IJCRR - 6(13), July, 2014
Pages: 38-44
Date of Publication: 12-Jul-2014
Print Article
Download XML Download PDF
MORPHOMETRY OF THE FIRST SACRAL PEDICLE IN SOUTH INDIAN POPULATION
Author: Padmavathi Devi S. V., T. Rajini, Varsha Mokhasi
Category: Healthcare
Abstract:Instrumentation of the sacrum is increasing in importance in treatment of spinal disorders, sacro-iliac joint disturbances and sacral fractures. There is concern about injuries to pedicle cortex, nerve root, facet joint, iliac vein penetration and other vital structures by a misplaced or a misdirected pedicle screw. In this study Description of the Morphometry of the sacral pedicles of Indian samples has been done. 100 dry sacral vertebrae were used for the morphometric analysis of the first sacral pedicle (57 male and 43 female) using vernier calliper (0.1mm) and goniometer. The height of the first sacral pedicle in male was 19.30\?1.6mm and in female was 18.46\?1.8mm. The width of the first sacral pedicle was 24.06\?2.4mm in male and 23.48\?2.3mm in female. The anteromedial trajectory length in male was 46.88\?3.2mm and in female was 43.35\?3.7mm. The anterolateral trajectory length in male was 45.78\?3.5mm and in female was 44.02\?2.2mm. The medial trajectory angle in the male was 34.28\?2.5mm and in female was 32.08\?2.4mm. The lateral trajectory angle in the male was 28.33\?3.4mm and in the female was 25.58\?2.8mm. The results of this study will guide surgeons on the choice of the screws that are used for pedicle fixation and their direction of insertion. A detailed knowledge of the morphometric anatomy of the sacral pedicles will minimize surgical complications.
Keywords: Sacrum, Pedicle, Screw fixation, Sacral pedicle
Full Text:
INTRODUCTION
Pedicle is the cylindrical and strong structure bridging the gap between the dorsal spinal elements and the vertebral body [1]. The nerve roots form the caudal relation to the pedicles as they pass through the inter-vertebral foramina. The nerve roots after passing through the intervertebral foramen are related closely to the lateral border of the immediately caudal pedicle. Due to proximity to the nerve roots, injury to the nerve roots may be possible during procedures involving the pedicle. Pedicle screw fixation involving bone screws to obtain spinal fixation was first described by Tourney in 1943 and King in 1944 and practiced by Boucher in 1959. Over the years pedicle screw fixation systems have proved to be biomechanically superior to segmental fixation. The screws are fixed using linkages which may be rods, plates, internal fixators or have coupling to permit some motion. They may also allow controlling of kyphotic or lordotic forces on the vertebra. They are indicated in spinal instability, post laminectomy spondylolysthesis, painful pseudoarthrosis, spinal stenosis, unstable fractures, stabilizing spinal osteotomies etc.[2] The advantage of the pedicle screw system is that they stabilize dorsal as well as ventral aspects of the spine as they traverse all the three columns of the vertebra.Also the rigidity of the system allows for inclusion of fewer motion segments in order to achieve stabilization. They can be carried out even after a traumatic disruption of the laminae, spinous processes and facets. The main disadvantage is the possibility of neural injury as a result of caudal or medial penetration of the pedicle cortex. Mechanical injury inflicted by a drill ,curette or an eccentrically placed screw or postoperative late screw cut out causing nerve root irritation leading to radiculopathy or cauda equine syndrome. Perforation of the anterior cortex may cause damage to lumbosacral plexus and aorta (at or above Lumbar 4) or iliac vessels. Osteoporosis may prevent adequate screw fixation. The implantation requires extensive tissue dissection to expose points of entry and provide lateral to medial orientation for the screw trajectory. There can be an added risk of infection due to use of many instruments, an image intensifier etc. Pedicle screw systems also involve surgical techniques that bear several potential problems and complications such as postoperative epidural hematoma, overcorrection, and loss of stabilization, pseudoarthrosis and implant prominence. Pedicle fracture may occur due to placing of too large a screw through a small pedicle or due to placing of a screw in an incorrect axis. This reduces the strength of the pedicle and also results in damage to the surrounding structures.[1] The pedicle screw should be ideally placed along the axis of the pedicle incorporating the largest available transverse and sagittal diameters. A thorough understanding of the Morphometry of the first sacral pedicle will help to prevent the damage caused as a result of a misplaced pedicle screw. The purpose of this study is to morphometrically analyse the first sacral pedicle in the Indian population in order to provide surgeons a better understanding of its anatomy so that related complications could be avoided.
MATERIALS AND METHODS
100 dry sacral vertebrae devoid of any visible pathological findings were taken from the Anatomy department of Vydehi Institute of Medical Sciences And Research Centre. Linear parameters were calculated using verniercallipers (0.1mm). Angular parameters were calculated using goniometer.
Linear parameters:
? Pedicle height: line joining a point at the superior most point of the upper margin first sacral foramina and point at the superior border of the sacrum immediately superior to it. ? Pedicle width: the distance between the point at the junction of the first sacral facet and the first sacral body and the point at the junction of the first sacral body and the ala. ? Anteromedial screw trajectory distance: the distance between the midpoint of the sacral promontory to the junction of the first sacral facet and the first sacral body ? Anterolateral screw trajectory distance: the distance between the lateral most tip of the ala of the sacrum to the junction of the first sacral facet and the first sacral body
Angular parameters:
? Anteromedial screw trajectory angle: angle between the line joining the first sacral facet angle to the junction of the body and the sacral promontory and the line joining the first sacral facet angle to the midpoint of the sacral promontory. ? Anterolateral screw trajectory angle: angle between the line joining the first sacral facet angle to the junction of the body and the sacral promontory and the line joining the lateral most tip of the ala of the sacrum to the first sacral facet angle[4]
STATISTICAL METHODS
A t-test for significant difference in means was done at 5% level of significance between the male and female parameters.
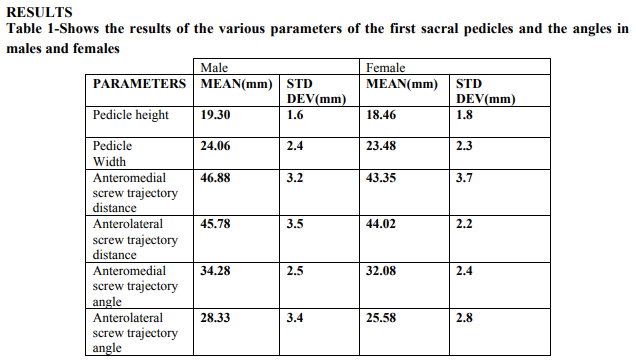
A significant difference in the Pedicle height ,Antero-lateral screw trajectory distance,Anteromedial screw trajectory distance,Antero-medial screw trajectory angle,Antero-lateral screw trajectory angle were found between the male and female sacral vertebra (p0.05).
DISCUSSION
Pedicle screw fixation is a procedure requiring extensive technical expertise and skill. Placing the screw beyond the dimensions of the pedicle, fracturing the pedicle or usage of screws of inadequate circumference, thread size or length has resulted in nerve damage. Any disproportion in the screw diameter or trajectory could hold potential threat to damage of surrounding anatomical structures. The first sacral pedicle has been defined differently in different studies and we find that the differences in measurements of the sacral pedicles can be explained by the differences in the definitions. In this study the distance of entry from a point just inferolateral to the first sacral facet to the midpoint of the sacral promontory was takes as the anteromedial screw trajectory distance and the same point to the lateral most tip of the ala of the sacrum was taken as anterolateral screw trajectory distance. The mean angles for anteromedial and anterolateral orientations were measured. Harrington and Dickenson suggest that sacral screw placements passing through the first sacral pedicle to the sacral promontory were the most secure and thus the anatomical measurement of the first sacral pedicle is of crucial importance.[3] Candan Arman et al. conducted a complete Morphometry of the sacral vertebra in the Turkish population using vernier calliper and goniometer. The results were tabulated in forms of linear and angular parameter. The pedicle height, width anteromedial screw trajectory lengths and angles and the anterolateral screw trajectory lengths and angles were defined similar to our study. However the pedicle height in our study was 4.26 mm more while the anteromedial screw trajectory length was 6.08mm less and the anterolateral screw trajectory length was 5.40mm less than their study. The differences in the measured values in this study and the study conducted by Candan et al. may be accounted for by the diet and socio-economic status of the different populations.[4] Okutan et.al defined the pedicle height between the superior border of the first sacral foramen and superior surface of body of first sacral.The width was between the anterior and posterior width of first sacral pedicle. The measurements were carried out on dry sacra of Turkish population. The pedicle length was the distance from entrance point(X- The tip of the first sacral facet) to promontory. The pedicle height in their study was found to be 5.47mm greater than the values of our study. In our study we have not done a side comparison as no significant differences were encountered between the left and right pedicular morphometric values.[5] Rongming et al. have provided a surgical anatomy of the sacrum. They divide the sacrum into 2 zones, the anatomical parameters of first sacral pedicle in each of the zones were measured and zone 2 was found to be wider and longer than zone 1; and suggest zone 2 is ideal for screw placement. They also suggest that instrumentation extending to second sacral vertebra may enhance the strength of sacral fixation.[7] Ebraheim et.al conducted CT guided anatomical study of the screw paths and lengths. 4 paths were chosen. Path 1 was from lateral border of the superior facet to the anterior cortex of the sacrum at 30 medial inclinations. Path 2 was from the midpoint between the medial and lateral borders of the superior facet to the anterior cortex of the sacral canal. Path 3 was from the medial border to the superior facet to the anterior cortex along the lateral cortex of the sacral canal. Path 4 was from lateral border of the superior facet to the most anterior cortex of the ala. The longest screw lengths were seen with path4. They concluded that the optimum medial screw paths for first sacral are paths 1 and 2. The median distance from the screws inserted this way to the lateral aspect of the sacral canal was 5 to 6mm. Mean length of anteromedial screw was 33 mm and anterolateral screw was 37mm. The current study does not incorporate CT findings.[8] Deepak and Najeeb have provided entry sites and trajectories for thoracic, lumbar and spinal pedicles. They have suggested that the size and angulation of pedicles varies throughout the spinal column. According to their study the transverse pedicle width is said to be narrower than the sagittal pedicle width except in the lower lumbar spine. Pedicles below 10 thoracic vertebra are greater than 7mm in transverse diameter and most below first lumbar are greater than 8mm. The transverse pedicle width increases from first lumbar to first sacral. Coronal angulation decreases along the spine until the lumbar region[1]. According to Mirkovic et.al, using a 30 angulation, the length of the screw was 38 while usage of 45 angulation, the mean length was 44mm[9] . XU et al. reported a mean first sacral pedicle medial angle was 39.4 degrees. Morse et al. using average angles for anteromedial and anterolateral first sacral screw placement defined risks to important structures and advice CT scan verification to determine safe angles to decrease the risk[10]. Peretti et al. notified that the oblique forward and inward degrees of first sacral are 15 and 30 respectively[11] . The current study holds significance as sacral screw fixation surgeries are less common in India. Although morphometric analysis of the sacral pedicle have been carried out many times, an analysis of the Morphometry in the south Indian population will make it simpler for the surgeons to choose the appropriate screw in surgeries performed on this population. The demerits of this study are that it has been carried out on dry sacral specimens and a variation in the in-situ value may be expected. It is also limited to the first sacral pedicle while studies suggest an extension of instrumentation to the second sacral vertebra provides better stability [6] .

CONCLUSION
Development in technology has lead to an increase in the instrumentation at the lumbo sacral level.The knowledge of the pedicular anatomy of the first sacral vertebra has crucial importance in the pedicular-corporeal screw placement.Screw placement will be safe if the screw has proper length and angulation.Larger angles(>34.28mm) may cause damage to the spinal nerves .Smaller angles(<34.28mm) may cause damage to vital vascular structures.It is advisable for dimensions of the screws to be <14.81mm(width) and <51.19 mm(length) to prevent damage to pedicular cortex.
ACKNOWLEDGEMENTS
We would like to thank the institution VIMS & RC for giving us an opportunity for pursuing a research project and forming a strong platform for our future endeavours. We are extremely grateful to all the authors, editors, publishers, books and journals from where literature was reviewed and discussed. We express our gratitude to our family and to the Almighty

References:
1. Deepak Awasthi and Najeeb Thomas, Pedicle, cited at http://www.medschool.lsuhsc.edu/neurosurger y/nervecenter/tlscrew.html Accessed on 14.4.14.
2. Weinstein JN, RydevikBL, Rauschning W. Anatomic and technical considerations of pedicle screw fixation.Clin Orthop Relat Res. 1992 Nov;(284):34-46.
3. Harrington PR, Dickson JH. Spinal Instrumentation in the treatment of severe progressive spondylolistheses. Clin.Orthop,1976(117),157-163
4. Candan Arman , Sait Naderi , Amac Kiray , Funda Tastekin Aksu , Hakan Sinan Y?lmaz , Suleyman Tetik, Esin Korman, The human sacrum and safe approaches for screw placement, Journal of Clinical Neuroscience 16 (2009) 1046–1049
5. Ozerk Okutan, Erkan Kaptanoglu, Ihsan Solaroglu, Etem Beskonakli, Ibrahim Tekdemir, Pedicle morphology of the first sacral vertebra, Neuroanatomy, 2003, Volume 2, Pages 16-19.
6. Xu R, Ebraheim NA, Yeasting RA, et al. Morphometric evaluation of the first sacral vertebra and the projection of its pedicle on the posterior aspect of the sacrum. Spine 1995;20:936–40.
7. Rongming Xu,Nabil A,Ebraheim, MD, and Nicholas K Gove,MD. Surgical anatomy of the sacrum, Am J Orthop. 2008;37(10):E177- E181
8. Ebraheim NA, Xu R, Li J,Yeasting R, Computed Tomographic consideratioms of dorsal screw placement.J Spinal Discord. 1998:11(!):71-74
9. Mirkovic S, Abitbol JJ, Steinman J, et al. Anatomic consideration for sacral screw placement. Spine 1991;16:S289–94.
10. Morse BJ, Ebraheim NA, JacksonT. Preoperative CT determination of angles for screw placement. Spine 1994;19:604-7
11. Peretti F, Argenson C, Bourgeon A, Omar F, Eude P, Aboulker C. Anatomic and experimental basis for the insertion of a screw at the first sacral vertebra. Surg. Radiol. Anat. 1991 (13) 133-137.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License