IJCRR - 6(13), July, 2014
Pages: 31-37
Date of Publication: 12-Jul-2014
Print Article
Download XML Download PDF
CURRENT TRENDS IN ECLAMPSIA AT TERTIARY CARE HOSPITAL
Author: Deliwala K. J., Patel R. V., Shah P. T., Thaker R. V., Patel S. L.
Category: Healthcare
Abstract:Aims and Objectives: (1) To evaluate the incidence of eclampsia (2) To study material and perinatal outcome in eclamptic patients and its management. Methodology: Prospective study was done between July 2007 to June 2012. A total of 308 patients with eclampsia were included in the study. Results: The incidence of eclampsia is about 1.31 %. Majority of patients were primipara and between 21-25 years of age group. 97.1% of patients showed good response to MgSO4 therapy. 53.9 % patients had vaginal delivery while 46.1 % patients had LSCS. Conclusion: Eclampsia is not a totally preventable disease but its incidence can be decreased by proper antenatal care, early diagnosis of Pregnancy Induced Hypertension (PIH) and its proper management.
Full Text:
INTRODUCTION
Eclampsia is defined as new onset of grandmal seizure activity and/or coma during pregnancy, labour or postpartum in a woman with signs or symptoms of preeclampsia, more than 50% occur in third trimester.1 It is one of the leading cause of maternal and perinatal mortality as well as morbidity throughout the world.2,3 Every year more than 50,000 deaths occurred due to eclampsia, most of which occurs in developing countries.4 Recent series reports antepartum eclampsia in 38-53% and postpartum eclampsia in 11-44%.1 Primigravidas are at higher risk of developing eclampsia and that antepartum convulsions are more dangerous than those beginning after delivery.5,6 Incidence of eclampsia is said to be declined, still is a major problem for maternal mortality associated with increased risk of abruptio placenta, disseminated intravascular coagulation (DIC), acute renal failure (ARF), cerebral hemorrhage. It also reduces uteroplacental perfusion, places the foetus at high risk for intra uterine growth retardation (IUGR), preterm birth, and perinatal mortality.6 The main pathology might be generalized vasoconstriction and the endothelial dysfunction and signs and symptoms appear in late mid trimester or in the advanced stage of disease. Mainstay of management in case of eclampsia is early delivery, to improve the prognosis in terms of reducing maternal and perinatal morbidity and mortality. The current study was done to determine the clinical presentation and management of eclampsia, maternal complications and foetal outcome who presented in our institution during the year July 2007 to June 2012.
AIMS AND OBJECTIVES
- To evaluate the incidence of eclampsia in terms of age, parity, socio economic status and gestational age.
- To study mode of delivery, complications, management of eclampsia and perinatal outcome.
- To recognise various factors influencing the prognosis of maternal and foetal outcome.
MATERIAL AND METHODS
Prospective study was conducted at the department of obstetrics and gynaecology in one of the tertiary care teaching hospital. 308 cases of eclampsia patients were taken randomly to study the clinical manifestations, mode of delivery, management and its complications. On admission, assessment of each women was done on an individual basis depending on the severity of condition and the gestational age. Once the patients were stabilized with anti-hypertensive and MgSO4 therapy and detailed history was elicited. Induction of delivery was generally done after 3-4 hours from the last fit. If cervix favourable, induction done with Inj. Oxytocin i.v. infusion drip. If unfavourable, cervix ripened with prostaglandin gel. In case of failed induction cesarean section was done under general anaesthesia.
RESULTS
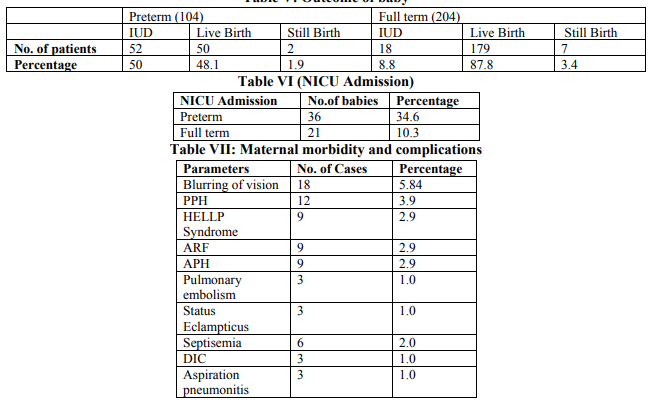
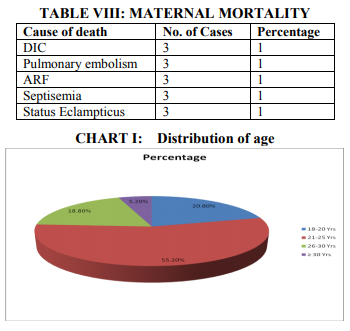
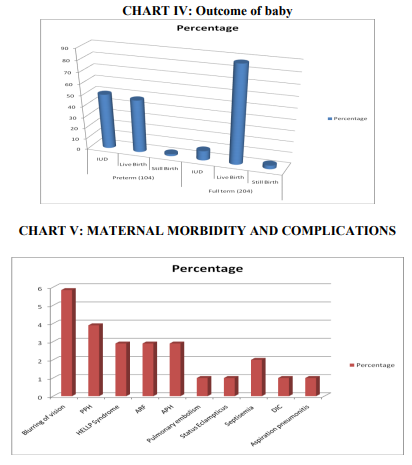
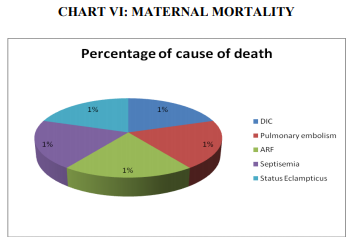
In our study, 308 patients of eclampsia were analysed between the period of July 2007 to June 2012. The incidence of eclampsia is 1.31% in our study.During the present study it is noted that about 80% of patients were emergency while 20% were registered patients. Highest incidence of eclampsia (55.2 %) was seen in the age group of21-25 years (Table Iand Chart I). In our study, almost 74 % of patients were primigravida. About 64.9 % patients had antepartum eclampsia, 15.9 % patients had intrapartum eclampsia while 19.2 % patients had postpartum eclampsia (Table IIand Chart II). Highest incidence of eclampsia was seen between 28-36 weeks of gestation(Table IIIand Chart III) which requires some screening test for prediction of PIH.In our study 88% of patients were having diastolic BP ≥100, 10% of patients had no oedema, 57.8% had +1 oedema and 50% had massive proteinuria. Out of 308 patients, 299 patients (97.1%) showed a good response to MgSO4 therapy (PRITCHARD regime). Only 9 patients (2.9%) required other anti convulsant therapy. Among those 9 patients, 3 had status epilepticus, 3 had two convulsions after MgSO4 therapy and 3 were known case of epilepsy. In patients with atypical eclampsia or prolonged coma, other diagnosis should be considered in women with onset of convulsion more than 48 hours postpartum or in women with focal neurological deficits. In present series, 53.9% of patients had vaginal delivery and 46.1% had cesarean delivery (Table IV). Out of total 308 babies, 9 were stillborn. In 50 live preterm births, 18 babies were expired due to low birth weight and birth asphyxia. Out of 179 live full term babies 9 were expired – 3 due to meconium aspiration and 6 due to birth asphyxia (Table V and VI, and Chart IV). In our study, maternal complication rate was 24.4% while maternal mortality rate was 5% (Table VIIand VIII and Chart V and VI).
DISCUSSION
The hypertensive disorders of pregnancy (HDP) and particularly the pre eclampsia- eclampsia syndrome remain the leading cause of pregnancy related morbidity and mortality worldwide.7 Hypertensive disorders of pregnancy affect almost 7 % of all pregnancies and remain one of the leading causes of adverse maternal and neonatal outcomes, both in developed and developing world. Eclampsia is a major cause of maternal mortality along with hemorrhage and infection.8 This is second most common cause of maternal death during pregnancy.9The incidence of eclampsia is 1.31% in our study while Olakunleet al shows incidence of 1.61%.10The data from public hospitals show a high incidence of eclampsia because all complicated cases from smaller centers, even private clinics are shifted when a patient’s condition deteriorates.11 There is a better understanding of pathophysiology of eclampsia in recent years. It is now generally accepted that eclampsia is a multi-organ disorder unique to human pregnancy. There is generalized vasospasm affecting tissue perfusion in vital organs like brain, liver, kidney, etc. The cause of seizures is attributed to platelet thrombi, hypoxia due to local vasoconstriction or foci of haemorrhage in the cerebral cortex. It must be remembered that though eclampsia often follows severe pre-eclampsia, it can come like a bolt from the blue in a woman without preexisting preeclampsia.11 Eclampsia is more common in women who have not taken antenatal care. In India only 60 % of pregnant women receive antenatal care.11 Good antenatal care will help in prevention of PIH, early detection of PIH and to modify the severity of PIH by giving proper treatment in time. It was suggested that prophylactic use of aspirin, calcium, vitamin C and E may help in preventing PIH and thus may help in preventing eclamptic fit. Aspirin generated a lot of interest as a prophylaxis for PIH. However, recent studies show that its usefulness is to be confirmed by large multicentric trials prophylactic use of aspirin is controversial. Some studies have shown low serum levels of anti-oxidants in women with PIH. Anti-oxidants are known to reduce endothelial cell activation. Eclampsia is a disease specifically of teenage primigravida but highest incidence (55.2%) is seen in age group of 21-25 years in our study. This shift from, teenage to 21-25 years can be explained by late marriages in last few years.12 In our study, almost 74% patients were primigravida which supports the genetic theory of development of preeclampsia where alloimmunity between maternal and foetal tissues is the predisposing factor.13Reynolds suggested the possibility of a single gene likely to be responsible for pregnancy induced hypertension (PIH) which is usually responsible for eclampsia in many cases.14 Eclampsia can recur in future pregnancies in approximately 2% of eclamptics.In our study, about 65% of patients were antepartum. This is because developing countries still are struggling to cope with inadequate ANC, home deliveries and unsupervised deliveries.15In present series, 53.9% patients had vaginal delivery and 46.1 % had cesarean delivery. Umar et al (2007) showed 48.3 % had vaginal delivery and 51.7 % had cesarean delivery.16Vaginal delivery is a safe option resulting in low maternal mortality rates as long as foetal presentation and status are appropriate and labour progresses in an ordinary fashion.17Labour should be closely watched to detect emerging complications like eclampsia, cardiac failure, pulmonary oedema, respiratory failure, cerebrovascular accidents, eye complications, fetal complications like foetal distress/ and death. Neonatologist should be present at birth to look after the newborn. Maternal complication rate was 24.4 % in present series. Rate of complications depends upon number of convulsions, duration of convulsion, duration of admission between hospitalization and last fit, proper nursing care and least time for delivery. Maternal mortality rate was 5 % in our study while Chekari A et al (2008) showed maternal mortality rate of 6.7 %.18Analyzing the causes of death it was found that delayed hospitalization, early onset of eclampsia, low socio-economic status of woman and lack of essential obstetric care are fundamental determinants of maternal death.
CONCLUSION
Eclampsia is not a totally preventable disease but its incidences can be decreased by proper antenatal care, early diagnosis of PIH and pre-eclampsia and its proper management with selective termination to improve maternal and perinatal outcome. This study suggests that MgSO4 therapy is considered as the best therapy and is very effective in preventing and controlling convulsions. Termination of pregnancy is the primary treatment for eclampsia. Induction of labour with oxytocics and prostaglandins decreases the duration of labour. Cesarean section has definite place to improve feto-maternal prognosis. Incidence of complications in LSCS has become very low due to better operative techniques, proper anaesthesia and easy availability of blood components. If vaginal delivery fails following induction of labour cesarean section is preferred.
ACKNOWLEDGEMENT
We acknowledge the immense help received from the scholars whose articles are cited and included in references of our manuscript. We also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. We are also thankful to our seniors, colleagues and patients to help us in our study. Not only that we are also thankful to our family for their kind cooperation and support.
References:
1. Sibai BM. Diagnosis, prevention and management of eclampsia. ObstGynecol; 2005; Feb; 105 (2).
2. Dare FO, Eniola OA, Bariweni AC. Eclampsia revisited. Nig. J Med; 1998; 7; 168-171 cs.
3. Adetoro OO. The pattern of eclampsia at the university of Ilorin teaching hospital, Ilorin Nieria, International J of gynecology and Obstetrics; 31: 221-226.
4. Duley L Maternal Mortality associated with hypertensive disorders of pregnancy in Africa, Asia,Latin America and Caribbean. Br. J. ObstetGynecol 1992; 99: 547-553.
5. Percy CN In: Handbook of Obstetric Medicine Isis Medical Media oxford 1997.
6. Chelsey LC. A short history of eclampsia, ObstetGynecol 1974; 43: 599-602.
7. Acharya p, Damania K.R., Konar H., Misra S., Singh A., Thanawala U., et al.; Pregnancy induced hypertension; In Duftary S.; ECAB clinical update: Obstretricsand Gynecology; High-Risk Labour and Delivery; Haryana; Elsevier; 2011; 42-44.
8. PatilMithil M. et al – Role of Neuro imaging in patients with Atypical Eclampsia – The Journal of Obstetrics and Gynecology of India ( September – October 2012 ) 62 (5) : 526- 530.
9. D’Souza R., Bhide A.; Hypertensive disorders of pregnanacy; In: Thanawala U, Divakear H.; ECAB clinical update: Obstretricsand Gynecology; Medical disorders in pregnancy; New Delhi; Elsevier; 2009; 1-37.
10. Olakunle Kusemiju MBBS : The internet journal of third world medicine, 2008, Volume 6 number.
11. Bhatt R., Patel V., Patel C.; EclampsiaDiagnosis and management; In Mittal C., Mittal P., Emergencies in Obstetrics and Gynecology; Volume I, Second edition; Delhi; Peepee; 2012; 95-101.
12. Wang Y, Gu Y, Zhag Y et al. Evidence of endothelial dysfunction in pre-eclampsia. Decreased endothelial nitric oxide synthatase expression is associated with increased cell permeability in endothelial cells from preeclampsia. Am. J. Obstet. Gynecol, 2004; 190: 817.
13. Kanki T, Mihara F, Nakanoh. Diffusion weighted images and vasogenicoedema in pregnancy. ObsteGynecol. 1999; 93: 821-3.
14. Reynolds C., Mabie W. Hypertension studies in pregnancy; In Current Obst. Gynec. Decheney A.; Ninth Edition; Lange Medical Books, New York; 2000; 338.
15. Naidu K, Modly J. SPECT, CT scan, and TCD findings in eclampsia. Br. J. ObstetGynecol. 1997; 104 (10) : 1162-72.
16. J. Tukur B. A. Umar, R. Rabi U. Annals of African Medicine volume 6, No. 4; 2007: 164- 167.
17. Pritchard J. A. Cunningham FG, Pritchard SA the Parkland Memorial Hospital, protocol for treatment of eclampsia. Evaluation of 245 cases Am. J. Obstet. Gynecol 148: 951, 1984.
18. MigullM;Chekairi, A. Hypertension in pregnancy, 27(2), May 2008.


|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License