IJCRR - 7(2), January, 2015
Pages: 69-73
Print Article
Download XML Download PDF
A RARE CASE OF DIFFUSE NEUROFIBROMA - A CASE REPORT
Author: Ramkumar G., Sudha V., Subbiah S., Karthi Sundar V., Jasmine Deva Arulselvi
Category: Healthcare
Abstract:Diffuse neurofibroma is the rarest form of neurofibroma which is more common among children and young adults.The lesions are ill defined and infiltrative in nature and usually affects the skin and subcutaneous tissue.We present a case of 10 year old boy whose initial clinical and radiological evaluation did not reveal the diagnosis and it was only after the histopathological study we concluded the case as neurofibroma
Keywords: Diffuse neurofibroma, Café au lait patches, Spindle cells, Meissners corpuscles
Full Text:
INTRODUCTION
Neurofibroma is a benign nerve sheath tumour of the peripheral nervous system.It has three distinct types namely localized, diffuse and plexiform type.This case report is of a patient who presented with diffuse neurofibroma, which is also the rarest form. The aim of presenting this case of diffuse neurofibroma is to emphasize the importance of clinical and histopathological examination in its diagnosis. Also, this condition when detected early can be monitored on a periodic basis to detect complications of the same and improve patient outcome.
CASE REPORT
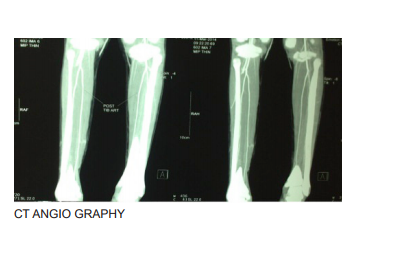
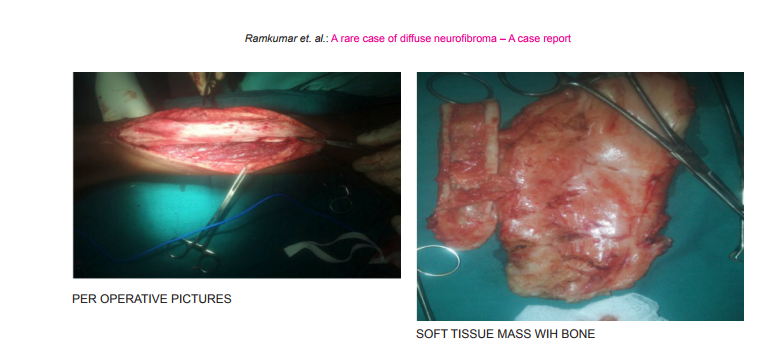
A 10 year old boy presented with swelling in the right leg for seven years.The swelling was initially small and gradually got bigger to attain the present size.There was pain for two days after being hit over the swelling while playing.There was no history of bleeding or discharge from the swelling.There was no history of fever or other similar swelling elsewhere. It was interesting to note that over the past seven years patient has been thorughly investigated for recurrent pain in his leg.In 2010, patient underwent medial epiphysiodesis of right ankle for calcaneo valgus deformity correction in a government hospital. CT and MRI taken in a private hospital showed periosteal based lesion along the tibial diaphysis possibly sub periosteal hematoma or sub periosteal abscess. The patient continued to have pain inspite of an extended treatment for infection.A repeat MRI in 2012 showed small resolving abscess with haemorrhagic contents.No other new clinical finding was noted that time. On this occasion, the general condition was fair. The swelling on the right leg was 15x7cms on the anterolateral aspect extending from 3cms below the knee to 4cms above the medial malleolus.The swelling was not warm and non tender.The surface was smooth and firm in consistency.It was not mobileand fixed to the underlying bone. There was no scars and no dilated or engorged veins. There was limb lengthening which measured 2cms. The limb girth on the right side was 3cms more than theleft. There was full range of movements at both the knee and ankle joints.Examination did not reveal any neuro vascular deficit. Routine blood investigations were normal.X-ray of the leg showed sclerosis,periosteal thickening, anterolateral bowing and deformity of the bone.CT angiography revealed residual hematoma probabaly infective in aetiology. Excision biopsy was planned.Per-operatively, a soft tissue mass was found and was sent for histopathological examination along with a piece of bone. Histopathological examination of the soft tissue mass showed a neoplasm composed of elongated, spindleshaped cells with wavy, buckled nuclei and (Fig A,C) some with oval nuclei arranged in a haphazard fashion (Fig B) entrapping lobules of mature adipose tissue and skeletal muscle fibres.Some areas show differentiation towards Meissner type of tactile corpuscles and scattered ectatic blood vessels were also seen (Fig D). Neurofibromatous tissues show immunoreactivity with S-100 protein (Fig E,F). It is a sensitive, but non-specific marker of benign nerve sheath tumors.1 Sections from the bone showed normal mature lamellated bone.(Fig G)Based on these findings, it was reported as diffuse neurofibroma. Following the tissue diagnosis,the patient was examined retrospectively for café au lait patches and multiple café au lait spots were seen over the trunk. (Fig H) .An ophthalmology opinion was sought to detect Lisch nodules which was however absent.CT brain and trunk showed no abnormalities.The post operativecourse was uneventful. DISCUSSION Neurofibromas are benign nerve sheath tumors in the peripheral nervous system, which frequently occur as a part of Neurofibromatosis 1.Neurofibromatosis is a genetic disorder that may be associated with multiple neurofibromas. They arise from the non myelinating type of Schwann cells that exhibit biallelic inactivation of the NF1 gene that codes for the protein neurofibromin.Neurofibromas are classically described as localized, diffuse, and plexiform types2 depending on the growth pattern. Localized and plexiform neurofibromas are well known subtypes. The localized form is the most common and they usually present as skin-colored dome-shaped or pedunculated papules that display the pathognomonic “buttonhole” sign. They can be sporadic or Neurofibromatosis associated. Plexiform neurofibromas are larger and more extensive tumors that are usually associated with Neurofibromatosis. Diffuse neurofibroma is an uncommon but distinctive subtype of neurofibroma.They are usually solitary lesions and are progressively enlarging and infiltrating type, simulating malignant tumors.They occur most commonly among children and young adults. They typically involvethe skin and subcutaneous tissues of the head and neck3,4,5 . Trunk and extremities are also commonly involved and constitute more than one third of the lesions.6 They are poorly defined lesions that spreads extensively along connective tissue septa and between fat cells.They surround rather than destroy adjacent normal structures 3,4,5. This lesion has also been termed “paraneurofibroma” as the tumor extends beyond the confines of the perineurium 7 . They differ from conventional neurofibromas by the presence of uniform matrix of fine fibrillary collagen , less elongated schwann cells and clusters of meissner body-like structures which are the characteristic feature of this lesion. The incidence of neurofibromatosis among patients with diffuseneurofibroma has been reported to be approximately 10% 4 .For the diagnosis of Neurofibromatosistype 1, two or more of the cardinalsignsare required:
• 6 or more brownish discolorations on the skin, more than 5mm in diameter in pre-adolescents and greater than 15 mm in adolescents and adults.
• 2 or more neurofibromas.
• Freckling in the axilla or groin.
• Optic glioma
• 2 or more Lisch nodules, or small masses on the iris.
• Bone lesions like sphenoid dysplasia.
• A first degree relative with Neurofibromatosis 1.
In our case , as solitary neurofibroma and multiple café au lait spots are present there is a high potency for the development of Neurofibromatosis I. 8 Malignant transformation rarely occurs in solitary diffuse neurofibromas9 . Pain or enlargement of a neurofibroma may herald malignant transformation.Surgical excision is not mandatory as malignant transformation is rare 2 .Resection is performed when the tumor is severely disfiguring or severely compromises function 10. Partial or complete surgical excision is done for large neurofibromas. The extensive and infiltrative nature of the lesions precludes complete surgical resection.2,3,10Recurrence may develop even after complete excision because of it’s infiltrative growth pattern in Diffuse neurofibroma. As there is a relatively high incidence of recurrence and the potential development of neurofibromatosis, yearly follow-up is warrented.3,7,10.
CONCLUSION
Most often neurofibromas are of histopathological diagnosis especially in solitary lesions because of the indefinite clinical characteristics. Relevant history taking, clinical examination and ophthalmic and radiological investigations are needed for thepreoperative suspicion. In order to exclude neurofibromatosis, special attention is needed for the detection of café au lait spots.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.

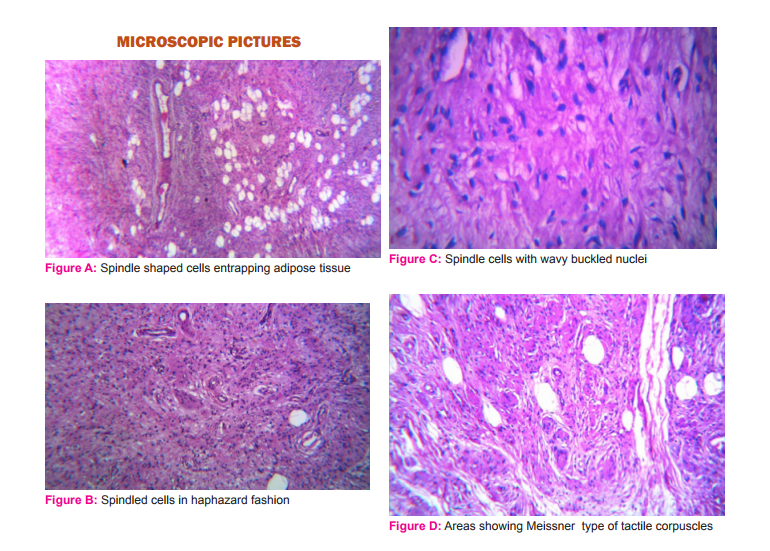

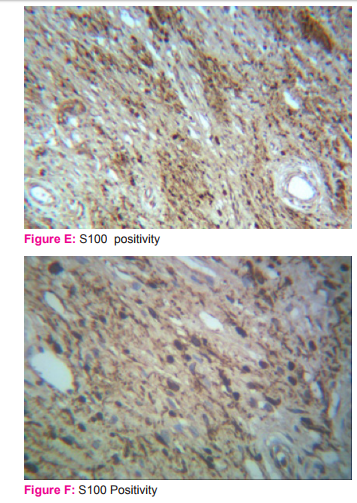

E,F -S 100 Positivity G - Normal mature bone

References:
1. Ito H, Akagi O, Nomura N, Tahara E. Giant pigmented tumour of the scalp--a diffuse neurofibroma or a congenital naevus showing neurofibromatous changes? Immunohistochemical and electron microscopic studies. Histopathology. 1988;13:181–189.
2. Coakley D, Atlas MD. Diffuse neurofibroma obstructing the external auditory meatus. J Laryngol Otol 1997; 111:145– 147
3. Van Zuuren EJ, Posma AN. Diffuse neurofibroma on the lower back. J Am Acad Dermatol 2003; 48:938–940
4. Weiss SW, Goldblum JR. Benign tumors of peripheral nerves. In: Enzinger and Weiss’s soft tissue tumors, 4th ed. St. Louis, MO: Mosby, 2001:1132 –1140
5. Kransdorf MJ, Murphey MD. Neurogenic tumors. In: Imaging of soft tissue tumors, 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2006:334 –338
6. Hassell DS, Bancroft LW, Kransdorf MJ, Peterson JJ, Berquist TH, Murphey MD, et al. Imaging Appearance of Diffuse Neurofibroma. AJR Am J Roentgenol. 2008;190:582- 8.
7. Daoud MS, Pittelkow MR. Lichen planus. In: Freedbersg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick’s dermatology in general medicine. 6th ed. New York: McGraw-Hill; 2003. pp. 463–477.
8. Whitehouse D: Diagnostic value of the café au lait spot in children. Arch Dis child 1996; 41: 316-31
9. Beggs I, Gilmour HM, Davie RM. Diffuse neurofibroma of the ankle. Clin Radiol. 1998;53:755–759.
10. Ergun SS, Emel E, Karabekir S, Buyukbabani N. Extracranial diffuse neurofibroma with intracranial extension. Plast Reconstr Surg. 2000;105:801–803
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License