IJCRR - 7(2), January, 2015
Pages: 74-77
Print Article
Download XML Download PDF
PRIMARY BULLOUS LUNG DISEASE - A CASE REPORT
Author: Vishnukanth Govindaraj, Venkateswara Babu Ranganathan, Venkatesh Couppoussamy, Jayashalini Jayabalan, Madhumidha Bhaskaran, Gokulavasanth Balakrishnan
Category: Healthcare
Abstract:Bullae are thinwalled air-containing space within the lung parenchyma. They are usually larger than 1 cm in diameter, and their walls are composed of attenuated and compressed lung parenchyma. (1) Presence of bulla in a background of smoking is usually attributed to chronic obstructive pulmonary disease and is termed bullous emphysema. Bullous lung disease is presence of bulla in an otherwise normal lung. We present a case of bullous lung disease in a sixty five year old man with a clinical presentation of pneumothorax. The confounding factor was presence of smoking. The diagnosis was established by high resolution computed tomography(HRCT) of the chest.
Keywords: Bullous lung disease, HRCT
Full Text:
INTRODUCTION
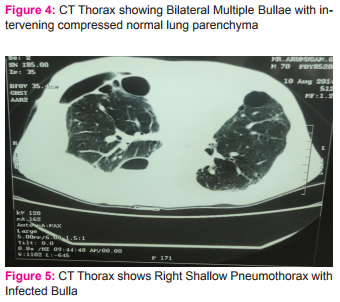
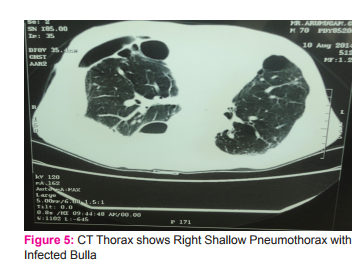
Presence of airspace opacity on chest x ray often is a diagnostic challenge to many a clinicians. Bulla, bleb and cyst are terms used to describe air filled opacity in the chest radiogram. These terms are often used interchangeably. Bleb is an intrapleural collection of air within the layers of visceral pleura. The source of air is usually a ruptured alveolus. Bulla is an air filled space within the lung parenchyma resulting from destruction of alveolar tissue. Cysts are thin-walled, air- or fluid-filled space with a wall that contains respiratory epithelium, cartilage, smooth muscle and glands. (1, 2) Bulla (pleural- bullae) can develop in a lung with underlying normal parenchyma. But most often it develops in a background of chronic obstructive lung disease. The former is termed as bullous lung disease and the latter as bullous emphysema. Bullous lung disease accounts for 20% of bullae and is less commonly mentioned in the differential diagnosis of an air filled space, mostly overshadowed by bullous emphysema.(1) We present a case of bullous lung disease in a sixty five year old man with a clinical presentation of pneumothorax. The confounding factor was presence of smoking. The diagnosis was established by high resolution computed tomography (HRCT) of the chest. CASE SCENARIO A sixty five old agricultural labourer presented with complaints of progressively worsening breathlessness and cough with minimal expectoration of six months duration. He developed sudden onset of right sided chest pain three days prior to presentation. He had no past history of tuberculosis and had no co morbid illness. He was an occasional smoker of thirty years. On presentation he was dyspneic and mildly tachypneic. General physical examination was unremarkable. His room air saturation was 84%. Blood pressure was 110/70 mm Hg, respiratory rate was 26breaths/ min and heart rate was 90 beats/ min. Respiratory system proper examination revealed a central trachea with diminished movements on the right side. Tactile vocal fremitus was diminished in the right infraclavicular, mammary, infra axillary and infra scapular region. There was a hyperresonant note and absent breath sounds in the same areas. A possibilty of secondary spontaneous pneumothorax in a background of chronic obstructive pulmonary disease was considered and he was subjected to chest radiogram. Chest x ray revealed a partial pneumothorax on the right side with hyperlucent opacity in the left upper zone. There was no hyperinflation in the chest radiogram.(fig 1) An intercostal chest tube(ICT) was placed on the right side.(fig 2,3) Post intercostal tube insertion the right lung expanded. There was a minimal airleakage and minimal subcutaneous emphysema around the ICT side. Though there was a complete expansion of the pneumothorax, he continued to be tachypneic. Arterial blood gas analysis (ABG) showed a persistent hypoxia with a normal carbon dioxide levels. Patient was subjected to a high resolution computed tomography (HRCT) scan of the chest. HRCT chest revealed multiple bullae bilaterally with intervening normal lung parenchyma.(fig 4,5) There was no evidence of pan acinar or paraseptal emphysema. Echo cardiogram showed no evidence of pulmonary hypertension. Taking into consideration his chest x ray which showed no evidence of hyperinflation, his persistent hypoxic status with normal carbon di oxide tension in ABG, his HRCT picture of bilateral bullae with intervening normal lung parenchyma, a possibility of primary bullous lung disease was considered. His alpha one antitrypsin levels were within normal limits. Patient underwent pleurodiesis on the right side with tetracycline. He was advised for domiciliary oxygen therapy and advised to restrain from performing strenuous physical activity. Patient is currently on home oxygen cylinder therapy and has not worsened till the last contact.
DISCUSSION
Bulla refers to an air-filled space that may be subpleural or intrapulmonary in location, with a diameter more than 1cm and a wall less than 1mm thick. Bulla commonly develops in persons with underlying chronic obstructive lung disease. Bullous emphysema refers to development of bulla in patients of chronic obstructive pulmonary disease. Bullous lung disease refers to presence of bulla in an apparently normal lung parenchyma. Cocaine smoking, Pulmonary Sarcoidosis, α1-antitrypsin deficiency, 1-antichymotrypsin deficiency, Marfan’s syndrome, Ehlers-Danlos syndrome , exposure to inhaled fiberglass have all been implicated in the development of bulla.(3,4,5) Bullae are classified anatomically into three main types. Type I bullae are characterized by a narrow neck that connects the bullae with the pulmonary parenchyma. They are usually found at the lung apices andalong the edges of the lingula and middle lobes and often occur in association with paraseptal emphysema. Type II bullae arise from the subpleural parenchyma and are characterized by a neck of panacinar emphysematous lung tissue. Type II bullae are most frequent in the upper lobe, at the anterior surface of the middle lobe, and over the diaphragm.Type III bullae consist of slightly hyperinflated lung connected to the rest of the lung by a broad base extending deep into the parenchyma. This type is believed to represent an atrophic form of emphysema (1, 6).Various hypothesis are put forth for the development of bulla but none of them are conclusive. The clinical presentation of bullous lung disease depends on the extent of bulla and their size and number. Occasionally bulla can enlarge and encompass more than one-third of the lung volume leading to compression of adjacent normal lung tissue. Giant bullous emphysema or vanishing lung syndrome (7, 8) is mainly seen in young men with history of tobacco smoking and Marijuana use and is characterized by the presence of large progressive bullae that occupy a significant volume of a hemithorax and are often asymmetrical. Patients with bullous lung disease may be asymptomatic and bulla may be incidentally detected on routine chest radiography. Symptomatic patients may complain of progressive dyspnea or chest paindue to gradual increase in the size of the bullae (9). Sudden onset of severe chest pain or sudden worsening of breathlessness may be due to air trapping in bulla or a spontaneous pneumothorax secondary to rupture of bulla. Increase in cough with sputum production usually indicates infection in a bulla. Young patients with large bullae are predisposed to lung cancers. Dystrophic changes caused by bulla in the adjacent lung parenchyma due to compression and the presence of scar tissue that predispose to development of bulla may be the reason for increased incidence of lung cancer in these patients. Poor ventilation of the bullae may lead to accumulation of carcinogens in them(10, 11). The clinical findings in patients of bullous lung disease are variable. Giant bullae may clinically mimic a pneumothorax with the presence of diminished breathsounds and increased resonance on percussion. Fever, purulent expectoration may occur when bulla is secondarily infected. Radiological features of bulla: Bulla is often suspected radiologically and is mostly an incidental finding. An area of hyperlucency with presence of thin hairline shadows may be an identifying feature. However, occasionally it is difficult to differentiate the hairline shadows produced by a bulla from irregular walls of a cavity or cysts in the lung parenchyma. A forced expiratory film may be needed to confirm the presence of bulla. Bulla tends to trap air and during a forced expiratory maneuver their outline becomes more accentuated as the surrounding normal parenchyma shrinks. Large bulla may sometimes displace the mediastinum contralaterally and may even compress the opposite lung. Ultrasound imaging helps to differentiate between a pneumothorax and bulla. A typical ‘comet tailing’ phenomenon of the movement of the lung tissue againstthe pleura during respiration can be seen in bullous disease, but is absent in pneumothorax.(12) Computed tomography study of the thorax is perhaps the best method for identifying bulla. A bulla is identified as area of transradiancy that usually do not contain blood vessels and is confined by visible walls. The complications of bulla like pneumothorax, secondary infection can be better detected with CT. (13) The double wall sign is a valuable sign to help distinguish a pneumothorax from adjacent giant bulla (14). Double wall sign is presence of air outlining both the sides of the bulla wall parallel to the chest wall. Treatment of bulla depends on the symptomatology of the patient, the extent of the disease, presence of coexisting illness. Bulla that cause few respiratory symptoms are treated conservatively. Patient is advised to quit smoking, avoid physical activities or exercise that may promote the rupture of bulla. Scuba diving are better avoided. An annual chest radiograph evaluation may be advised. Infection of a bulla is treated by antibiotics and chest physiotherapy. Surgical treatment of bulla allows normal but compressed lung parenchyma to expand.Surgical removal of bulla is needed when there is a progressive increase in bulla size, recurrent pneumothorax due to rupture of bulla, giant bulla causing respiratory insufficiency due to compression of adjacent lung and recurrent infection. Bullectomy or resection of the entire bulla, either through a video assisted thoracoscopic surgery (VATS) or a standard open thoracotomy, is the most common surgical technique used for treatment Total pneumonectomy is indicated in those withsevere unilateral bullae with essentially no functioning lung.(16,17,18)
CONCLUSION
It is not uncommon to attribute all cases of bulla to chronic obstructive pulmonary disease and name them as bullous emphysema. Our patient was an occasional smoker and in the presence of bulla on chest x ray one would have been tempted to treat him as bullous emphysema. The treatment for bullous lung disease and bullous emphysema are different. Our case also highlights the need for evaluation with a HRCT scan in patients with suspected bulla in chest x ray.
ACKNOWLEDGEMENT
S Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. The authors have received no funding for this work. The authors assure that there is no conflict of interest .
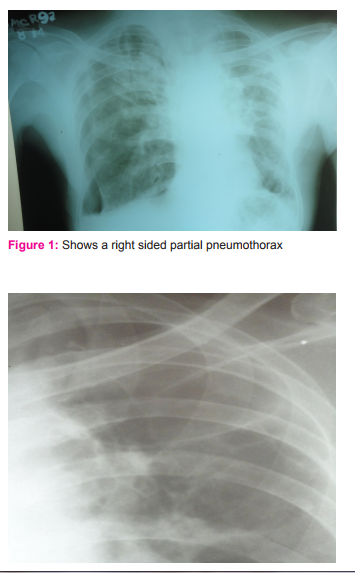
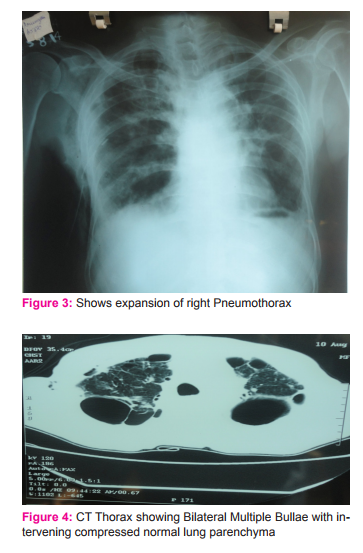
Figure 2: Presence of a bulla in the left upper zone
References:
1. Robert R.Klingman, Vito A.Angelellio, Tom R.Demesseter. Cystic and bullous lung disease. Ann Thoracsurg 1991; 52: 576-580.
2. David M.F.Murphy,AlfredP.Fishman- Fishman’s textbook of pulmonary diseases and disorders The Mcgraw Hill company- fourth ed. Pg-913-915.
3. NidhiSood and Nikhil Sood. A rare case of vanishing lung syndrome.Case Reports in Pulmonology volume 2011, Article ID 957463.
4. S.W. Hii, J. D. C. Tam, B. R. Thompson, and M. T. Naughton,“Bullous lung disease due to marijuana,” Respirology, vol. 13, no. 1, pp. 122–127, 2008.
5. M. Beshay, H. Kaiser, D. Niedhart, M. A. Reymond, and R. A. Schmid, “Emphysema and secondary pneumothorax in young adults smoking cannabis.European Journal of Cardio-thoracic Surgery, vol. 32, no.
6, pp. 834–838, 2007. 6. R.S Fraser, P.D.Pare- diagnosis of diseases of the chest W.B Saunder’s company . Fourth ed Pg-2234-2235.
7. Nidhi Sharma, AlMamoonJustaniah, Jeffrey P. Kanne et al Vanishing Lung Syndrome (Giant Bullous Emphysema): CT Findings in 7 Patients and a Literature Review. J Thorac Imaging 2009;24:227–230).
8. N. N. Shah, R. Bhargava, Z. Ahmed, D.K. Pandey et al unilateral bullous emphysema of lung. Lung India 2007; 24 : 30-32.
9. Boushy SF, Kohen R, Billing DM, Heiman MJ. Bullous emphysema: clinical, roentgenologic and physiologic study of 49 patients. Dis Chest 1968; 54: 327-34. 10. Arongerg DJ, Sagel SS, LeFrak S, Kuhn C, Susman N. Lung carcinoma associated with bullous lung disease in young men. AJR Am J Roentgenol 1980;134:249-52. 11. Goldstein MJ, Snider GL, Liberson M et al. Bronchogenic carcinoma and giant bullous disease. Am Rev Respir Dis 1968; 97:1062-70.
12. Simon BC, Paolinetti L. Two cases where bedside ultrasound was able to distinguish pulmonary bleb from pneumothorax.J Emerg Med. 2005.29:201-5.
13. Phillips GD, Trotman-Dickensen B, Hodson ME, Geddes DM. Role of CT in the management of pneumothorax in patients with complex cystic lung disease. Chest 1997; 112: 275-8.
14. Gayle M. Waitches,Eric J. Stern,Theodore J. Dubinsky Usefulness of the Double-Wall Sign in Detecting Pneumothorax in Patients with Giant Bullous Emphysema AJR 2000;174:1765–1768.
15. Mehran RJ, Deslauriers J. Indications for surgery and patient work-up for bullectomy.ChestSurgClin N Am 1995; 5: 717-34.
16. Greenberg AJ, Singhal S, Kaiser LR Giant bullous lung disease: evaluation, selection, techniques, and outcomes. Chest SurgClin N Am. 2003 Nov;13(4):631-49.
17. Grayson Wheatley III, Aaron Estrera. Bullous Lung Disease. the cardiothoracic surgery network .www.ctsnet.org. published on aug 30, 2010. Accessed on 19.11.14.
18. Yasir Ahmad Lone, Abdul MajeedDar,MukandLal Sharma et al Outcome of the Surgical Treatment of Bullous Lung Disease: A Prospective Study. Tanaffos2012; 11(2): 27-33.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License