IJCRR - 6(13), July, 2014
Pages: 45-50
Date of Publication: 12-Jul-2014
Print Article
Download XML Download PDF
WHAT CAN WE MISS IN IDENTIFYING \"MATERNAL NEAR MISS\"EVENT?
Author: Niyati Parmar, Ajay Parmar, V. S. Mazumdar
Category: Healthcare
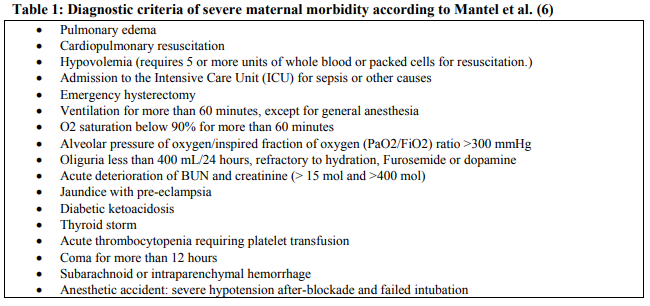
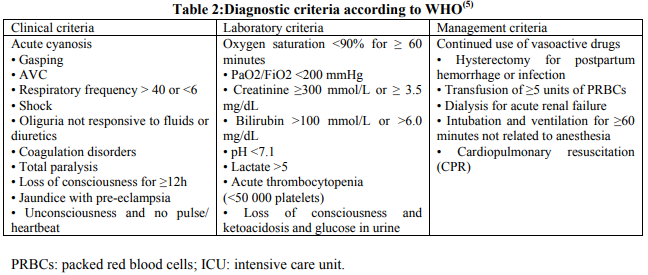
Abstract:Background: The maternal mortality ratio (MMR), the most sensitive indicator for social inequalities, varies dramatically between developed and developing countries. With declining MMR, the need for the search of a new indicator has motivated investigators to study hospital obstetrical morbidity data especially the new concept of severe maternal morbidity called \"Maternal Near Miss (MNM)\" which was defined using WHO and / or Mantel et. al. criteria. Methodology: A hospital based cross sectional study was carried out at tertiary care regional referral hospital where selection of study participants was from the Obstetrics and Gynecology ward irrespective of the place of delivery to improve coverage. Data collection was done over a period of five months by one to one interview of patients after two days of admission to ensure survival after critical condition and then followed up till their discharge. Results: Out of 2238 admissions, 50 women with severe maternal morbidity were identified, of which, 46 women were classified according to WHO and / or Mantel et. al. criteria. While remaining 4 women (~10%) though treated as near miss, did not fit into either WHO or Mantel et. al. criteria and were analyzed separately. Conclusions: Study of factors leading to near miss events which would be factors related to maternal mortality also should be undertaken routinely to identify preventable ones and actions required for the same. Appropriate modifications to the WHO criteria, evolved and validated for local needs, are required as they currently underestimate near misses in India.
Keywords: Maternal near miss, severe maternal morbidity, maternal mortality.
Full Text:
INTRODUCTION
Health Indicators in India are significantly improving. Still maternal mortality and morbidity continue to remain a major public health problem. The maternal mortality ratio (MMR) is the most sensitive indicator for social inequalities. It is considered to be an indicator of economic development and of the quality of obstetrical care. No other health indicator varies so dramatically between developed and developing countries(1) . Maternal mortality is used as a sentinel event to assess the quality of a health care system(2) . Maternal Death Review (MDR) is an important strategy to improve the quality of obstetric care and reduce maternal mortality and morbidity (3) . Studies of negative outcomes have been highly successful in preventing their causes(2). But this strategy of prevention faces difficulties when the numbers of negative outcomes drop to low level. Due to improved health care the ratio has been declining steadily in developed countries(2) . MMR in India has shown an appreciable decline from 212/100,000 live births in the year 2009-10 to 178/100,000 live births as per report of Census India 2010-12 (4) . As there is constant decline in the number of maternal deaths, there is a need for the search of a new indicator. This search has motivated investigators to study hospital obstetrical morbidity data. This idea led to formation of new concept of severe maternal morbidity called “near miss”. The term „„near-miss?? describes a serious adverse event that only failed to occur by luck or by adequate management. This concept was recently defined by the World Health Organization (WHO) as „„a woman who, being close to death, survives a complication that occurred during pregnancy, delivery or up to 42 days after the end of her pregnancy?? (1) . Currently there is paucity of literature available regarding Maternal Near Miss (MNM), as not many studies have been carried out in India; it is a potential area of research. Therefore, a study was carried out to find such events at a tertiary care hospital of central Gujarat. Near Miss women were identified using WHO criteria(5) and Mantel G D et al(6) criteria. Near miss cases occur more often than maternal deaths and theirinquiry is much easier as women survived this condition. Such events start at periphery and end up at higher centre of care. In periphery and rural areas, there is a need to identify high risk women by midwives. When there is presentation of patients with such serious clinical problems, they must be trained to identify these critical conditions or they should be provided with a list of criteria by which they can identify them. With this objective in mind “near miss” cases were attempted to be identified.In the process, some cases were identified who otherwise did not fit into either criteria used for classifying „„near-miss?,? though they should have been classified as Near Miss as they had serious morbidities. The following cases, which though did not fit into the above criteria, were saved only because they were given rigorous and timely medical interventions, and this study presents some of them.
METHODOLOGY
A hospital based cross sectional study was carried out at Department of Obstetrics and Gynaecology at ShriSayajirao General Hospital (SSGH), Vadodara during May to September 2012.It is a tertiary care regional referral hospital having a case load of about 5000 deliveries per year. Selection of study participants was from the ward, irrespective of the place of delivery. Data collection were done by interview after 2 days of admission to ensure survival after critical condition and followed up till their discharge. All the interviews were conducted by the same investigator to avoid inter - observer variation. MNM was defined using WHO(5) and Mantel et al criteria(6). Since both differ in their components it was decided to use both. Over the period of data collection there were some cases which though did not fit into the inclusion criteria did present with clinically serious morbidities and were analyzed separately.
OBJECTIVE
To describe, cases of near miss women, who did not fit into either WHO(5) or Mantel et al criteria(6) defined for classifying “Maternal Near Miss”.
RESULTS AND DISCUSSION
During the entire study period, from May to September 2012, 2238 patients were admitted in Department of Obstetrics and Gynecology. During this time, 18 maternal deaths were reported giving maternal mortality ratio of 933/ 100000 live births for this hospital during the study period. All 2238 cases were followed up for their clinical, laboratory and/or management details to identify the criteria of maternal near miss event if present. 50 women with severe maternal morbidity / near miss were identified, of which, 46 women were classified according to WHO and Mantel et. al. criteria. While, the remaining women though treated as near miss, did not fit into either WHO or Mantel et al. criteria. The number of such women was 4 out of 50, almost 10% of suspected “near miss”. These important set of patients who were missed by both criteria were patients who ideally should have been classified in the category of “near miss” but did not fit into either of the criteria. Their clinical condition was serious enough to be considered as maternal near miss. A brief description of all these cases is as under: Case A A 22 year old primigravida with 31 weeks 6 days pregnancy presented with dry cough, breathlessness and pedal edema. Her blood pressure was 160/100 mm Hg. She had severe pedal and vulval edema. Respiratory system examination showed crepitations and bilateral deceased air entry in basal area. On further investigation she was found to be Rh negative. On ultrasonography (USG) examination Gross free fluid (++++) was present in abdomen. Moderate free fluid was found in left pleural cavity with underlying lung collapsed and mild free fluid was present in right pleural cavity with underlying lung collapsed. Significantly, she had taken 6 Antenatal visits at a private hospital and the last visit was before 25 days of admission to this hospital. At that time, she was diagnosed as having pregnancy induced hypertension (PIH) andUSG was also done. But other problems were not ruled out. After 12 days of admission she delivered a preterm still birth baby by normal delivery. Her total duration of stay at hospital was 17 days. Case B A 28 year old, 4th gravida woman, presented with severe abdominal pain, leaking and bleeding per vaginum. She was referred from one of the Community Health Centres (CHC) due to non availability of doctor at that time and that she needed urgent treatment. As she was in labour, initially assisted vaginal breech delivery was conducted, but it was followed by laparotomy for ruptured uterus due to scar dehiscence of previous caesarean section. She was given 2 PCV (Packed Cell Volume) and 1 RCC (Red Cell Concentrate). When her labour pain started she was alone and finally when it became severe her neighbor took her to hospital in 108 (Ambulance Service). Thetotal time taken between onset of labour pain and reaching 1st referral centre was 12 hours and reaching SSGH was almost 13 hours. This could have been one of the reasons for ruptured uterus. This patient would have died because of ruptured uterus causing haemorrhage, if she had not got timely tertiary care treatment and early transportation by 108. This was one the cases of “near miss”, which was missed by either criterion. Her age at the time of 1st pregnancy was 19 years. Case C A 25 year old woman, 4th gravida, labourer by occupation, presented with severe abdominal pain and bleeding per vaginum at 36 weeks of pregnancy. She came from one of the tribal villages after travelling almost 110 kilometers. Before coming to this hospital she was referred to 2 other hospitals. Within 1 hour onset of labour pain, she was taken to one government hospital in 108(Ambulance Service). The hospital staff waited for 2 hours for progression of labour and gave only pints and some injections. When they felt that labour was not progressing, they referred patient to SSG hospital for further management. Even then, she was taken to some private clinic in government ambulance taking almost 1 hour. The doctor at private clinic examined patient and looking at the severity of condition referred her to SSG hospital within 15 minutes. After another 1 hour of travelling, she was brought to SSGH in unconscious state where immediate laparotomy was done for ruptured uterus delivering still born baby of 3100 grams, which was followed by suturing of uterine rent. She was given blood transfusion in the form of 2 PCV and 1 RCC. She stayed in hospital for 10 days. She took 2 ANC during 3rd trimester at Anganwadi, but no ANC was taken during 1st or 2 nd trimester. On eliciting past history, during previous 3 deliveries she had delivered live babies by normal vaginal delivery which occurred at home. But 2 of them died at the age of 1 year and 1 died at the age of 2 years. So at presentation she did have any living child. Case D A 32 years old farmer, 5th Para, was referred to SSGH from a private hospital post laparotomy for further post-operative management. She was taken to a government hospital in 108 after 2 hours of onset of labour pain. The nurse waited for 12 hours and tried to conduct a normal delivery. During this time she received few injections and pints. Even after waiting for 12 hours when she did not deliver, she was referred to a higher centre in 108. When she was taken to another private clinic after travelling for almost one and half hours, emergency laparotomy was done for ruptured uterus with retroperitoneal hematoma with mild anemia. This whole procedure took almost 2 hours and when critical phase was over she was referred to SSGH for further postoperative management. Two units of blood were given at that private hospital and during transportation On elaborating above cases, Case A was identified as having severe pre-eclampsiawith Rh negativity, severe anasarca and severe vulval edema, with ascites with pleural effusion; still she was not classified by either the criteria as “near miss”. Case B and C were not identified by Mantel and WHO criteria as hysterectomy was not done for ruptured uterus and also, the threshold for severe haemorrhage is transfusion of five or more packed red blood cells. At SSG hospital they received 3 units of blood. In our set up threshold of 5 units may be too high. It may be more appropriate to set it at 1,500 ml (equivalent to three or more packs) or even lower. In both the cases, the women presented in severely morbid conditions, in unconscious state with ruptured uterus, but still did not fit into defined criteria of “near miss”. Case D did not fit into either criteria, but she may have died if she had not got timely treatment at the private hospital at Rajpipla, which is almost 100 km from SSGH, for ruptured uterus before coming to SSGH. When she reached SSGH her critical phase was over. From these incidents we can assume that many more such near miss cases may occur in remote rural areas than those who reach tertiary care centres. But either they would not be reported or may die by the time they would reach such tertiary care centres. Thus, it is necessary to evolve criteria by which such near miss events can be identified earlier at peripheral areas and be referred to higher centers without delay, but only after receiving primary treatment which is necessary for their survival. In the same case at 1st centre nursing staff wasted 12 hours for giving trial of labour. This passage of time with non-progression of labour resulted in rupture of uterus causing formation of retro peritoneal hematoma. As tertiary care centre was almost 130 kilometers away from 1st referral centre, passage of time during transportation may have led to occurrence of maternal death if she had not received treatment at 2nd referral centre.
CONCLUSIONS
Study of factors leading to near miss events which would be factors related to maternal mortality also should be undertaken routinely to identify preventable factors and actions for the same. Appropriate modifications to the WHO criteria, evolved and validated for local needs, are required as they underestimate near misses in India. These criteria can further be implemented by the peripheral health care system to enable early identification of such factors which may, in turn, help prevent some maternal deaths, because of more rapid reporting on maternal care events (because of the larger number of cases).
ETHICAL ISSUES
Before starting enrolment of the participants, necessary clearances and permissions were obtained from concerned authorities and Institutional Ethics committee for Human research (IECHR).
ACKNOWLEDGEMENT
We are highly obliged to all the study participants who enthusiastically participated in the study. We express our honest gratitude to all those who made this study possible including all doctors and hospital staff. We acknowledge immense help received from scholars whose articles are cited and included in references of this article. We are also grateful to authors / editors / publisher of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Fátima Aparecida Lotufo, Mary Angela Parpinelli, Samira Maerrawi Haddad, Fernanda Garanhani Surita, Cecatti JG. Applying the new concept of maternal nearmiss in an intensive care unit. Clinics (Sao Paulo. 2012;67(3):6.
2. Wikipedia tfe. Maternal near miss. Available from: http://en.wikipedia.org/wiki/Maternal_near_m iss.
3. NRHM. Maternal death review. In: Department of Health and Family Welfare GoP, editor.JULY 2010.
4. Office of Registrar General I. A Presentation on Maternal Mortality Levels (2010-12). 20th December 2013.
5. Morse ML, Fonseca SC, Gottgtroy CL, Waldmann CS, E. G. Severe maternal morbidity and near misses in a regional reference hospital. Rev Bras Epidemiol. 2011;14(2):310-22.
6. Mantel GD, Buchmann E, Rees H, Pattinson RC. Severe acute maternal morbidity: a pilot study of a definition for a near-miss. BJOG: An International Journal of Obstetrics and Gynaecology. 1998;105(9):985-90.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License