IJCRR - 7(6), March, 2015
Pages: 44-46
Print Article
Download XML Download PDF
ANAESTHESIA FOR ABDOMINO - PERINEAL RESECTION IN A PATIENT WITH PREVIOUS PARALYTIC POLIOMYELITIS
Author: Pratibha S. D., Shivanand L. K., Renuka H.
Category: Healthcare
Abstract:Poliomyelitis (also called infantile paralysis or acute anterior poliomyelitis) is an acute viral infectious disease that can present in two forms: asymptomatic infection or paralytic disease. A 45year old man, ASA(American society of anaesthesiologist) physical status II, 168cm tall and weighing 66kg was scheduled for Abdomino-perineal resection for Carcinoma - rectum. Medical history included paralytic poliomyelitis since childhood with hypoplastic lower limbs and kyphoscoliosis. General anesthesia was planned as patient refused for regional technique. General anaesthesia was effectively performed for polio patients with kyphoscoliosis by meticulous neuromuscular monitoring and titrated dose of drugs.
Keywords: Poliomyelitis, Kyphoscoliosis, General anaesthesia, Neuromascular monitoring
Full Text:
INTRODUCTION
Post polio syndrome1 is a disorder related to the recurrence of neuromuscular symptoms in survivors of paralytic poliomyelitis. Poliomyelitis (also called infantile paralysis or acute anterior poliomyelitis) is an acute viral infectious disease that can present in two forms: asymptomatic infection or paralytic disease. Paralytic disease2 is characterized by the sudden onset of flaccid paralysis associated with fever. It usually affects the lower limbs causing muscular weakness which results in reduction or loss of neurological reflexes. sensory system will be intact. Poliovirus damages the reticular activating system, many anesthetic drugs have action on this site . This may account for the extreme sensitivity these patients demonstrate to anesthetic medications as well as to the increased potential for delayed awakenings and other postoperative complications. Therefore it is of utmost importance to be careful about pharmacologic dosing of opioids and neuromuscular agents. Perioperative and postoperative issues related to aspiration risk, cold intolerance and positioning need timely intervention. CASE REPORT A 45year old man, ASA(American society of anaesthesiologist) physical status II, 168cm tall and weighing 66kg was scheduled for Abdomino-perineal resection for Carcinoma - rectum. His medical history included paralytic poliomyelitis since childhood with hypoplastic lower limbs and kyphoscoliosis, but did not include respiratory insufficiency necessitating assistive devices.
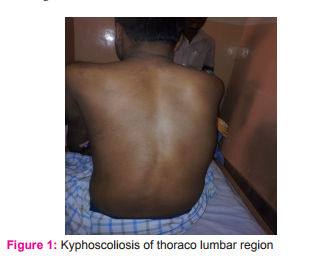
Preoperative blood pressure was 136/68 mm Hg, pulse was 86/min, respiratory rate was 14/min, temperature was 37.2°Cand oxygen saturation was 100% on room air. Airway assessment demonstrated a Mallampati class II. Spine examination revealed kyphoscoliosis, with irregular intervertebral spaces. Serum electrolytes, blood sugar, urea, creatinine and complete blood cell count indices were all within normal limits. The chest radiograph did not show any acute disease but showed kyposcoliosis. His electrocardiogram(ECG) was within normal limits. Results of the physical examination revealed bilateral lower extremity muscle weakness, necessitating the use of a cane and leg braces. He denied any history related to deficiencies with the respiratory muscles, including difficulty with breathing, swallowing or sleep apnoea. Colonoscopy done and biopsy revealed adenocarcinoma –colon (moderately differentiated). General anesthesia was planned as patient refused for regional technique. Premedication IV was given with midazolam-1mg ,Glycopyrolate -0.2mg,Pantoprazole- 40mg,Ondansetron-4mg and fentanyl-100 µg. Monitors included NIBP(non invasive blood pressure), ECG, Pulse oxymetry, ETCO2 (end tidal carbon dioxide ) respiratory gas analyzer, temperature, urine output and neuromuscular monitor. Induced with inj propofol 100mg IV, Intubated with cuffed portex 8.5 No endotracheal tube with inj. Vecuronium 6 mg iv . Maintained with oxygen, nitrous oxide, isoflurane and inj vecuronium with neuromuscular monitoring to maintain surgical plane of anaesthesia. Measures to maintain temperature were taken. Surgery lasted for 5hours.

Figure 2: Neuromascular Monitoring
End of surgery TOF (train of four) ratio in NMM (Neuro muscular monitoring) -0.9. Reversed with glycopyrolate (0.5 mg iv) and neostigime (2.5 mg iv) . Patient was conscious oriented, responded to oral commands but was unable to lift the head for more than 5secs and had inadequate hand grip. Patient was put on t-piece 5lts oxygen and monitored for 4hrs and extubated once extubation criteria were met. Patient was shifted to intensive care unit for observation for 24 hours.
DISCUSSION
An estimated 60% of those who had paralytic poliomyelitis are affected by postpolio syndrome. Postpolio syndrome is diagnosed in patients with a history of paralytic polio who have had a neurologic recovery of at least 15 years, followed by a gradual or new onset of muscle weakness, pain or other neurological symptoms. The most common symptoms of postpolio syndrome are fatigue, muscle pain, respiratory difficulties, intolerance to cold and difficulty in swallowing. The choice of using a general anesthetic versus a regional anesthetic should be based on the preoperative assessment, surgery and patient consent3 . It is unknown whether the motor neurons of patients with postpolio syndrome are more vulnerable to the effects of local anesthetics and if these patients may be more sensitive to overall toxic concentrations. Up to 42% of patients with postpolio syndrome4 have respiratory muscle involvement ranging from laryngeal muscle weakness to vocal cord paralysis. Dysphagia is present in 10% to 20% of these patients. This should alert the anesthetist to the increased potential of postoperative apnea and aspiration. The careful titration of opioids and muscle relaxants is necessary because of the increased sensitivity to these medications. Depolarizing muscle relaxant poses potential risk of hyperkalemia, severe myalgia and prolonged duration of action5 . There is a potential of increased sensitivity to nondepolarizing neuromuscular agents, necessitating careful neuromuscular monitoring. Careful positioning is essential because of potential chronic pain. Patients typically have a profound cold intolerance. Care should include warming the ambient air of the operating room, using warming blankets and warming intravenous fluids as indicated as well as continued warming efforts in the postoperative period to avoid shivering.
CONCLUSION
General anaesthesia was effectively performed for polio patients with kyphoscoliosis by meticulous neuromuscular monitoring and titrated dose of drugs. The decision to perform regional anesthesia in patients with preexisting neurologic deficits should be based on the risks and potential benefits of each individual case.
Source of funding: None
Conflict of interest: Nil
ACKNOWELEDGMENT
Authors would like to thank BLDEU Medical college for giving an opportunity. They also extend their gratitude to their colleagues for continuous support for during the case. Authors also thanks all the authors of articles from which information is cited in this paper.
References:
1. Donna Wheeler, Anesthetic Considerations for Patients with Postpolio Syndrome: A Case Report; AANA Journal; October 2011;Vol. 79, No. 5; 408-410.
2. Lambert DA, Giannoulin E, Schmidt BJ. Postpolio syndrome and anesthesia. Anesthesiology. 2005;103(3):638-644.
3. Costello JF, Balki M. Cesarean delivery under ultrasoundguided spinal anesthesia [corrected] in a parturient with poliomyelitis and Harrington instrumentation. Can J Anesth. 2008;55(9):606-611.
4. Suneel PR, Sinha PK, Unnikrishnan KP, Abraham M. Anesthesia for craniotomy in a patient with previous paralytic polio. J Clin Anesth. 2008;20(3):210-213.
5. Cherng C. Uneventful use of succinylcholine in six patients with post-polio syndrome. Br J Anaesth Online. 2008;101(1).
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License