IJCRR - 6(22), November, 2014
Pages: 29-38
Print Article
Download XML Download PDF
EARLY DETERIORATION IN QUALITY OF LIFE AND PHYSICAL FUNCTIONING OF MULTIPLE SCLEROSIS PATIENTS
Author: Ozge Ertekin, Serkan Ozakbas, Egemen Idiman
Category: Healthcare
Abstract:Objectives: (1) To examine the associations among ambulatory capacity, physical functioning and quality of life (QOL) in multiple sclerosis patients with different disability levels and compare the results to the healthy controls, and (2) to explain the relationship between QOL, disability status and disease duration. Methods: 112 multiple sclerosis patients and 50 healthy controls were selected for the study. Clinical and demographic data were recorded. Disability status (EDSS), walking ability and capacity (MSWS-12, T25FW), physical functioning (SF-36 /PF-10), QOL (MUSIQOL) and disease severity (MSIS-29) were evaluated. Outcome results of two subgroups with mild and moderate ambulatory impairment were analysed and compared with the control group. Results: There were a statistically significant difference between multiple sclerosis patients with low to moderate disability in MSWS-12, T25FW, SF-36 (PF-10) (p< 0.001), and MSIS-29 (p=0.018); additionally in the outcome results for EDDS (p< 0.001), MSWS-12 (p< 0.001), MSIS-29 (p=0.08) according to the physical functioning classification. Conclusions: The clinical impact of disability severity may contribute to impairments in walking, significantly influencing physical functioning in multiple sclerosis patients. QOL impairment may be emerged regardless of the disability level and disease duration.
Keywords: Multiple sclerosis, Disability, Walking, Physical functioning, Quality of life
Full Text:
INTRODUCTION
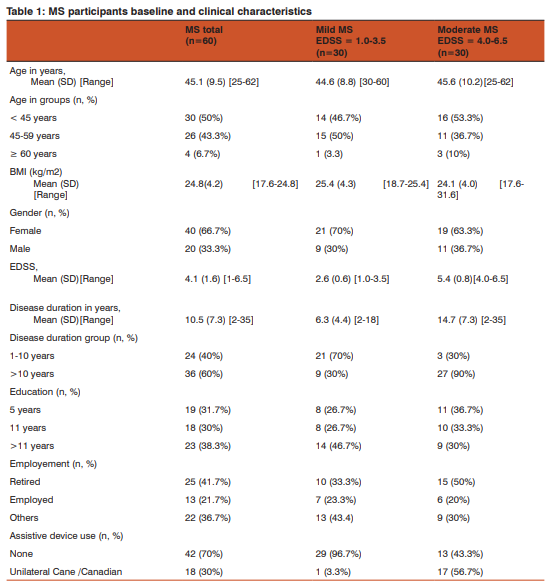
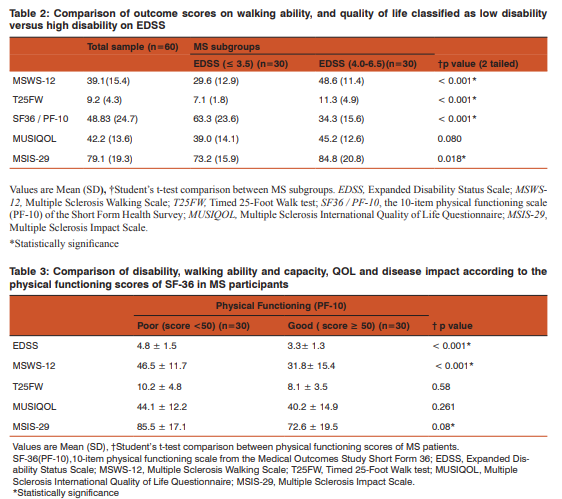
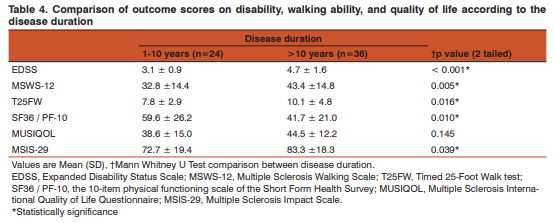
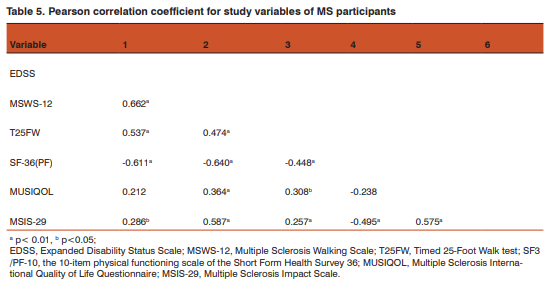
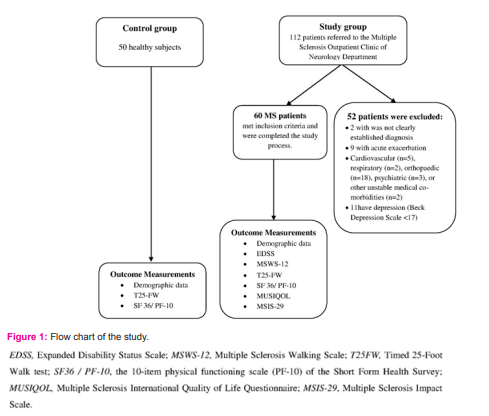
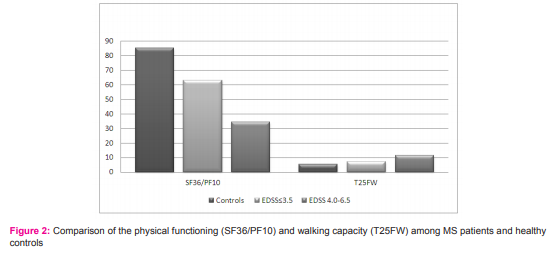
Multiple sclerosis (MS) is a chronic demyelinating disease resulting in functional limitations, disability and reduced quality of life (QOL) through the impairments such as muscular weakness, ataxia, spasticity, balance dysfunction, general fatigue, sensory disturbances, and visual vestibular disturbances1 . Walking ability, a marker of both disability and disease progression, is the most important part of physical disability in MS and has the major interest in rehabilitation 2,3,4,5,6,7. Although van Asch3 reported that the appearance of mobility difficulties were seen in almost all patients within 10 years of diagnosis, mobility impairment can begin early stages in the disease, with only one year of diagnosis. Recent studies have indicated that MS patients consider mobility impairment to be the most concerned symptom3,4, which have a significant impact on daily live and participation5,6. As shown in our recently published study, it has also a significant and long-term burden on caregivers, not restricted only to the patients’ life 7 . MS is not only associated with mobility loss, but it also has a severe negative impact on QOL. Previous research has shown that mobility impairment is an important cause of disability and reduced QOL in patients with MS, even when mobility loss is mild8,9,10, which may occur even in early stages of the disease11,12. MS patients having mild mobility disability in clinical assessments may have limitation in especially outside activities such as stairs and transportation, which may interrupt their QOL status earlier than expected. On the other hand, it will be not sufficient when walking impairment will evaluated without the environmental factors. Recently, Cavanaugh et al.12 reported that the ambulatory activity includes not only walking speed or cadence; it refers also physical activity behaviour such as walking, jogging, stair climbing, which includes daily activities in life. The quality of life deteriorations and mobility impairments appeared in multiple sclerosis at the mild to mod erate disability level may be an important determinant of long-term MS rehabilitation goals and need further investigation as well as it’s relation with physical functioning and disease duration. Thereby it will be possible to provide the appropriate physiotherapy and rehabilitation approaches on aspects of location, duration and intensity. Our purposes were (a) to examine the associations among ambulatory capacity, physical functioning and QOL in MS patients with different disability levels and compare the results to the healthy controls (b) to explain the relationship between QOL and disability status as well as disease duration. METHOD Participants: 112 ambulatory individuals with Multiple Sclerosis (MS) referred to the Multiple Sclerosis Outpatient Clinic of Neurology Department of the Dokuz Eylul University School of Medicine were assessed for eligibility. Inclusion criteria of the study were 1) clinically or laboratory definite relapsing remitting, primary progressive or secondary progressive multiple sclerosis according to Poser’s criteria13 2) aged 18-75 years, 3) EDSS between 1.0 and 6.5, 4) cooperated, and 5) volunteer to join to the study. Patients were excluded if their diagnosis was not clearly established (n=2), they were suffering from an acute relapse (in the last 30 days) prior to the first examination (n=9), history of cardiovascular (n=5), respiratory (n=2), orthopaedic (n=18), psychiatric (n=3), or other unstable medical co-morbidities (n=2), and having depression according to Beck Depression Scale (n=11). The study was approved by the head of the department and passed the ethics committee review of the university. Written informed consent was received from all participants. The physical therapist administered the evaluation scales. EDSS was performed by the neurologist. Data Collection: Demographic characteristics, socioeconomic status and medical history recorded by questionnaire included age, gender, height, weight, and body mass index, education, employment, disease duration, assistive device use (cane/canadian), and EDSS group specified for both total MS patients and subgroups. Disability Status: The severity of disability was stated with the Kurtzke Expanded Disability Status Scale (EDSS)14. Patients were subdivided in subgroups with mild (EDSS<4.0) and moderate (EDSS ≥ 4.0-6.5) ambulatory dysfunction15. Walking ability and capacity: Walking ability was measured with the Multiple Sclerosis Walking Scale-12 (MSWS-12). This scale has 12 questions about the limitation degree according to MS in the past two weeks. Scores range between zero (0) and 80 and higher scores show worse walking ability or more walking difficulty16. Walking capacity was measured using the Timed 25-Foot Walk (T25FW), which is a known indicator of ambulatory impairment and a component of the Multiple Sclerosis Functional Composite. Higher values reflect greater limitation12,17. Physical functioning: Physical functioning was measured with the 10-item physical functioning scale (PF-10) from the Medical Outcomes Study Short Form 36 (SF-36)18. The scale is scored from 0 to 100, with 100 being the highest level of functioning. Physical functioning of the participants were classified into good (score ≥50, n=30) or poor (<50, n=30) in accordance with the reference values of Nogueira et al.19. Health-Related Quality of life: Multiple Sclerosis International Quality of Life (MUSIQOL) questionnaire is a multi-dimensional, self-administered and disease-specific quality of life scale. Lower scores show higher level of quality of life. The validity and reliability of the MUSIQOL were established in patients with MS20. Disease Severity: The Multiple Sclerosis Impact Scale (MSIS-29) can be used to measure therapeutic outcome in a patient with MS. There are 29 items covering findings over the previous two weeks: three items dealing with limited abilities and 26 items related to being bothered by symptoms or consequences of illness. The higher is the score the greater is the degree of disability with a minimum score of 29 and maximum score of 145)21. Control group assessments included demographic characteristics, physical functioning (SF-36/PF-10) and walking capacity (T25-FW). Data Management and Statistical Methods All statistical analyses were performed use of the Statistical Package for the Social Sciences Software (version 15.0, SPSS Inc., 233 South Wacker Drive, 11th Floor, Chicago, IL, 60606-6307). All results are reported as mean and standard deviations (SD). Descriptive statistics were used to summarize demographic and baseline characteristics. Potential baseline differences between subgroups and control group outcomes of the participants were analysed using the Student’s t-test for independent samples. Potential baseline differences according to gender and disease duration for outcome scales of the patients were analysed using the Mann Whitney U test. All analyses were performed on an intention-to-treat basis. All tests were two-tailed and the level of significance was set at p11 years, 30% had 11 years, and 31.7% had five years education) and mostly retired (41.7%). 30% of the patients had a cane or canadian as an assistive device (Table 1). Comparison of the outcome measures according to the disability subgroups Table 2 shows the comparison of the outcome measures of the patients classified as the disability status on EDSS. While age and body mass index (BMI) were not significantly different between subgroups of mild and moderate disability (p=0.677, p=0.255, respectively), disease duration was significantly higher in moderate disability group (p10 years). Patients having longer than 10 years disease duration (n=36) showed significantly worse scores in EDSS, MSWS-12, T25FW, SF-36 (PF) and MSIS-29 (p0.05).
DISCUSSION
The present study highlighted that the clinical impact of disability severity may contribute to impairments in walking, significantly influencing physical functioning in MS patients. Additionally, QOL impairment may be emerged regardless of the disability level and disease duration. Researchers highlighted that walking impairment has been demonstrated early in the MS disease process and at low levels of disability, with and without clinical signs of pyramidal dysfunction. It is evident that low levels of disability and mobility impairment have substantial effects on the daily lives of people with MS6,22,23. Additionally walking and mobility are clinical significant indicators of disease progression and disability12,14. Accordingly, the use of walking specific scales and measures in clinical studies and also in practice has increased. Hutchinson et al.24, reported an agreement that in a clinical setting, gait outcome measurements such as the T25FW test and self-reported MSWS-12 should be the tools initially included. In our study, ambulatory functional capacity was evaluated with the T25FW test25, 26, which is known as the standard index for gait impairment in MS5,17,27,28. In the current study, persons with MS who had moderate disability showed worse ambulatory capacity than those with mild disability. However, the patients even with mild disability showed impaired levels of ambulatory functional capacity at T25FW test compared with the control group. Similarly, Johansson et al.29 reported that 22% of the patients with mild disability based on EDSS scores of 1.0-3.5, demonstrated walking impairment in the T25FW. Therefore, the walking impairment appeared at the mild disability level may be an important determinant of long-term MS rehabilitation goals and need further investigation. De Groot et al.30 concluded that patient-based outcome scales will be more sensitive than physician-based or objective MS rating scales. As recent researches reported that the most affected mobility-related activities in MS were outside walking, stair activity, transportation, dressing, and social activities31,32,33, this self-reported scale may be helpful to assess the walking impairment detailed. Additionally, this scale has been suggested to be more responsive to change than either the EDSS or T25FW16, defining the limitations of walking distance, walking effort, and the use of support and the ability to run. Thus we assessed self-reported, patient-based walking impairment with the MSWS-12, which measures different aspects of walking than the objective walking measures. Our participants with higher disability had significantly worse scores on the walking ability, so they had much more difficulty in walking. Therefore, it may be important to evaluate the walking deficits not only with clinical test but also with daily outside activities. Nogueira et al.19 showed the effect of functional limitations on the QOL in people with MS and stated that the most affected domain was that of physical functioning. A recent study34 reported that patients with recently diagnosed MS reported significantly lower on SF-36 physical functioning (PF-10) subscale, compared with controls. Pugliatti et al.35 reported that the SF-36 (PF-10) subscale seemed to indicate physical functioning more sensitively than EDSS. In our study, EDSS scores are highly correlated with physical functioning, consistent with the literature36. Beckerman et al.37 reported that in the first 10 years after definite diagnosis, patients with multiple sclerosis showed a more pronounced decline in physical functioning than in cognitive and social functioning. We found that patients having disease duration more than 10 years reported significant impairment in physical functioning, walking ability and disability level compared with patients having lower than 10 years disease duration. It may be suggested that the progressive nature of the disease has to be considered while developing programs in rehabilitation process. In addition to this, consistent with previous reports, SF-36 (PF-10) subscale has been showed to correlate well with walking assessments such as the MSWS-1216. In the present study, after classification of physical functioning into good (score ≥50) or poor (<50) in accordance with the reference values19, there was a strong significance for disability, walking ability and disease impact, except from QOL between MS subgroups. The interaction between these domains will be predictable and reported before, since physical functioning will be declined as disease progressed8 . However, this data may be considered to give more importance to QOL assessments, which will be negatively influenced also in patients with good physical functions. Mobility impairment is an important cause of disability and reduced QOL in patients with MS, even when mobility loss is mild8,9,10. For this reason, mobility evaluation may be especially important to build up strategies to prevent and/ or diminish the disability status. We demonstrated that our patients even with mild disability reported walking limitations. Additionally, we assessed QOL in MS individuals with a disease specific questionnaire20, and compared these results according to disability status on EDSS and SF-36 (PF-10) subscale. While all patients with mild to moderate disability reported impaired QOL, the difference was not significant, which may explain that the negative results in QOL can begin irrespective of the disability level and physical functional status of the patients. Therefore, patients having mild mobility disability in clinical assessments may have limitation in especially outside activities such as stairs and transportation. As a consequence they may experience early deterioration of their QOL. This results emphasis the necessity of physical activity programmes for MS patients more inactive than the other chronic diseases to improve QOL. In the present study, the physical and psychological impact of MS from the patient’s perspective was compared according to the disability level with both disability level and physical functioning. Patients with higher disability and poor physical functioning showed greater limitation in Multiple Sclerosis Impact Scale (MSIS-29) than lower disability and good physical functioning consistent with the literature, that researchers reported high correlation between MSIS-29 physical disease impact and disability on EDSS38,39. Hoogervorst et al.38 noted that patients with an EDSS>6.5 scored significantly higher on the MSIS29 physical score than patients with a low EDSS score (≤3.5). In the present study, consistent with the literature3,29, the patients with both mild and moderate disability were classified by significantly reduced ambulatory capacity. Additionally, as MS-related disability progresses, MS patients have associated deteriorations in walking ability, which confirm previous reports on the progressive deterioration of mobility in this disease. We demonstrated also that loss of mobility was significantly associated with physical functioning loss. Some limitations of this study should be acknowledged. One limitation is that we collected data at one point in time. Another limitation is that because fewer patients included to this study, the generalizability of our findings are restricted. To conclude, the results of the present study that the clinical impact of disability severity may contribute to impairments in walking, significantly influencing physical functioning in even mild disability MS patients shown previously11,12. However, it has to be noted that even patients with mild mobility disability may experience early deterioration of their QOL. Therefore our results support the importance of early assessment and treatment of decreases in mobility to improve QOL and strategies to define and focus on gait disturbances at early stages of disease may be crucial, which may help to decrease the detrimental impact of disability. We furthermore suggest that the effect of the parameters such as depression, fatigue and also caregiver burden on early mobility impairment might be valuable, especially from the patient perspective.
ACKNOWLEDGEMENTS:
We thank all our participants with multiple sclerosis for their assistance and cooperation. We acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. We are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Motl RW, McAuley E, Snook EM, Gliottoni RC. Physical ac- Physical activity and quality of life in multiple sclerosis: intermediary roles of disability, fatigue, mood, pain, self-efficacy and social support. Psychol Health Med 2009; 14(1):111-24.
2. Weikert M, Suh Y, Lane A, Sandroff B, Dlugonski D, Fernhall B, et al. Accelerometry is associated with walking mobility, not physical activity, in persons with multiple sclerosis. Med Eng Phys. 2012; 34(5): 590-7.
3. Van Asch P. Impact of mobility impairment in multiple sclerosis 2 patient perspectives. Eur Neurol Rev. 2011; 6: 115–20.
4. Heesen C, Bohm J, Reich C, Kasper J, Goebel M, Gold SM. Patient perception of bodily functions in multiple sclerosis: gait and visual function are the most valuable. Mult Scler. 2008; 14: 988–91.
5. Kieseier BC, Pozzilli C. Assessing walking disability in multiple sclerosis. Mult Scler. 2012; 18(7): 914-24.
6. Panitch H, Applebee A. Treatment of walking impairment in multiple sclerosis: an unmet need for a disease-specific disability. Expert Opin Pharmacother. 2011; 12(10): 1511- 21.
7. Ertekin Ö, Özakba? S, ?diman E. Caregiver Burden, Quality of Life and Walking Ability in Different Disability Levels of Multiple Sclerosis. NeuroRehabilitation 2014; 34: 313-21.
8. Aronson KJ. Quality of life among persons with multiple sclerosis and their caregivers. Neurology 1997; 48: 74-8.
9. Chruzander C, Ytterberg C, Gottberg K, Einarsson U, Widén Holmqvist L, Johansson S. A 10-year follow-up of a population-based study of people with multiple sclerosis in Stockholm, Sweden: changes in health-related quality of life and the value of different factors in predicting healthrelated quality of life.J Neurol Sci. 2014; 15: 339(1-2):57- 63.
10. Paltamaa J, Sarasoja T, Leskinen E, Wikström J, Mälkiä E. Measures of physical functioning predict self-reported performance in self-care, mobility, and domestic life in ambulatory persons with multiple sclerosis. Arch Phys Med Rehabil. 2007; 88: 1649-57.
11. Salter AR, Cutter GR, Tyry T, Marrie RA, Vollmer T. Impact of loss of mobility on instrumental activities of daily living and socioeconomic status in patients with MS. Curr Med Res Opin. 2010; 26: 493-500.
12. Cavanaugh JT, Gappmaier VO, Dibble LE, Gappmaier E. Ambulatory activity in individuals with multiple sclerosis. J Neurol Phys Ther. 2011; 35(1): 26-33.
13. Poser CM, Paty DW, Scheinberg L, McDonald WI, Davis FA, Ebers GC, et al. New diagnostic criteria for multiple sclerosis: guideliness for reserach protocols. Ann Neurol. 1983; 13: 227-31.
14. Kurtzke JF. Rating neurological impairment in multiple sclerosis: an Expanded Disability Status Scale (EDSS). Neurology. 1983; 33: 1444-52.
15. Ertekin Ö, Özakbas S, diman E, Algun ZC. Quality of Life, Fatigue and Balance Improvements after Home-Based Exercise Programme in Multiple Sclerosis Patients. Archives of Neuropsychiatry. 2012; 49 (1): 33-8.
16. Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ. Measuring the impact of MS on walking ability: The 12-Item MS Walking Scale (MSWS-12). Neurology. 2003; 60: 31-6.
17. Gijbels D, Dalgas U, Romberg A, de Groot V, Bethoux F, Vaney C, et al. Which walking capacity tests to use in multiple sclerosis? A multicentre study providing the basis for a core set. Mult Scler. 2012; 18 (3): 364-71.
18. Koçyiit H, Aydemir Ö, Fi?ek G, Ölmez N, Memi A. K?sa Form-36 (KF-36)’nn Türkçe versiyonunun güvenilirli?i ve geçerlili?i. ?laç ve Tedavi Dergisi. 1999; 12: 102-6.
19. Nogueira LA, Nóbrega FR, Lopes KN, Thuler LC, Alvarenga RM. The effect of functional limitations and fatigue on the quality of life in people with multiple sclerosis. Arq Neuropsiquiatr. 2009; 67(3B): 812-7.
20. Simeoni MC, Auquier P, Fernandez O, Flachenecker P, Stecchi S, Constantinescu CS, et al, on behalf of the MUSIQOL study group. Validation of the Multiple Sclerosis International Quality of Life questionnaire. Mult Scler. 2008; 14(2): 219-23.
21. Hobart J, Lamping D, Fitzpatrick R, Riazi A, Thompson A. The Multiple Sclerosis Impact Scale (MSIS-29): a new patient-based outcome measure. Brain. 2001; 124(Pt 5), 962-73.
22. Martin CL, Phillips BA, Kilpatrick TJ, Butzkueven H, Tubridy N, McDonald E, et al. Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Mult Scler. 2006; 12: 620-8.
23. Dalgas U, Kjølhede T, Gijbels D, Romberg A, Santoyo C, de Noordhout BM, et al. Aerobic intensity and pacing pattern during the six-minute walk test in patients with multiple sclerosis. J Rehabil Med. 2014; 46(1): 59-66.
24. Hutchinson B, Forwell SJ, Bennett S, Brown T, Karpatkin H, Miller D. Toward a consensus on rehabilitation outcomes in MS: gait and fatigue. Int J MS Care. 2009; 11: 67-78.
25. Fischer JS, Rudick RA, Cutter GR, Reingold SC. The Multiple Sclerosis Functional Composite Measure (MSFC): an integrated approach to MS clinical outcome assessment. National MS Society Clinical Outcomes Assessment Task Force. Mult Scler. 1999; 5(4): 244-50.
26. Kragt JJ, van der Linden FA, Nielsen JM, Uitdehaag BM, Polman CH. Clinical impact of 20% worsening on Timed 25-foot Walk and 9-hole Peg Test in multiple sclerosis. Mult Scler. 2006; 12(5): 594-8.
27. Rudick R, Antel J, Confavreux C, Cutter G, Ellison G, Fischer J, et al. Recommendations from the national multiple sclerosis society clinical outcomes assessment task force. Ann Neurol. 1997; 42(3): 379–82.
28. Kaufman M, Moyer D, Norton J. The significant change for the Timed 25-foot Walk in the multiple sclerosis functional composite. Mult Scler. 2000; 6(4):286-90.
29. Johansson S, Ytterberg C, Claesson IM, Lindberg J, Hillert J, Andersson M, et al. High concurrent presence of disability in multiple sclerosis. Associations with perceived health. J Neurol. 2007; 254(6): 767-73.
30. De Groot V, Beckerman H, Uitdehaag BM, de Vet HC, Lankhorst GJ, Polman CH, et al. The usefulness of evaluative outcome measures in patients with multiple sclerosis. Brain. 2006; 129: 2648–59.
31. Einarsson U, Gottberg K, Fredrikson S, von Koch L, Holmqvist LW. Cognitive and motor function in people with multiple sclerosis in Stockholm County. Mult Scler. 2006; 12: 340-53.
32. Zwibel HL. Contribution of impaired mobility and general symptoms to the burden of multiple sclerosis. Adv Ther. 2009; 26(12): 1043-57.
33. Sutliff MH. Contribution of impaired mobility to patient burden in multiple sclerosis. Curr Med Res Opin. 2010; 26(1): 109-19.
34. Klevan G, Jacobsen CO, Aarseth JH, Myhr KM, Nyland H, Glad S, et al. Health related quality of life in patients recently diagnosed with multiple sclerosis. Acta Neurol Scand 2014; 129(1):21-6.
35. Pugliatti M, Riise T, Nortvedt MW, Carpentras G, Sotgiu MA, Sotgiu S, et al. Self-perceived physical functioning and health status among fully ambulatory multiple sclerosis patients. J Neurol. 2008; 255(2): 157-62.
36. Nortvedt MW, Riise T, Myhr KM, Nyland HI. Quality of life in multiple sclerosis: measuring the disease effects more broadly. Neurology. 1999; 22; 53(5): 1098-103.
37. Beckerman H, Kempen JC, Knol DL, Polman CH, Lankhorst GJ, de Groot V. The first 10 years with multiple sclerosis: the longitudinal course of daily functioning. J Rehabil Med. 2013; 45(1): 68-75.
38. Hoogervorst EL, Zwemmer JN, Jelles B, Polman CH, Uitdehaag BM. Multiple Sclerosis Impact Scale (MSIS-29): relation to established measures of impairment and disability. Mult Scler. 2004; 10(5): 569-74.
39. van der Linden FA, Kragt JJ, Klein M, van der Ploeg HM, Polman CH, Uitdehaag BM. Psychometric evaluation of the multiple sclerosis impact scale (MSIS-29) for proxy use. J Neurol Neurosurg Psychiatry. 2005; 76(12): 1677-81.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License