IJCRR - 7(1), January, 2015
Pages: 28-33
Print Article
Download XML Download PDF
EVALUATION OF LIVER SPACE OCCUPYING LESION WITH SPECIAL REFERENCE TO ETIOLOGY AND CO-MORBID CONDITION
Author: Sahid Imam Mallick, Phani bhusan Sarkar, Sauvik Dasgupta, Auriom Kar, Soumavo Mukherjee, Sneha Jatan Bothra, N B Debnath
Category: Healthcare
Abstract:Background: Identifying etiology and co-morbid conditions of SOL liver is important for further management. Objectives: To evaluate the different causes of Space Occupying Lesion (SOL) of liver and find out etiology of liver tumor among patients of SOL of liver and also short term follow up of treatable condition.
Method: Observational study is done over 1 year on 40 patients aged above 12 years with SOL liver who has attended General Medicine outdoor and/or indoor of NRS Medical College and Hospital. Longitudinal type of prospective study techniques have
been used to analyses data.
Results: The study shows that the highest percentage (27.5) of SOL seen in 51-60 years of age group and male were affected more than females (70% and 30% respectively). Metastatic adeno carcinoma was the commonest cause of liver SOL (32.55) followed
by amoebic and pyogenic liver abscess (20% and 15% respectively). On 6 months follow up there was 83.33% complete
resolution of pyogenic abscesses and 37.5% complete resolution of amoebic liver abscesses.
Conclusion: Majority of liver SOL are metastatic adenocarcinoma. Next common SOL is amoebic liver abscess, followed by
pyogenic liver abscess. Majority of liver abscesses responded with antibiotics.
Keywords: Liver, Space Occupying Lesion (SOL), Adenocarcinoma, Liver abscess
Full Text:
INTRODUCTION
Space Occupying Lesion (SOL) on liver can be caused by various diseases that may or may not be manifested with symptoms. Mass lesions of the liver occur quite frequently, thus clinicians interested in liver diseases should have a thorough understanding of their presentations, diagnosis and treatment. Hepatic mass lesions include tumors, tumor-like lesions, abscesses, cysts, hemartomas and confluent granulomas. The frequency with which each is seen varies in different geographic regions and different populations. Focal nodular hyperplasia is more common than hepatocellular adenoma. Focal nodular hyperplasia occurs at all ages, but most patients present in the third and fourth decades of life.(1) The cause of focal nodular hyperplasia is unknown. Some evidence suggests that focal nodular hyperplasia may be hormone-dependent.(2), (3) The liver is the most common destination of hydatid cyst (70%), followed by the lungs (20%), kidney, spleen, brain, and bone. The sensitivity and specificity of both ultrasonography and CT in confirming the diagnosis are high. (4) In adults in most part of the world, hepatic metastasis are more common than primary malignant tumors of the liver, whereas in children, primary tumors outnumber both metastases and benign tumors of the liver. Hepatic metastases occur in 40% to 50% of adult patients with extra hepatic primary malignancies.(5) Most cases of pyogenic liver abscess are cryptogenic or occur in older men with underlying biliary tract disease.(6) Different liver SOL has different etiology and risk factor, so it is important to find out etiology and risk factor in Indian subcontinent, which would help us to treat different kind of SOL of liver.
MATERIALS AND METHODS
This observational study was conducted among the liver SOL patients who attended Medicine OPD and indoor of Nil Ratan Sirkar (NRS) Medical College, Kolkata. The study participants were above 12 years of age. The study was conducted for about 1 year. The sample size of 40 were included who were satisfying inclusion criteria. The inclusion criteria were patients having clinically and radiologically confirmed hepatic SOL above 12 years of age with consent from patient’s relatives. The patients who were seriously ill and age below 12 years were excluded from this study. The data was collected to study demographic profile like age, sex, religion and assessment of co morbid condition and risk factors. All patients were undergone detailed clinical examination and routine as well as specific blood and imaging study. Longitudinal type of prospective study was used as study techniques. Ethical committee approval was obtained from the Institutional Ethical Committee of Nil Ratan Sircar Medical College, Kolkata. After obtaining the required permission from the Medical college and hospital, the study participants were briefed about the nature and purpose of the study.
RESULTS
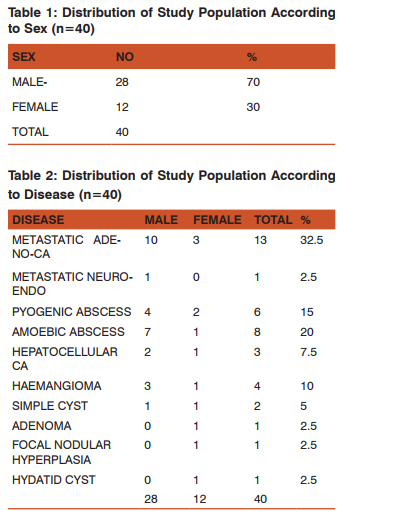
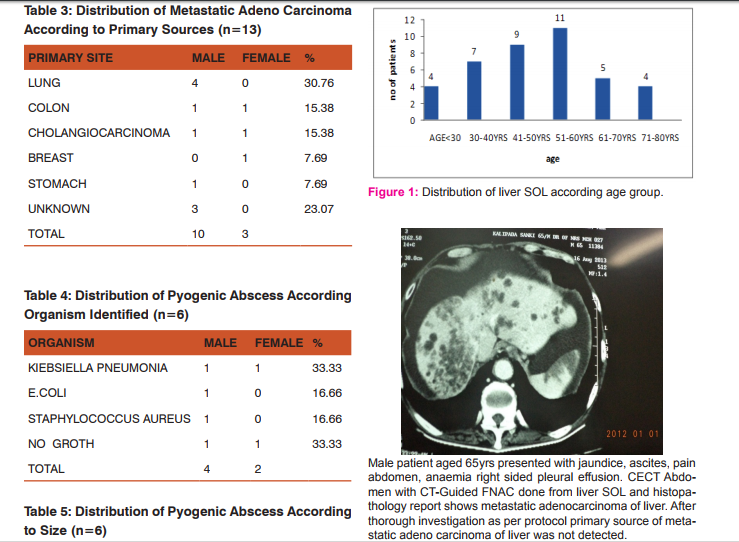
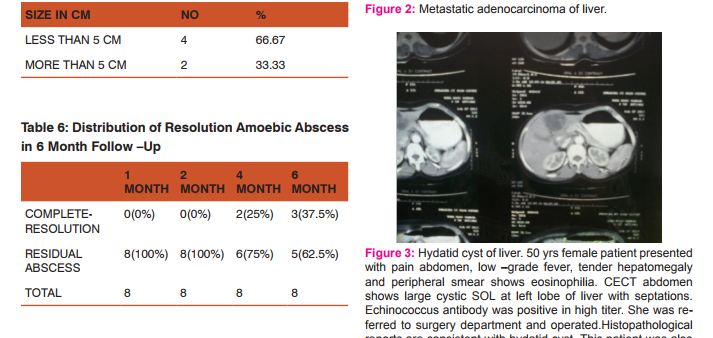
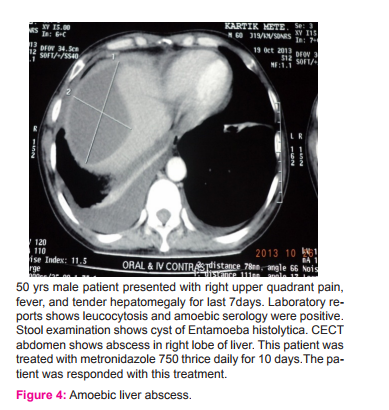
A total of 40 patients above the age of 12 years with liver SOL were studied regarding their demographic profile, etiology, co-morbidity, and risk factor. The present study was carried out at the department of medicine, N.R.S Medical College and Hospital, Kolkata from February 2012 to March 2013. In this study it has been seen that highest percentage (27.5%) of SOL seen in 51-60 age group. Figure 1 showing distribution of liver SOL according to age group. This study reveals 70% of male having liver SOL and 30% of female having liver SOL. Table number 1 showing distribution of study population according to sex. In this study out of 40 patients Hindu patients were 34(85%) and Muslim patients were 6(15%). Metastatic adenocarcinoma was commonest cause of liver SOL found in our study (32.5%), out of which 10 patients were male and 3 were female. Amoebic liver abscess was second most common cause of liver SOL in our study (20%), followed by Pyogenic liver abscess (15%). Haemangioma was found in 10% of population and 7.5% of patient had Hepatocellular carcinoma. Simple liver cyst was found in 5% of patient. Metastatic neuro-endocrine tumor, Adenoma, Hydatid cyst and Focal Nodular Hyperplasia were the other causes of liver SOL found in our study (each 2.5%). Among the metastatic adenocarcinoma, lung was the commonest primary site (39.76%) found in our study. In 3 patients we could not locate the primary site (i.e. 23.07%). Colon and Cholangiocarcinoma was primary site in 15.38% of patients among the Metastatic adenocarcinoma. Table No. 3 showing distribution of Metastatic adenocarcinoma according to primary source. Table 4 showing Klebsiella pneumonia was the commonest organism causing pyogenic liver abscess (33.33%), whereas in same percentage of patients of liver abscess no growth were found. Among the Pyogenic liver abscess patients 4 patients had less than 5 cm of abscess size (67.67%) and more than 5 cm abscess size was found in 2 patients (33.33%). Out of 6 Pyogenic liver abscess patients 4 were treated with antibiotics only and other 2 were treated jointly with antibiotics and aspiration. Among 6 Pyogenic liver abscess patients 3 patients had co-morbid condition like Diabetes Mellitus and 1 patient had Cholangitis. Out of 8 Amoebic liver abscess patients found in our study, 7 were male (87.5%) and 1 patient was female (12.5%). 75% Amoebic liver abscesses were single in number and 25% were single abscess. In our study, all 8 amoebic abscesses were less than 5 cm in size. All 8 patients of amoebic abscess in our study were responded well to treatment with Metronidazole and Diloxanide fuoate. Two hepatocellular carcinoma patients have Hepatitis C (66.66%) and other patient has Hepatitis B (33.33%). Cirrhosis of liver and alcoholism were present in 2 patients of hepatocellular carcinoma. 3 male and 1 female patients were found to have hemangioma in our study. Both the benign tumor of liver, namely adenoma and focal nodular hyperplasia were found in female only. And in both the case, oral contraceptive pill was common risk factor. Amoebic and pyogenic liver abscess patients were followed up in OPD on regular interval. After 6 months 83.33% of pyogenic liver abscess patients had complete resolution and 16.67% had residual abscess. Whereas, in case of amoebic liver abscess, only 37.5% had complete resolution and 62.5 %( Table No. 6) had residual abscess after 6 months of follow up.
DISCUSSION
A. Demography, Etiology and Risk factors :
• During one year study period total 40 cases selected randomly satisfied inclusion criteria attending medicine outpatient department and inpatient department. Minimum age were 22 yrs and maximum age were 76 yrs. Mean of age were 50.15yrs. standard deviation of age were 14.43.
• In this study maximum number of liver SOL is found 51-60yrs age group (27.5%).
• Male are commonly affected than female. Out of 40 patients 28(70%) patients were male and 12(30%) patients were female.
• Among the total patients 34(85%) patients were
Hindu and 6(15%) patients were Muslim. Among 40 patients 13(32.5%) had metastatic adeno carcinaoma, 8(20%) patients had amoebic liver abscess, 6(15%) patients had pyogenic abscess, 4(10%)patients had haemangioma, 3(7.5%) patients had hepatocellular carcinoma. 2(5%) patients had simple cyst, 1(2.5%) patient had adenoma, 1(2.5%) patient had focal nodular hyperplasia. 1(2.5%) patient had hydatid cyst, 1(2.5%) had metastatic neuro-endocrine carcinoma. A study by Dr. Syed Mehdi Raza Rizvi, Allied Hospital, Faisalabad(7) revealed that primary liver malignancy were 61.6%, metastatic liver malignancy were 16.7%, liver abscess were 8.3%, focal nodular hyperplasia were 5%, simple cyst were 5%, hemangiomas were 3.3% out of 120 patients. In comparison to this study, it has been seen that in our study metastatic adenocarcinoma and liver abscesses occurring more frequently. This difference may be due to difference in number of patients studied. In this study, maximum number of liver SOL is found metastatic adenocarcinoma. Out of 13 metastatic adenocarcinoma patients, 4(30.76%) patients’ primary sources were in Lung. Colon and cholangiocarcinoma was primary sources in 2(15.38%) patients each. After thorough investigation as per protocol, primary sources of metastatic adenocarcinoma of liver were unknown in 3(23.07%) patients. Among 13 patients of metastatic adenocarcinoma of liver, male patients were 10(76.92%) and female patients were 3(23.08%).
• Out of 40 patients 6(15%) patients had pyogenic abscess. Single abscess is found in 2(33.3%) patient and multiple abscesses are found in 4(67.7%) patients. Among 6 patients 4(66.67%) patients are associated with diabetes mellitus and 2(33.3%) patients are associated with cholangitis. No organism identified in 2(33.33%) patients out of 6 patient of pyogenic abscess by culturing blood and pus from abscess. These may be due to antibiotic therapy started before arriving hospital. Out of 6 patients of pyogenic liver abscess organism identified were klebsiella pneumonia in 2(33.33%) patients, E.coli and Staphylococcus aureus was found in 1(16.66%) patient each. The study showed, in pyogenic abscess associated with Diabetes mellitus most commonly identified Organism was Klebsiella pneumonia. Out of 6 patients of pyogenic liver abscess 4(67.7%) patients were male and 2(33.3%) patients were female. Among 40 patients 8(20%) patients had amoebic abscess. Out of 8 patients 7(87.5%) patients were male and 1(12.5%) was female. Single abscess was found in 6(75%) patients and multiple amoebic abscesses are found in 2(25%) patient. In contrast to pyogenic abscess, amoebic abscess occur commonly single in number. All patients improved with anti-amoebic drug therapy. Therapeutic aspiration and surgical drainage were not needed as most of the lesion in right lobe and size of abscess in all patients were less than 5cm.
• Out of 40 patient’s hepatocellular carcinoma were found in 3(7.5%) patients. Hepatitis B positive patients were 1(33.33%) and hepatitis C positive patient were 2(66.67%). Out of 3 patients of hepatocellular carcinoma 2(66.67%) were alcoholic. In contrast to other study it is seen that hepatitis C associated hepatocellular carcinoma occurring more commonly than hepatitis B associated hepatocellular carcinoma.
• Hemangioma was found 4(10%) patients out of 40 patients. Among 4 patient of hemangioma 3(75%) patients were male and 1(25%) was female. Size of hemangioma was less than 4cm in all 4 patients. In contrast to other study it is seen that hemangioma occurring more common in male.
• In this study adenoma and focal nodular hyperplasia was found in 1(2.5%) patient each out of 40 patients. These two female patients were taking OCP for long duration.
B. Follow-up
Hepatocellular carcinoma and metastatic carcinoma all were treated conservatively and referred to surgery and oncology department. Hydatid cyst case were treated with albendazole and referred to surgery. Liver abscesses and benign liver SOL were followed up in medicine department. These patients were followed up at 1, 2, 4 and 6 months interval with complete blood count, liver function test and USG. Patients of Focal nodular hyperplasia, heamangioma, adenoma and simple cyst were asymptomatic.
Pyogenic abscess: Among 6 patients of pyogenic abscess 4 patients responded with broad spectrum antibiotic therapy and 2 patients responded with broad spectrum antibiotic and therapeutic aspiration. Clinically all patients were improved within 2-3weeks treatment but sonologically resolution of abscess delayed. Sonologically after one month 1(16.67%) patient had complete resolution of abscess cavity and 5 (83.33%) had residual abscess cavity. In 4 month 4(66.67%) patients had complete resolution of abscess cavity and 2(33.33%) patients had residual abscess cavity. .In 6month 5 (83.33%) patients had complete resolution of abscess cavity and 1(16.67%) patient had residual abscess cavity.
A study by K.C.S Sharma D (8) reveals that majority of pyogenic abscess resolved sonologically after 2-18 wks. In our study too majority of abscess resolved within 6month.
Amoebic abscess: All patients of amoebic abscess responded with antiamoebic drugs. They did not require therapeutic aspiration and surgical drainage. Clinically all patients improved within 6-10 days with anti-amoebic drug therapy but sonologically resolution of abscess were delayed. In 6month 3(37.5%) patients had complete resolution of abscess cavity and 5(62.5%) patient had residual abscess cavity In comparison to pyogenic abscess it was seen that complete resolution of abscess cavity delayed in amoebic abscess. A study by Sheen IS, Chien CS, Lin DY, Liaw YF (9) in Chang Gung Memorial Hospital, Taipei, Taiwan shown that pyogenic liver abscesses resolve more rapidly than amoebic abscess. This result is similar with our study.
CONCLUSION
In this study, majority of liver SOL were metastatic carcinoma of liver. Next common SOL is liver abscess. Amoebic liver abscess is more common than pyogenic liver abscess. Liver SOL has various etiology and risk factor. Most of the liver SOL occurs in older age group. Most of them have male preponderance except adenoma, focal nodular hyperplasia. Some of the liver SOL (hemangioma, simple cyst, adenoma, and focal nodular hyperplasia) may be asymptomatic. Majority of liver abscess responded with antibiotics. Clinical response is followed many months later by radiological resolution of abscess.
ACKNOWLEDGEMENT
The authors are grateful to the participants who voluntarily took part in the study. We wish to acknowledge the support provided by the Department of General Medicine, Nil Ratan Sircar Medical College, Kolkata for encouraging research and its publication. Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/ publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Nagorney DM: Benign hepatic tumors: Focal nodular hyperplasia and hepatocellular adenoma. World J Surg 1995; 19:13-18.
2. Ross D, Pina J, Mirza M, et al: Regression of focal nodular hyperplasia after discontinuation of oral contraceptives [letter]. Ann Intern Med 1976; 85:203-4.
3. Mathieu D, Kobeiter H, Maison P, et al: Oral contraceptive use and focal nodular hyperplasia of the liver. Gastroenterology 2000; 118:560-4.
4. Czermak BV, Akhan O, Hiemetzberger R, et al: Echinococcosis of the liver. Abdominal Imaging 2008; 33:133-43.
5. Pickren JW, Tsukada Y, Lane WW: Liver metastasis: Analysis of autopsy data. In: Weiss L, Gilber HA, ed. Liver Metastases, Boston: CK Hall; 1982:2-18.
6. Rockey DC: Hepatobiliary infections. Curr Opin Gastroenterol 2001; 17:257-61.
7. Syed MRR, Nasir I, M Azhar N, M Asif R:Evaluation of liver masses on CT scan: Professional med. journal. sep 2006 13(3) 431-434.
8. European Journal of Radiology. 2010 Apr; 74(1):195-8. doi: 10.1016/j.ejrad.2009.01.017. E.Pub 2009 Feb 12.
9. Sheen IS, Chien CS, Lin DY, Liaw YF: Resolution of liver abscesses: comparison of pyogenic and amebic liver abscesses. Am j tropical med hyg 1989 Apr,40(4); 384-9.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License