IJCRR - 7(8), April, 2015
Pages: 71-74
Print Article
Download XML Download PDF
BENIGN OVARIAN TUMOURS IN A TERTIARY CARE HOSPITAL IN NIGER DELTA, NIGERIA: A 10 YEAR HISTOPATHOLOGICAL STUDY
Author: Udoye Ezenwa Patrick, Kotingo Ebikabowei Lucky
Category: Healthcare
Abstract:Objectives: To determine the relative frequencies, types, subtypes and age distribution of Benign ovarian tumours and to compare the results with other local and international studies. Methodology: A 10 year retrospective analysis of Benign ovarian tumours diagnosed in the Anatomical Pathology Department of University of Port Harcourt Teaching Hospital from January 1998 to December 2007.
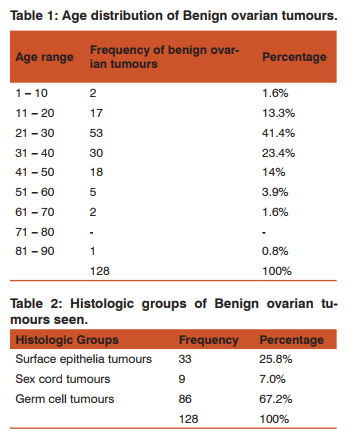
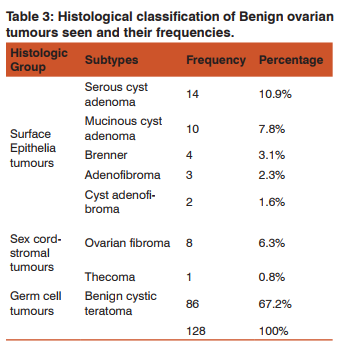
Results: Out of a total of 7529 surgical specimens received in the department within the study period, 166 (2.2%) were ovarian tumours. Of these 166 ovarian tumours, 128 (77.1%) were benign neoplasms. These 128 benign ovarian tumours formed 1.7% of the total surgical specimen received. The most common histological group was the germ cell tumours (67.2%), followed by surface epithelial tumours (25.8%) and sex cord-stromal tumours (7%). All the germ cell tumours seen were benign cystic teratoma, 86 (67.2%). The lowest age at which benign ovarian tumours occurred in this study was 4years while the highest age was 82years. Benign ovarian tumours peaked in the 21 \? 30 years age range, followed by 31- 40 years age range.
Conclusion: Ovarian tumours are more commonly benign in our environment with germ cell tumours being the most common histologic group unlike in Caucasians where surface epithelial tumours are more predominant. Benign cystic teratoma is very common in our locale unlike in Europe, North America and some parts of Asia where surface epithelial tumours are more common.
Keywords: Benign ovarian tumours, Cystic teratoma, Neoplasms, Histologic types
Full Text:
INTRODUCTION
The ovaries are female reproductive organs which are normally paired and located at both sides of the uterus, behind the broad ligaments and in front of the rectum1 . Each ovary is covered by a single layer of modified mesothelium known as surface, coelomic or germinal epithelium2 . All primary ovarian tumours tend to originate from one of the four structures that make up the composite ovarian organ notably the surface epithelial cells, the germ cells, the sex cords and the specialized ovarian stroma1,2. Interestingly, no other organ gives origin to a wide range of histogenetic tumours as the ovaries3,4. Benign cystic tumours of the ovaries are the fourth most common gynecological causes of hospital admissions5 . Worldwide figures show that about 80% of ovarian neoplasms are benign, occurring mostly in the 20 – 45 years age range2 . There is likelihood of increase in the incidence of ovarian tumours in the developing countries because of decreasing fertility rate and increasing use of ovulation induction drugs, among other factors, which thus calls for greater effort in the study of this tumour in these regions6 . No previous work has been done exclusively on the histopathological pattern of benign ovarian tumours in the University of Port Harcourt Teaching Hospital. In view of this and the need to have a comprehensive literature on ovarian tumours in Africa which will help us reappraise our dependence on western data, this study was carried out. The purpose of this study was to show the histopathologic pattern and age distribution of benign ovarian tumours and how they compared to results from other centres locally and outside Nigeria with the hope that this work would contribute to the literature on ovarian tumours in this country.
METHODOLOGY
This is a retrospective study based on histopathologically proven cases of benign ovarian neoplasms seen at the department of Anatomical Pathology of University of Port Harcourt Teaching Hospital over 10years. The original request forms and histopathology reports for all the ovarian neoplasms seen within the study period were retrieved and relevant clinical information and biodata were obtained. Clinical information and biodata unavailable on the request forms were obtained from the case files. The original slides of the entire benign neoplastic lesions were also retrieved and reviewed using the simplified version of W.H.O classification of ovarian tumours2 . Fresh sections of the missing slides were also taken from the tissue blocks and stained with Haematoxylin and Eosin, then reviewed. The results obtained were analyzed using simple descriptive statistical methods. Cases of benign ovarian tumours with incomplete biodata or those with missing slides and blocks were excluded. Ethical committee clearance: This study was duly approved by the ethics committee of the University of Port Harcourt
Teaching Hospital.
RESULTS
A total of 7529 surgical specimens were received in the department within the study period, 166 (2.2%) were ovarian tumours while 128 (1.7%) were benign ovarian neoplasms. Of these 166 ovarian neoplasms, 77.1% (128) were benign. The most common histologic group was the germ cell tumours which constituted 67.2% of all the benign ovarian tumours. Benign ovarian tumours were seen between the ages of 4years and 82years in this study and occurred mostly (41.4%) in the third decade (21 - 30years) followed by the fourth decade (31 - 40years) 23.4%. Frequencies for other age ranges are shown in Table 1. All the 86 germ cell tumours seen in this study were Benign cystic teratoma (BCT). BCT was also the most common histologic subtype of the benign ovarian tumours and occurred most in the 21- 30years age range. The surface epithelial tumours 25.8% were the second most common histologic group and were seen most in the 31- 40years age range. Serous cystadenomas (14) were the most common subtype of the surface epithelial tumours and also formed the second most common histologic subtype of all the benign ovarian tumours (10.9%). Other subtypes of surface epithelial tumours and their relative frequencies are also shown in Table 3. The sex cord-stromal tumours (9) were the least occurring histologic group of benign ovarian tumours forming only 7%. Eight out of the nine sex cord-stromal tumours were ovarian fibroma which occurred most in the 11 – 20 years age range.
DISCUSSION
In this study, benign ovarian tumours constituted 1.7% of the total surgical specimen received in the department over the study period, a figure which may suggest that these neoplasms are relatively uncommon in our locale.
Abbreviations
BCT: Benign cystic teratoma
W.H.O: World Health Organization
ACKNOWLEDGEMENTS
The authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. We also acknowledge Prof. S. O. Nwosu of the Department of Anatomical Pathology, University of Port Harcourt Teaching Hospital who supervised this work, a dissertation for the award of Fellowship of the National Postgraduate Medical College of Nigeria, 2011.
Source Of Funding No external source of funding.
Conflict Of Interest None declared.
References:
1. Rosai J. Ovary. In: Rosai and Ackerman’s Surgical Pathology. 9th ed. (Vol. 2). New Delhi: Mosby; 2004. p. 1649-709.
2. Ellenson LH, Pirog EC. The female genital tract. In: Kumar V, Abbas AK, Fausto N, Aster JC, editors. Robbins and Cotran Pathologic Basis of Disease 8th ed. Pennysylvania: Saunders; 2010. p. 1005-61.
3. Greenwald EF. Ovarian tumours. Clin Obstet Gynecol 1975; 18(4): 61-84.
4. Salzer H, Denison U, Breitenecker G, Speiser P, Obermair A. Ovarian carcinoma. ACO Manual 1993; 2: 5-7.
5. Yasmin S, Yasmin A, Asif M. Frequency of benign and malignant ovarian tumours in a tertiary care hospital. JPMI 2006; 20: 393-7.
6. Odukogbe AA, Adebamowo CA, Ola B, Olayemi O, Oladokun A, Adewale IF, et al. Ovarian cancer in Ibadan: characteristics and management. J Obstet Gynecol 2004; 24(3): 294-7.
7. Jibrin P. A ten year histopathological review of ovarian tumours in Calabar [dissertation]. National Postgraduate Medical College of Nigeria, 2001.
8. Akhiwu WO. Histopathological analysis of ovarian tumours seen in the University of Benin Teaching Hospital: A ten year retrospective study 1987-1996 [dissertation]. National Postgraduate Medical College of Nigeria, 1999.
9. Onyiaorah IV, Anunobi CC, Banjo AA, Abdulkareem AA, Nwankwo KC. Histopathological pattern of ovarian tumours seen in Lagos University Teaching Hospital: A ten year retrospective study. Nig Qt J Hosp Med 2011; 21(2): 114-8.
10. Doh AS, Shasha W. A clinicopathologic study of ovarian tumours in Yaoundé, Cameroun. West Afr J Med 1994; 13(4): 196-7.
11. Murthy DP. Ovarian tumours in Papua, New Guinea: relative frequency and histological features. PNG Med J 1985; 28(1): 14-22.
12. Gatphoh ED, Darnal HK. Ovarian neoplasm in Manipur. J Indian Med Assoc 1990; 88(12): 338-9.
13. Pilli GS, Suneeta KP, Dhaded AV, Venni VV. Ovarian tunours: a study of 282 cases. J Indian med Assoc 2002; 100(7): 420, 423-4, 447.
14. Katchy KC, Briggs ND. Clinical and pathological features of ovarian tumours in Rivers State of Nigeria. East Afr Med J 1992; 69(8): 45-9.
15. Lancaster EJ, Muthuphei MN. Ovarian tumours in Africa: a study of 512 cases. Cent Afr J Med 1995; 41(8): 245-8.
16. Briggs ND, Katchy KC. Pattern of primary gynecological malignancies as seen in a tertiary hospital situated in the Rivers State of Nigeria. Int J Gynecol Obstet 1990; 31: 157- 61.
17. Baker TR, Piver MS. Etiology, biology and epidermiology of ovarian tumour. Semin Surg Oncol 1994; 10: 224-6.
18. Babarinsa IA, Akang EEU, Adewale IF. Pattern of Gynecological malignancies at the Ibadan cancer registry (1976- 1995). Nig Qt J Hosp Med 1998; 8(2): 103-5.
19. Moller H, Evans H. Epidemiology of gonadal germ cell cancer in males and females. APMIS 2003; 111(1): 43-6. Discussion 46-8.
20. Ahmad Z, Kayani N, Hasan SH, Muzafar S, Gill MS. Histological pattern of ovarian neoplasm. J Pak Med Assoc 2000; 50(12): 416-9.
21. Bukhari U, Memon Q, Memon H. Frequency and pattern of ovarian tumours. Pak J Med Sci 2011; 27(4): 884-6.
22. Sharma I, Sarma U. Dutta UC. Pathology of ovarian tumour: a hospital based study. Valley Int J 2014; 1(6): 284- 6.
23. Mabogunje OA, Nirodi NS, Harrison KA, Edington GM. Teratomas in adult Nigerians. Afr J Med Med Sci 1980; 9(3-4): 151-8.
24. Akang EE, Odunfa AO, Aghadiuno PU. A review of teratomas in Ibadan. Afr J Med Med Sci 1994; 23(1):53-6.
25. Di Bonito L, Patriarca S, Delenchi M, Alberico S. Ovarian tumours: anatomohistopathological contribution to their interpretation. Eur J Gynecol Oncol 1988; 9(4): 324-30.
26. Junaid TA. Ovarian neoplasms in children and adolescents in Ibadan, Nigeria. Cancer 1981; 47(3): 610-14.
27. Tavassoli FA, Devilee P. Tumours of the ovary and peritoneum. In: Pathology and Genetics of tumours of the breast and female genital organs. Lyon: IARC; 2003. p. 113-202.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License