METHODS
A two year prospective study was carried out between November 2011 and May 2013 on 50 aphakic patientsfulfilling the selection criteria after informed consent. All patients were analyzed for visual outcome and intra operative and postoperative complications of Scleral fixated posterior chamber intraocular lens implantation in aphakic eyes using the Modified four point AbExterno scleral fixation technique. Patients with Corneal pathology (degenerations and dystrophies), pathology of retina, macula and optic nerve, chronic uveitis, traumatic cataracts andbleeding disorders were excluded from this study. The patients were divided into following groups according to the nature of procedure required: 1. Primary scleral fixation of IOL. (Patients who had capsular rupture during cataract surgery.Eg: Hyper mature cataracts, pseudoexfoliation, subluxated/dislocated lens) 2. Secondary scleral fixation of IOL. (Patients wanting secondary implantation in aphakic eyes) A complete ocular examination was carried out which included theBest corrected visual acuity with aphakic correction, slit lamp biomicroscopic examination for corneal clarity (endothelial status), presence of synechiae, phacodonesis or frank subluxation / dislocation of lens, pseudoexfoliation in pupillary margins. Dilated evaluation of fundus periphery and biomicroscopic evaluation of macula was done with a+90 D lens, Gonioscopy with Goldmann three mirror for any evidence of PAS, recession or neovascularisation, Applanation tonometry, Keratometery, A-scan and IOL power calculation was done by SRK –2 formula. All patients were given systemic antibiotics (Tab Ciprofloxacin 500mg). On the day of surgery pupils were dilated adequately with 0.8% tropicamideand 5% or 10% phenylephrineeye drops every 10 minutes along with Flurbiprofen eye drops, one hour before surgery. Informed consent was taken and all patients underwent mandatory anterior vitrectomy followed by Ab –externo four point scleral fixated PC-IOL implantation under peribulbar anaesthesia by all operating surgeons. Postoperatively all patients recieved a course of topical antibiotic and steroid eye drops hourly followed by a tapering dose for 6 weeks along with Flurbiprofen eye drops 0.03% TID for 4 weeks. Systemic antibiotics Tab Ciprofloxacin 500 mg was given for 5 days postoperatively. Postoperatively the patient was evaluated on 1st day, 1stweek, 1st, 3rdand 6th month. The total duration of followup was 6 months. At each postoperative visit, the patients were subjected to the following examinations:
1. Best corrected visual acuity for distant and near. 2. Slit lamp evaluation. 3. Indirect ophthalmoscopic evaluation and biomicroscopic assessment of macula was performed. A careful noteof IOL stability and centration, suture relatedcomplications, postoperative reaction and cystoidmacular oedema were made and the compiled pre andpostoperative data analysed. The results were comparedwith previously published studies.
RESULTS
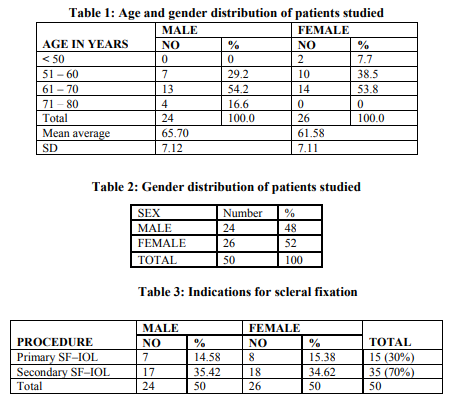
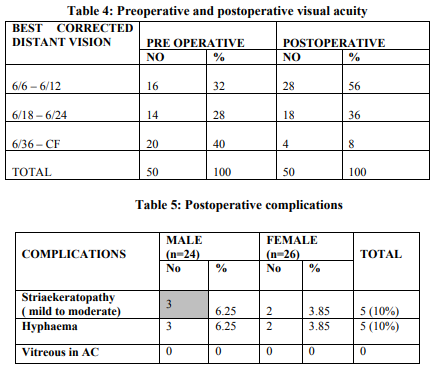
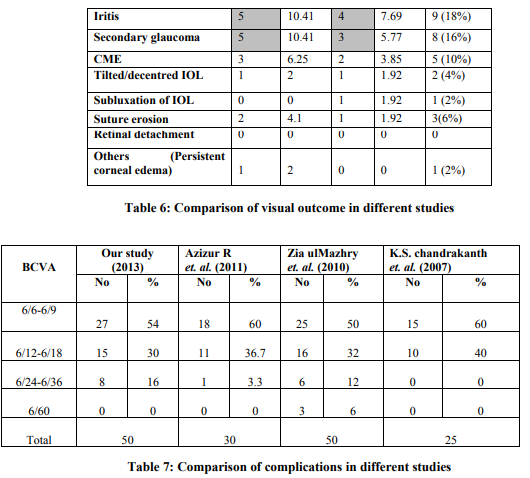
The study included 2(4%) patients in age group <50 years, 17 (34%)patients in the age group 51- 60 years, 27 (54% ) patients in the age group 61- 70 years, and 4 (8%) patients in the age group 71- 80 years. The average age of patients was 63.56 years and about 31 (62%) patients were above 60 years of age.There were 24(48%) males and 26(52%) females. Age and sex distribution is presented in table1. Out of 50 patients 15(30%) patients underwent primary scleral fixation of IOL due to reasons like PC rent, subluxated /dislocated lens, zonular dehiscence etc., and 35 (70%) patients underwent secondary scleral fixation due to postoperative aphakia. Twenty eight eyes (56%) had good vision in the range of 6/6 – 6/12, eighteen eyes (36%) had better vision in the range of 6/18 –6/24 and four (8%) eyes had vision in the range of 6/36 – CF. Postoperative visual acuity improved significantly. (P value = 0.0007) The most common early postoperative complications noticed were Iritis in 9 (18%) eyes followed by Secondary glaucoma in 8 (16%), Striaekeratopathy in 5 (10%) eyesand Hyphaema in 5 (10%) eyes.And the late complications were Cystoid macular edema in 5(10.1%) patients,Suture erosion in 3 (6%) eyes, Mild lens tilt/mild decentered IOL in 2 (4%) eyes, subluxated IOL in 1(2%) patient and persistent corneal edema in 1 (2%) eye. IOL tilt which occurred in 2 cases (4%) developed significant astigmatism in one case only. All the early complications resolved with postoperative medications over a period of 2 weeks. Hyphaema resolved within 3-7 days in all the cases. IOL tilt which occurred in 2 cases (4%) developed significant astigmatism (-1.5 D) in one case only.
DISCUSSION
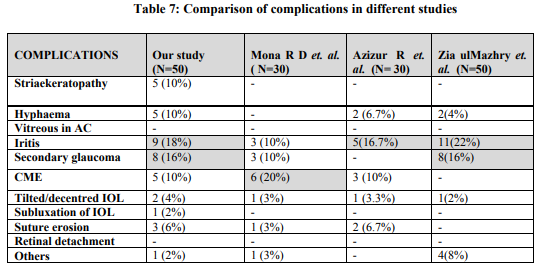
Optical rehabilitation of aphakic patients presents a therapeutic challenge when the patient is unable to tolerate contact lenses for reduction of aniseikonia associated with aphakic glasses. Variable options available include, epikeratophakia, anterior chamber IOL implant, iris fixated intraocular lens and scleral fixated intraocular lens implantation. Among them scleral fixated IOL implant can provide minimum magnification of image as compared to other options.5,6 In this study 50 eyes of 50 patients were included. Twenty eight eyes (56%) had good vision in the range of 6/6 – 6/12. This was comparable with another study conducted by Zia ulMazhry et al (2010)7 in 50 patients. Their study showed BCVA of 6/6-6/9 in 25 (50%) eyes, 6/12-6/18 in 16 (32%) eyes,6/24-6/36 in 6(12%) eyes and 6/60 in 3(6%) eyes.Similarly, K.S. Chandrakanthet al8 and AzizurRahman et al (2011)9 reported improvement of postoperative BCVA of 6/9 in 18 eyes, 6/12 in 6 eyesand 29 eyes in the range 6/6-6/18 respectively. In this study the most common postoperative complication was Iritis in 9 (18%) eyes followed by Secondary glaucoma in 8 (16%), Striaekeratopathy in 5 (10%) eyesand Hyphaema in 5 (10%) eyes.Cystoid macular edema in 5(10%) patients, Suture erosion in 3 (6%) eyes, Mild lens tilt/mild decentered IOL in 2 (4%) eyes, subluxated IOL in 1(2%) patient and persistent corneal edema in 1 (2%) eye which is comparable to Azizur Rahman et. al. (2011) study.
Due to iris manipulation while scleral fixation of IOL we noticed mild iritis in 11 (22%) patients which was comparable with the results of Kwong et. al. and Kanigowska K.10 Our study was also comparable with study conducted by Mona et. al. as depicted in the table 7.
CONCLUSION
We studied the safety, efficacy and stability of scleral fixated PC-IOL with the Ab – Externo four point technique. More than 60% of the cases in our series achieved a postoperative visual acuity of 6/6-6/12. Only 2 of the cases developed IOL tilt which was attributed to lose sutures and slippage. But significant astigmatism was noted only in one case. And one patient had persistent corneal edema even at the end of sixth month follow up probably due secondary glaucoma. Thus we conclude that the Ab – Externo scleral fixated posterior chamber intraocular lens was found to have stableimplantation in eyes with inadequate or no capsular support, with a low intra and post-operative complications. This technique also showed favourable postoperative visual outcome in aphakic eyes.
References:
1. Apple D.J, Mamalis N, Loftfield K.et al. Complications of intraocular lenses. A historical and histopathological review. SurvOphthalmol, 1984; 29:1–54.
2. Evereklioglu C, H, Bekir NA,BorazanM,Zorlu F.Comparison of secondary implantation of flexible open loop anterior chamber and scleral fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 2003; 29 (2):301-8.
3. Duffey R J, Holland, Agapitos P J, Lindstrom R L. Anatomic study of transcleral sutured intraocular lens implantation. Am J Opthalmol.1989; 108:300-9
4. Bergren R L. Four point fixation technique for suturing posterior chamber intraocular lens. Arch Ophthalmol.1994;12:1485-7
5. Bleckmann H, Kaczmarek U. Functional results of posterior chamber intraocular lens implantation with scleral fixation. J Cataract Refract surg. 1994;20:321-6
6. Rahman A, Bhutto I A, Bukhari S, Hassan M, NasirBhatti M. Visual outcome and complications in Ab-externo sclera fixation intraocular lens in aphakia. Pak J Ophthalmol 2011;(27):73-7
7. Zia UM, Wasif MK. Classification and Evaluation of Secondary Posterior Chamber IOL Implantation Scleral Fixation of IOL. Pak J Ophthalmol 2010, 26 (3): 148-153.
8. Chandrakanth K.S, Nirupama B. The functional results of posterior chamber intraocular lens with scleral-fixation: A one-year follow up analysis. 2007;19(4):386-90
9. Azizur R, Israr AB, Sadia B, Mazharul H et al. Visual outcome and complications in AbExterno Scleral Fixation IOL in Aphakia. Pak J Ophthalmol 2011; 27: 73-77.
10. Kanigowska K, Gralek M, Karczmarewicz B. [Transsclerally fixated intraocular artificial lenses in children-analysis of long-term postoperative complications]. KlinOczna.2007; 109:283-6.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License