IJCRR - 6(20), October, 2014
Pages: 16-20
Date of Publication: 20-Oct-2014
Print Article
Download XML Download PDF
A RARE CASE OF TAKAYASU ARTERITIS WITH SECONDARY SUBCLAVIAN STEAL SYNDROME
Author: Basavaraj, Shashikumar M. R., Pradeep H. N., Pradeep C.N., Ismail M.
Category: Healthcare
Abstract:Takayasu arteritis (also known as pulseless disease, aortoarteritis, and aortic arch syndrome) is a chronic, inflammatory and
occlusive vasculitis of the aorta and its primary branches as well as the pulmonary arteries. It predominantly affects young
females, particularly from India and South East Asia.Subclavian steal syndrome secondary to takayasu arteritis occurs when there is severe stenosis or occlusion in subclavian artery which usually causes symptoms of vertebrobasilar territory. A case of Takayasu arteritis with thrombosis of bilateral subclavian arteries with subclavian steal syndrome affecting right subclavian artery is being reported here.
Keywords: Takayasu arteritis, Colour doppler ultrasonography, Carotid artery, Subclavian artery, Thrombosis
Full Text:
INTRODUCTION
Takayasu arteritis (TA) is a well-known yet rare form of large-vessel, chronic, progressive, inflammatory, and occlusive vasculitis. It involves primarily aorta and its main branches as well as coronary and pulmonary arteries, causing stenosis and/or obstruction due to thrombus formation, or dilatation due to aneurysmal formation and/ or rupture of involved arteries.[1–4] It is an idiopathic inflammatory disease of the large elastic arteries occurring in the young and resulting in occlusive or ectatic changes mainly in the aorta and its immediate branches as well as the pulmonary artery and its branches. Takayasu arteritis has multivessel involvement as seen by the frequent involvement of the arch of the aorta and its major branches, usually at the points of origin from the aorta, the most frequently affected arteries being the subclavian (90%), carotid (45%), vertebral (25%), and renal (20%)[2]. Color-coded Doppler sonography can facilitate the accurate diagnosis of Takayasu arteritis by the characteristic appearance.
CASE REPORT
A 23 year old female with pain in both upper limbs, absent pulses in both upper limbs, dizziness, headache, and elevated erythrocyte sedimentation rate was examined with color Doppler imaging ,duplex Doppler imaging and Magnetic Resonance Angiography(MRA).
FINDINGS
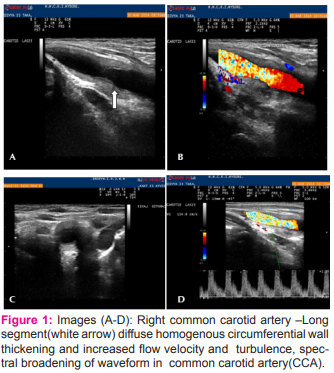
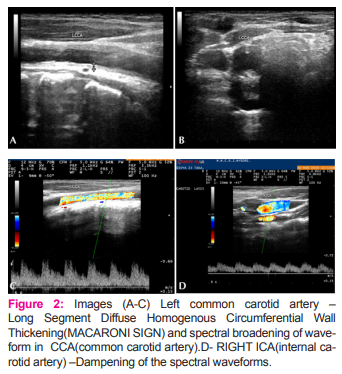
• Longitudinal and transverse color Doppler images of both the proximal common carotid arteries demonstrated a long segment of diffuse, homogenous, circumferential thickening of vessel wall, described as the “macaroni sign” with uniform color assignment within narrowed lumen (figure 1 & 2)
• Doppler waveform of both the proximal common carotid arteries showed increased flow velocities and turbulence and spectral broadening due to luminal narrowing caused by the thickened wall. Distal part of common carotid arteries on both sides appeared normal in calibre.Internal carotid arteries on both sides revealed dampened waveforms (fig 2).
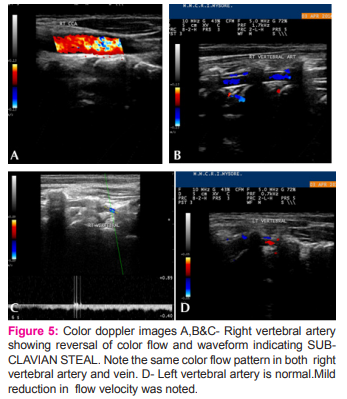
• Right vertebral artery showed reversal of flow with reduced flow velocity.(fig 5)
• Left vertebral artery was normal with mildly reduced flow velocity.
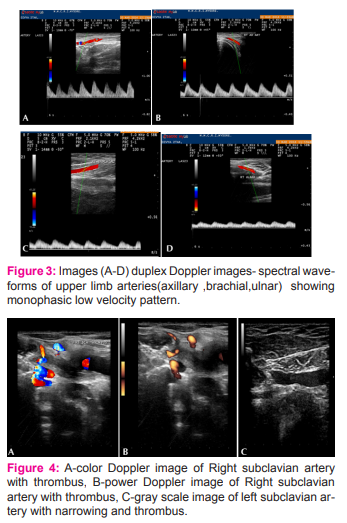
• Loss of the triphasic pattern in the right upper extremity arteries was noted.
Monophasic low flow velocities in both the upper extremity arteries due to proximal SCA occlusion and filling through the collaterals on both sides was noted.(fig 3) MRA of neck revealed complete non visualization of both subclavian from its origin on right side and just distal to its origin on left side with soft tissue signal intensities filling and occluding both lumen indicating complete thrombotic occlusion of both subclavian arteries.(fig 6)
DISCUSSION
TAKAYASU’S ARTERITIS
Takayasu arteritis is a chronic vasculitis of the aorta and its primary branches[1]. It predominantly affects young females, particularly from India and South East Asia. In the past, depending on some clinical manifestations,it was termed pulseless disease (Takayasu disease),aortic arch syndrome or atypical coarctation of the aorta, stenosing or constricting aortitis, and primaryarteritis[2]. Aortoarteritis has multivessel involvement , as seen by the frequent involvement of the arch of the aorta and its major branches, usually at the points of origin from the aorta, the most frequently affected arteries being the subclavian (90%), carotid (45%), vertebral (25%), and renal (20%)[2]. In 1990, aortoarteritis was defined and classified by the American College of Rheumatology as follows:“Takayasu’s arteritis is an idiopathic inflammatory disease of the large elastic arteries occurring in the young and resulting in occlusive or ectatic changes mainly in the aorta and its immediate branches as well as the pulmonary artery and its branches[3].” The most commonly affected artery in patients after initial diagnosis was found to be the left subclavian artery (SCA), followed by the right subclavian artery and the left common carotid artery (CCA).[3,4] In India, the female-male ratio varies from 1:1 to 3:1,[5] and the age of first appearance varies from 3 to 48 years.
PATHOLOGY
The pathology is a panarteritis characterized by mononuclear cells and occasionally giant cells, with marked intimal hyperplasia, medial and adventitial thickening, and, in the chronic form, fibrotic occlusion.Classically, the natural history of Takayasu arteritis has been described in 3 phases. The early prepulseless phase is characterized by systemic symptoms (ie, malaise, low-grade fever, weight loss, and arthralgia). It is followed by the phase of active vascular inflammation, when the clinical picture is dominated by pain localized over the affected area and the appearance of symptoms and signs of vascular insufficiency. Finally, fibrotic and stenotic lesions characterize the so-called burnout disease. However, the triphasic pattern of the disease can no longer be considered a rule, and the absence of systemic clinical features does not exclude ongoing vascular inflammation, nor does the presence of ischemic symptoms always indicate active inflammation of vessels.[6]
Sonographic Findings
Sonography is often the primary modality of investigation in a patient with signs and symptoms of aortoarteritis. Sonographic findings can be divided into the following according to the nature of the lesion,as described below[7].
Wall Thickening
This is the earliest finding in aortoarteritis and is universally seen in all patients with aortoarteritis. There is uniform thickening of the wall of the vessels involved . The earliest wall thickening is seen in the subclavian arteries, most commonly the left subclavian artery. The arch of the aorta is also involved early; however, because of difficulty in visualization of the aortic arch, the presence of aortoarteritis is inferred from assessment of the major aortic arch branches.[7,8] In Takayasu arteritis, long segments of diffuse, homogeneous, moderately echoeic circumferential vessel wall thickening are found. This is seen more commonly in the Common carotid artery in Takayasu arteritis and has been described as the “macaroni sign”. It can be distinguished from arteriosclerosis, which is more inhomogeneous.[9,10] An increase in wall thickness is associated with secondary signs such as decreased pulsatility and loss of a normal triphasic flow pattern. The involved vessels reveal loss of the triphasic pattern, with a monophasic or biphasic parvus tardus type of spectral flow pattern. This type of pattern is also seen distal to an occlusion when there is reformation of vessels by collaterals, but wall thickening associated with dampened flow suggests the diagnosis of aortoarteritis. Luminal Narrowing or Stenosis Luminal narrowing or stenosis is common in aortoarteritis because of wall thickening, which leads to a decrease in the luminal diameter. This stenosis or narrowing is commonly seen as a long segment, compared with atherosclerosis or fibromuscular dysplasia, in which the stenoses are commonly short segments.
Luminal Dilatation and Aneurysms Luminal dilatation and aneurysms are not as common as narrowing. It is suggested to be due to inadequate supportive fibrous tissue or focal intima weakness.[11] The aorta is most commonly affected, especially the thoracic and abdominal portions . Calcification Calcification is uncommon in aortoarteritis and more commonly seen in atherosclerosis. Occlusions Occlusions are seen in the later stages of the disease . Smaller vessels such as the carotid, subclavian, vertebral, and renal arteries are commonly involved. Because of the chronicity and slow progression of the disease, occlusions are commonly associated with collateral flow.[12] Pulsatility Pulsatility or compliance of the involved arteries has been found to be decreased in the pulseless stage of the disease in all cases of aortoarteritis. Changes in compliance have been known to precede the angiographic changes in vessels affected by aortoarteritis. Measurement of arterial compliance may provide indices of early vascular changes that predispose to the development of major vascular disease. Measurement of arterial stiffness could be useful in identifying the proliferative stage, the identification of which could be critical in early institution of treatment, which could prevent the further progression of the disease. Arterial compliance can be studied by various invasive and noninvasive methods.[13,14] Similar methods could be applied to the study of arterial compliance in patients with aortoarteritis.
Associated Organ Involvement
Heart Involvement of the heart is usually secondary to longstanding hypertension and ensuing congestive heart failure or left ventricular hypertrophy.[15] Congestive heart failure has been postulated to be a result of hypertension, rapidly developing pressure overload, and high levels of aldosterone and angiotensin II. Lung and Pulmonary Artery Various autopsy series have described involvement of the pulmonary arteries in aortoarteritis.[15,16] The pulmonary trunk is found to be more commonly involved compared with the intrapulmonary arteries. Cases appearing primarily as pulmonary hypertension without any involvement of the aorta have been described.[17] The differential diagnosis would include atherosclerosis, temporal arteritis, fibromuscular dysplasia, and idiopathic carotid dissection. Atherosclerosis may involve the common carotid artery ,but atherosclerotic plaque is usually more focal and asymmetric, occurs in an older patient population, and is accompanied by a normal erythrocyte sedimentation rate. In active temporal arteritis ,the erythrocyte sedimentation rate is elevated ,but the common carotid artery is not involved. Fibromuscular dysplasia affects the internal carotid artery but not the common carotid artery. Idiopathic carotid dissection typically involves only the internal carotid artery.[18] Subclavian Steal Syndrome[SSS]. Although incidence of TA associated with SSS is poorly documented in recent literature,actual occurrence of subclavian steal was more common than the associated syndrome.[19] Subclavian Steal Syndrome was generally characterized by neurologic symptoms of vertebral-basilar arterial distribution. Blood was siphoned along the vertebral artery because of low pressures distal to occlusion. The resulting steal phenomenon led to common symptoms of vertigo, syncope, and intermittent claudication of involved upper extremity. However, these symptoms alone rarely if ever resulted in permanent neurologic damage.[20] Doppler ultrasound was a noninvasive diagnostic tool currently used for diagnosis of Subclavian Steal Syndrome.[21,22] and was a good complement to angiography, still considered the gold standard. Both tools proved very helpful for diagnosis of Subclavian Steal Syndrome and Takayasu arteritis.[23]
TREATMENT
The process is progressive, and there is no definitive therapy. Glucocorticoids and immunosuppressive agents have been reported to be effective in some patients during the acute phase.[24] Surgical bypass or endovascular intervention of a critically stenotic artery may be necessary.[24]
CONCLUSION
In summary, takayasu arteritis has a characteristic set of findings at duplex sonography, and in the proper clinical setting , these findings appear to be diagnostic. Sonography of the carotid and subclavian arteries can be used to detect early Takayasu arteritis, but also to monitor disease progression and the effects of therapy. It is a quick, non-invasive technique without any radiation. The characteristic wall thickening of the carotid arteries and of the arteries of the limbs can even be evaluated by grey-scale ultrasonography whereas colour Doppler and duplex sonography are superior for other vessels and for the evaluation of flow characteristics.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
Schmidt WA, Nerenheim A,Seipelt E, Poehls C,Gromnica-Ihle E.Diagnosis of early Takayasu arteritis with sonography. Rheumatology 2002;41:496-502.
Eagle KA, De Sanctis RW. Diseases of the aorta. In: Braunwald E (ed). Heart Disease: A Textbook of Cardiovascular Medicine. 4th ed. Philadelphia, PA: WB Saunders Co; 1992:1528–1553.
Kinare SG, Gandhi MS, Deshpande JR. Nonspecific Aortoarteritis (Pathology and Radiology). Mumbai, India: Quest Publications; 1998.
Arrend WP, Michael BA, Block DA, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu’s arteritis. Arthritis Rheum 1990; 33:1129–1134.
Padmavati S, Aurora AP, Kasliwal RR. Aortoarteritis in India. J Assoc Physicians India 1987; 35:442–444.
Nasu T. Takayasu’s truncoarteritis: pulseless disease on aortitis syndrome. Acta PatholJpn 1982; 2(suppl 1):117–131.
Nitin Chaubal, Manjiri Dighe, Mohit Shah. Sonographic and Color Doppler Findings in Aortoarteritis(Takayasu Arteritis) .J Ultrasound Med 2004; 23:937–944 Matsunaga N, Hayashi K, Sakamoto I.Takayasu’s arteritis: protean radiologic manifestations and diagnosis. Radiographics 1997; 17:579–594. Kerr G. Takayasu’s arteritis. Curr Opin Rheumatol 1994; 6:32– 38. Maeda H, Handa N, Matsumoto M, et al.Carotid lesions detected by B-mode ultrasonography in Takayasu’s arteritis: “macaroni sign” as an indicator of the disease.Ultrasound Med Biol 1991; 17:695–701. Kozuka T, Nosaki T, Sato K, Tachiiri H.Aneurysm-associated aortitis syndrome.Acta Radiol 1968; 7:314–320. Sharma S, Rajani M. Aortic occlusion in nonspecific aortoarteritis (Takayasu disease):incidence and spectrum of involvement.Australas Radiol 1993; 37:57–59. Gamble G, Zorn J, Sanders G, et al. Estimation of arterial stiffness, compliance and distensibility from M-mode ultrasound measurements of the common carotid artery. Stroke 1994; 25:11–16. Emoto M, Nishizawa Y, Kawagishi T, et al. Stiffness index of the common carotid and femoral arteries are associated with insulin resistance in NIDDM. Diabetes Care 1998; 21:1178–1182. Arora P, Shankar J, Sethi KK, et al. Congestive cardiomyopathy in nonspecific aortoarteritis. J Assoc Physicians India 1985 3:589–591. Lupi-Herrera E, Sanchez-Torres G, Horwitz S.Gutierrez FE. Pulmonary artery involvement in Takayasu’s arteritis. Chest 1975; 67:69–74. Tyagi S, Kaul UA, Gambhir DS, et al. Pulmonary artery involvement in aortoarteritis. Indian Heart J1987; 39:415–419. Bond JR, Charboneau JW, Stanson AW. Takayasu’s arteritis:carotid duplex sonographic appearance including color doppler.Radiographics 1990;10:725-727 Lacey KO. Subclavian steal syndrome: a review. J Vasc Nurs 1996; 14:1–7. Smith JM, Koury HI, Hafner CD, Welling RE. Subclavian steal syndrome. A review of 59 consecutive cases. J Cardiovasc Surg (Torino) 1994;35:11–14. Kaneko A, Ohno R, Hattori K, Furuya D, Asano Y, Yamamoto T, Kim H, Shimazu K, Hamaguchi K. Color-coded Doppler imaging of subclavian steal syndrome. Intern Med 1998;37:259–264.34. Paivansalo M, Heikkila O, Tikkakoski T, Leinonen S, Merikanto J, Suramo I. Duplex ultrasound in the subclavian steal syndrome. Acta Radiol 1998;39:183–188. Rolda´n-Valade´z E, Herna´ndez-Mart?´nez P, Osorio-Peralta S, Espinoza-Cruz V and Casia´n-Castellanos G. Imaging Diagnosis of Subclavian Steal Syndrome Secondary to Takayasu Arteritis Affecting a Left-Side Subclavian Artery;Archives of Medical Research 2003;34: 433–438. Mark A.Creager,Joseph Loscalzo (2011) ‘Diseases of the Aorta’, in Dan Longo, Anthony Fauci, Dennis Kasper, Stephen Hauser, J. Jameson, Joseph Loscalzo (ed.)Harrison’s Principles of Internal Medicine 18th ed.. Newyork: McGraw Hill, pp. 2065.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License