IJCRR - 6(13), July, 2014
Pages: 24-30
Date of Publication: 12-Jul-2014
Print Article
Download XML Download PDF
EFFECT OF ENDOTRACHEAL TUBE CUFF INFLATION AND HEAD POSITION ON THE SUCCESS OF BLIND NASOTRACHEAL INTUBATION
Author: Shubhada R. Deshmukh, Charuta P. Gadkari, Gunjan M. Badwaik, Anjali R. Bhure
Category: Healthcare
Abstract:Objectives: The study was conducted to assess the effect of endotracheal tube cuff inflation and position of the head on the success of blind nasal intubation. Method: In a hospital based cross-sectional study, 52 ASA Iand II patients were included. After induction of general anaesthesia, blind nasotracheal (BNTI) intubation was tried with patients on spontaneous ventilation in following sequence of head position and state of endotracheal tube cuff \? Head on bed+cuff deflated (HBCD); Head on bed+cuff inflated (HBCI); Head on pillow+cuff deflated (HPCD); Head on pillow+cuff inflated (HPCI). Once intubation was successful in any one of these positions, the remaining positions were not tried. If blind nasal intubation failed, laryngoscopy was done and patient intubated. Results: Out of 52 patients, 1 of the 4 positions was successful for blind nasotracheal intubation in 47 cases (90.38%). BNTI was successful in 3(6.38%), 17(34.69%), 1(3.13%), 25(83.87%) in HBCD, HBCI, HPCD and HPCI positions respectively. The remaining 5 cases (9.62%) required laryngoscopy for intubation. Success of BNTI was significantly more with the tracheal tube cuff inflated whether head was on table (z score 3.265, P=0.0015) or head was on pillow (z score 4.89, P=0.000006). BNTI was also more successful with the head on pillow as compared to head on bed (z score 2.73, p< 0.006). Complications seen were sore throat in 22 patients, epistaxis in 1 patient and stidor after extubation in 1 patient. Conclusion: We conclude that endotracheal tube cuff inflation as well as raising the head on pillow is efficacious in aiding BNTI.
Keywords: Blind nasal intubation, cuff inflation, head position.
Full Text:
INTRODUCTION
Nasotracheal intubation is an effective and potentially life saving approach to the difficult airway. Magill and Rowbotham developed and practiced the technique of “blind” nasal intubation and coined the term. [1] Blind nasotracheal intubation (BNTI ) was widely used in patients in whom orotracheal intubation was not possible e.g, patients of trismus. Recently, agents such as sevoflurane and propofol that allow depression of laryngeal reflexes and intubation with rapid recovery, as well as equipment such as the intubating fibreoptic laryngoscope, have resulted in the BNTI technique becoming rarely used in current practice. Flexible Fibreoptic assisted intubation has become the first choice when orotracheal intubation is difficult or impossible. But BNTI during spontaneous ventilation may still be useful when a Flexible Fibreoptic Laryngoscope is not available at all or not in the required size. Apart from this situation, flexible fibreoptic laryngoscopy is not possible when there is bleeding or secretions in the airway. [2] If it can be done easily, BNTI can remain a dependable technique in the armamentarium in the scenario of the difficult airway. Temporary inflation of the endotracheal tube cuff in the oropharynx has been shown to improve the success rates of BNTI. [3,4,5,6] The position of the head for BNTI was classically described as “sniffing the morning air” position, but studies have also shown that BNTI in neutral position of the head (no pillow under the occiput) has more success rate.[5] Craniofacial structure differences among ethnic populations are known. [7] Hence we conducted this hospital based cross-sectional study to evaluate the effect of tracheal tube cuff inflation and head position on the success of BNTI in our population with the hypothesis that neutral position of head and inflation of endotracheal tube cuff would aid BNTI.
MATERIAL AND METHOD
The study was conducted in our institute after approval by the Institutional Ethics Committee. A written informed consent was taken from the patients. Fifty two patients of either sex belonging to ASA I and II posted for surgery under general anaesthesia in a period of 12 months and consenting to participate in the study were included in the study. Inclusion and Exclusion Criteria – Patients in the age group of 18 to 60 years, belonging to American Society of Anaesthesiologists (ASA) status I and II, and posted for elective surgery were included in the study. Patients having coagulopathy and those on anticoagulants or antiplatelet agents, patients complaining of nasal obstruction, patients having nasal polpys or any other mass in nasal cavity on anterior rhinoscopic examination and patients with history of basal skull fractures were excluded from the study. All patients had an anterior rhinoscopy done prior to anaesthesia to rule out any nasal pathology. The more patent (i.e, open and unobstructed) nostril was determined by asking the patient to breathe through one nostril at a time with the mouth closed and feeling the blast of air during exhalation. The more patent nostril was then used for intubation. In cases where both nostrils were equally patent, the right nostril was chosen. The Mallampatti class of the patient was noted. The routine monitors like cardiac monitor, non-invasive blood pressure monitor and pulse oximeter were attached to the patient. Intravenous (IV) line was established. The nostrils were decongested with xylometazoline drops and then lubricated with 2% lignocaine jelly. The patient was placed supine on the Operation Theatre table without a pillow under his or her head (neutral position). All intubations were done by either author 1 or 3. The patient was premedicated with Midazolam 30 mcg/kg, 1.5 mcg/kg Fentanyl and 20 mcg/kg glycopyrrolate intravenously. General anaesthesia was then induced with intravenous Propofol 1% given slowly till loss of eyelash reflex. The anaesthesia was deepened with O2 + Isoflurane using Bain’s circuit with the patient breathing spontaneouly. Isoflurane was started at 0.6% and increased after every 2 breaths till a concentration of 2.5% was reached. When the patient was judged to be in adequate depth of anaesthesia by the muscle tone and the pattern of respiration, a polyvinyl chloride (PVC) ivory cuffed nasal tube (Internal Diameter 6 or 6.5 mm for female patient and 7 or 7.5 mm for male patient) was inserted in the nostril and gently advanced until there was a loss of resistance indicating that the tube had entered the oropharynx. At this time the proximal end of the endotracheal tube was connected to the Bain’s circuit, the other nostril was occluded and the mouth was kept closed by a finger below the chin of the patient. The movement of the rebreathing bag was then used as a guide to judge correct alignment of the tip of the tube and the glottis of the patient. Anaesthesia was maintained with O2 + Isoflurane via Bain’s circuit. If the bag movements decreased and the respiration became abdominal, the depth of anaesthesia was judged to be excessively deep and Isoflurane was decreased till the bag was moving adequately again. The sequence of head position and cuff inflation used in the patient was - 1) Head on table, endotracheal tube cuff deflated: HBCD. 2) Head on table, endotracheal tube cuff inflated with 15 ml of air: HBCI. 3) Head raised on pillow of 10 cms thickness, cuff deflated: HPCD. 4) Head raised on same pillow and cuff inflated with 15 ml of air: HPCI. This was done in the following manner. After the tube reached the oropharynx, it was advanced slowly. Proper alignment of the tip of the tube with the glottic opening resulted in good movement of the rebreathing bag. If on advancement of the tube, the bag movement stopped, the tube was withdrawn to the oropharynnx, cuff inflated with 15 ml of air and the tube was readvanced, again observing the bag movement. If bag movement stopped again, the cuff was deflated, tube withdrawn in the oropharynx, a pillow put under the patient’s occiput and the above procedure done again, first with cuff deflated and then with cuff inflated with 15 ml of air. In those patients who were intubated with cuff deflated, successful intubation was indicated by the bag movements continuing to be good or even improved when the tube was inserted to a depth of 27-28 cms. In those cases which we could intubate with cuff inflated, a resistance was felt as the tube was advanced when the cuff met the vocal cords while the bag movement continued to be good. The cuff was deflated when this occurred and the tube advanced further. A good bag movement with the tube inserted to 27-28 cms was taken to be a successful intubation. The confirmation of intubation was done by capnography. If the tube was palpated on either side of the larynx, the tube was withdrawn in the oropharynx, external laryngeal manipulation was done or the head was tilted on the same side and the tube readvanced. Two attempts of intubation were made in each position. If the patient could not be intubated in any of the conditions mentioned above, direct laryngoscopy was done and oral intubation done under vision. When the intubation was successful in any one position, the remaining positions of the head and the cuff were not tried. After extubation, the complications if any, were noted. Sore throat or irritation in the throat was taken to be present if the patient said so on being asked in the Post Anaesthesia Care Unit. Epistaxis was defined as bleeding from the nasal cavity that required some intervention to stop it. So only the presence of blood stained secretions during oral or nasal suction was not considered to be epistaxis. The “z” score between the intubations with cuff deflated and inflated with head on bed i.e HBCD and HBCI; with head on pillow i.e HPCD and HPCI; intubations with head on bed (HBCD+HBCI) and head on pillow (HPCD+HPCI) was calculated by proportion test using the software Epi.info version 3.4.3; level of significance α = 0.05.
RESULTS
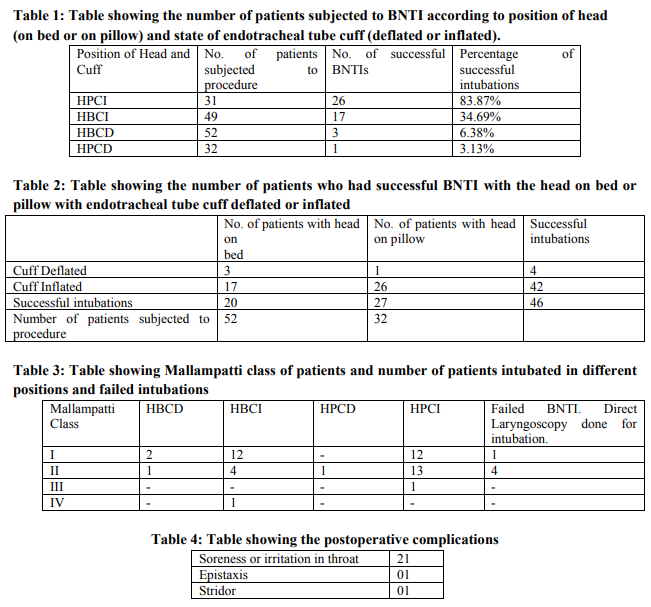
Out of 52 patients, one of the four positions was successful for blind nasotracheal intubation in 47 cases, i.e, a success rate of 90.38%. Only 5 cases (9.62%) required laryngoscopy for intubation. Among the successful BNTIs, the results were as follows (Tables 1 and 2). All 52 patients were first given a trial of BNTI with head on bed and cuff deflated (HBCD) position but in only 3 patients (6.38%) BNTI was successful in this position. In the remaining 49 patients, in 17 patients the BNTI was successful in the head on bed and cuff inflated (HBCI) position, i.e, 34.69% cases. In the remaining 32 patients, in only 1 patient BNTI was achieved in the head on pillow and cuff deflated position (HPCD), i.e, a success rate of 3.13%. In the now remaining 31 patients in the study, 26 could be intubated in the head on pillow and cuff inflated (HPCI) position, i.e, success rate was 83.87%. The remaining 5 cases (9.62%) required laryngoscopy for intubation. The z score by proportion test between HBCD and HBCI was 3.265 (p=0.0015, highly significant); between HPCD and HPCI was 4.89 (p=0.000006, highly significant); and between the two positions of head: on bed (HBCD+HBCI) and on pillow (HPCD+HPCD) was 2.73 (p=0.006, highly significant). Out of the 52 patients in this study, 27 patients were in modified Mallampati grade I; in 26 of these BNTI was successful, 1 patient required direct laryngoscopy for intubation. Out of 19 patients in modified Mallampati grade II, 13 could be intubated blindly but in 4 patients, BNTI was unsuccessful and direct laryngoscopy was required for intubation. There was 1 patient each in Modified mallampati grades III and IV and both could be intubated blindly with this technique. [Table 3] Complications seen postoperatively were as shown in the table [Table 4]. DISCUSSION Magill and Rowbotham pioneered blind nasal intubation. [1] Blind nasotracheal intubation is a technique learnt only by practice. Any maneuver that aids BNTI making it easier is therefore welcome. In the traditional method of doing BNTI, tube advancement after introducing the endotracheal tube in the nasopharynx is guided by the changes in the breath sounds at the proximal end of the tube and palpation of the larynx. Cessation of breath sounds indicates that the tip of the tube is not in alignment with the glottic opening. The tube is then withdrawn until the breath sounds are heard, head and neck position is adjusted and the tracheal tube is readvanced. Inflation of the endotracheal tube cuff to facilitate BNTI was first described by Gorback in 1987. [8] Previous studies have demonstrated that endotracheal tube cuff inflation in the oropharynx increases the success rate of BNTI. [3,4,5,6] In the presence of normal pharyngeal anatomy, inflation of the ETT cuff in the pharynx is assumed to center the tip of the tube with respect to the lateral wall of the pharynx. [9] Cuff inflation also would lift the endotracheal tube off the posterior pharyngeal wall and thus direct it towards the glottis. Magill described the position for blind nasal intubation thus: “The optimum position of the patient’s head for blind nasal intubation is simply that of a man sniffing the morning air. The head is in normal relation to the cervical vertebrae except for slight extension at the occiput-atlas junction. In this position the course of the airway from nose to the glottis is maximally open and a suitably curved rubber tube will follow that course naturally and enter the glottis in many cases. Of course, in the recumbent position a pillow under the occiput is usually necessary for this purpose”.[10] BNTI is also reported to be facilitated by neutral head position apart from endotracheal tube cuff inflation in spontaneously breathing patients. [5] In our study, we have assessed the effect of endotracheal tube cuff inflation as well as the position of the head on the success of BNTI. We have carried out the procedure on anaesthetized patients breathing spontaneously. Spontaneous ventilation confers the advantages of a widely opened larynx during inhalation. A good depth of anaesthesia was a precaution taken to prevent laryngospasm. The polyvinyl chloride ivory nasal tube was used to minimize the trauma caused. Of the PVC tubes available, this tube is most malleable for the nasal passage and yet retains the overall curve that is required for ease of laryngeal intubation. [11] After anaesthetizing the patient and after inserting the tube upto the oropharynx, we connected the tube to the Bain’s circuit. The movement of the rebreathing bag was good if the tube tip and the glottis were in alignment and decreased if the alignment was lost. Also, providing Oxygen and Isoflurane through the circuit helped us to maintain the oxygenation and the depth of anaesthesia. As per our protocol, the order of the positions in which BNTI was tried was HBCD, HBCI, HPCD and HPCI. Once intubation was achieved in any one position, the rest of the positions were not tried in order to prevent repeated unnecessary movement of the tube with respect to the laryngeal apparatus and hence the possibility of further irritation or trauma to the airway. Due to our protocol, among the successful BNTIs with endotracheal tube cuff inflated, all patients had been given a trial of intubation first with the endotracheal tube cuff deflated in that position of head (on bed or on pillow) in which they were intubated. To compare the effect of the inflation of endotracheal tube cuff on the success of BNTI, we compared the success rates of BNTI with the cuff inflated and those with cuff deflated in both the head positions. The rate of successful BNTI is 3/52 (6.38%) with cuff deflated (HBCD) and 17/49 (34.69%) with cuff inflated ( HBCI )with head on bed. [Table 1] The z score between these two is 3.265, p=0.0015 which is highly significant. With head on pillow, the success rate was 1/32 (3.13%) with cuff deflated (HPCD) and 26/31 (83.87%) with cuff inflated (HPCI). [Table 1] When these were compared the z score is 4.89, p=0.000006 which is also highly significant. This difference shows that tracheal tube cuff inflation increased the success of BNTI in any given position of the head . This could be as inflation of the cuff aligned the tube tip with the glottic opening. These results are in accordance to the previous studies. [3,4,5,6] To compare the effect of the head position (on bed versus raised with pillow under the occiput), we compared the total successful intubations on bed (with cuff inflated as well as with cuff deflated) with the total successful intubations with head raised on pillow (with cuff inflated as well as with cuff deflated) . 20/52 (HBCD+HBCI) i.e, 38.46% patients could be intubated with their head on bed and 27/32 (HPCD+HPCI) i.e, 84.38% with their head on pillow. [Table 2] The z score when these are compared was 2.73, P=0.006, highly significant. Thus the success of BNTI was more when the head was raised on a pillow as compared to when the head was on bed (neutral position). In this regard our results are not in accordance with the results of previous studies. [5] In our study, amongst the complications that we encountered [Table 4] most common was sore throat in the Post Anaesthesia Care Unit (PACU). Out of 52 patients, 21 (40.38%) patients had soreness or irritation of the throat when asked specifically in the PACU. These patients were treated with saline nebulization. A study on the comparison of glidescope videolaryngoscopy with direct laryngoscopy for nasotracheal intubation has found an incidence of moderate to severe sore throat in 34% patients. [12] One patient had epistaxis after extubation which was easily controlled by pinching the nostril for 2 minutes. One patient had stridor after extubation. Direct laryngoscopy revealed a blob of some transparent viscid material, probably the lignocaine jelly, near the cords. It was suctioned out and the stridor got relieved immediately. The failure rate of BNTI was 5/52 i.e, 9.62 %. We did not use any intubation aid and use of some aid like trachlite could have increased our success rate. Though patients of difficult intubation were not particularly included in this study the technique of endotracheal tube cuff inflation to aid blind nasotracheal intubation has been reported to be successful in patients anticipated to have difficult intubation like patients with limited mouth opening [3] and immobilized cervical spine in cases of cervical spine injury [4]. With respect to modified Mallampati score, the sample size in grade III and IV (Table 3) is too small to correlate the grade with success or failure of the technique of cuff inflation in aiding blind nasotracheal intubation. However it may be mentioned here that the Mallampati Classification was proposed as a clinical sign to predict difficult tracheal intubation on direct laryngoscopy.[13] Blind nasal intubation does not involve direct laryngoscopy. Our study has certain limitations. There was no randomization and this could have introduced some bias. Also, every patient did not undergo BNTI in all the four positions studied. When a patient was intubated in a particular position, the remaining positions of the head and the cuff were not tried. Hence the possibility that a patient could have been intubated in some later position also cannot be negated. However, all the 31 out of 52 patients in whom BNTI was successful with the head on pillow and with endotracheal tube cuff inflated had failed to be intubated in other three positions. Further study on the efficacy of endotracheal tube cuff inflation in aiding blind nasal intubation in anticipated cases of difficult intubation would provide more authenticity to this technique.
CONCLUSION
We conclude that endotracheal tube cuff inflation with the head raised on pillow is efficacious in achieving blind nasotracheal intubation in our population probably as in this position the endotracheal tube is in good alignment with the glottis opening.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to the authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Gold MI, Buechel DR. A Method of Blind Nasal Intubation in a Conscious Patient. Anesth Analg. 1960;39:257-63.
2. Nofal O. Awake light aided blind nasal intubation: prototype device. Br J A. 2010;104:254-7.
3. Van Elstraete AC, Pennet JH, Gajraj NM, Victory RA. Tracheal Tube Cuff Inflation as an aid to Blind Nasotracheal Intubation. Anaesthesia 2003;58:249-56.
4. Van Elstraete AC, Mamie JC, Mehdoui H. Nasotracheal intubation in patients with immobilized cervical spine: A comparison of tracheal tube cuff inflation and Fibreoptic Bronchoscopy. Anesth Analg. 1998;87:400-2.
5. Chung YT, Sheng Sun M, ShanWu H. Blind nasotracheal intubation is facilitated by neutral head position and endotracheal tube cuff inflation in spontaneously breathing patients. Can J Anaesth. 2003;50(5):511-3.
6. Casals-Caus P, Mayoral-Rojals V, Canales M A, Ruiz-Tamarit V, Casals-Castells A, Cochs-Cristià J. Inflation of the endotracheal tube cuff as an aid for blind nasotracheal intubation in patients with predicted difficult laryngoscopy. Revista Espanola De Anestesiologia Y Reanimacion .1997; 44(8): 302-4
7. Lam B, Ip MSM, Tench E, Ryan CF. Craniofacial profile in Asian and white subjects with obstructive sleep apnoea. Thorax 2005;60:504–510.
8. Gorback MS. Inflation of endotracheal tube cuff as an aid to blind nasotracheal intubation. Anesth Analg. 1987;66(9):917
9. Van Elstraete AC, Remy A. Difficult intubation: nasotracheal tube cuff inflation as an aid to difficult intubation. Ann Fr Anesth Reanim. 1994;13(6):873-5
10. Magill IW. Blind nasal intubation. Anaesthesia 1975;30:476-9
11. Hall CEJ, Shutt LE. Nasotracheal intubation for head and neck surgery. Anaesthesia 2003;58:249-56
12. Jones PM, Armstong KP, Armstrong PM, Cherry RA, Harle CC,Hoogstra J, Turkstra T. A comparison of Glidescope®videolaryngoscopy to direct laryngoscopy for nasotracheal intubation. Anesth Analg. 2008;107(1):144-8
13. Mallampati SR, Gatt SP, GuginoLD, Desai SP, Waraksa B, Freiberger D, Liu PL. A clinical sign to predict difficult intubation: a prospective study. Can Anaesth Soc J.1985;32 (1):429-34.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License