IJCRR - 7(8), April, 2015
Pages: 63-66
Print Article
Download XML Download PDF
CLINICOPATHOLOGICAL AND IMMUNOHISTOCHEMICAL PROFILE OF MAMMARY PAGET DISEASE
Author: Salma Bhat, Rohi Wani, Samina Khanday, Sheema Sheikh, Ruby Reshi, Humaira Bashir
Category: Healthcare
Abstract:Mammary Paget disease (MPD) is a rare manifestation of the nipple-areola complex that is often associated with an underlying in situ or invasive carcinoma. MPD is very often hormone receptor negative. However, unlike ER and PR, Her 2 neu receptor is overexpressed in the vast majority of Mammary paget disease. In this study we have evaluated the clinicopathological and immunohistochemical aspects of this disease. In this retrospective study, all cases of mammary Paget disease referred to the Department of pathology, Government Medical College Srinagar from 2006 till 2013 were evaluated. Collective data were analysed by descriptive statistical analysis methods.There were 19 cases of Mammary paget disease reported from 2006 to 2013. All but one of the MPD cases were associated with an underlying ductal carcinoma .The underlying breast malignancy was high grade with a significant proportion having axillary nodal involvement. One patient had underlying DCIS. On IHC , only two cases of MPD were ER and PR positive. There was a single triple negative MPD case. Conversely Her2 neu was strongly positive in sixteen cases of MPD .The same immunohistochemical spectrum was shared by underlying breast carcinoma including DCIS.
MPD is often associated with extensive underlying malignancy which is of high grade and is frequently Her2 neu positive with a resulting poor prognosis. Therefore for patients with clinical suspicion of MPD breast examination, mammography and even biopsy are highly recommended.
Keywords: Mammary Paget disease, Ductal carcinoma, Her2 neu
Full Text:
INTRODUCTION
MPD has been recognised as a distinct entity for over 120 years.MPD is diagnosed in 0.5%-5% of all breast cancer patients.1 The association of MPD with underlying breast carcinoma was described originally in 1874 by Sir James Paget.2 The clinical appearance of Mammary Paget disease is usually a thickened, sometimes pigmented, eczematoid, erythematous weeping or crusted lesion with irregular borders.3 Usually the lesion is limited to the nipple or extended to the areola and in advanced cases it may also involve the surrounding skin. It is often associated with underlying DCIS and/or invasive ductal carcinoma. Approximately,50% of these patients present with an associated palpable mass in the breast.4 In cases where mass is palpable, invasive carcinoma is likely to be found. On the other hand patients presenting without a clinical mass more likely have DCIS.5 The prognosis for MPD with an underlying palpable mass is poorer than mammary carcinoma without Paget disease. By contrast, the prognosis for Paget disease with minimal intrinsic in situ carcinoma is excellent.6 MPD occurs most commonly in post-menopausal women but may be observed even in younger and adolescent population.7 MPD is very often hormone receptor negative, because the underlying carcinoma tends to to be poorly differentiated. Unlike ER and PR ,Her2 neu is overexpressed in the vast majority of MPD.8 Over expression of Her 2 neu is the result of Her2 neu gene amplification.9 The Her 2 protein has a growth stimulating effect, furthermore it enhances the motility of tumour cells by the interaction of the membrane expressed neoprotein and a motility factor resulting in chemotaxis and invasion of epidermis by the Paget cells.10 Generally in many cases there is a correlation between positive stain ing for Her 2 oncoprotein of Paget cells and underlying in situ or invasive carcinoma.11 Patients with MPD and underlying IDC tend to have greater chance of lymph node metastasis , lower hormone receptor expression and higher Her2 expresssion compared to those without Paget disease.12
MATERIAL AND METHODS
In this descriptive retrospective study, all Paget biopsied samples referred to the department of pathology ,Government medical college, Srinagar since 2006 till 2013 were evaluated. The Inclusion criteria was 1)Mastectomy patients. 2)Had histologically confirmed IDC/DCIS with Paget disease. The tumour was characterised on the basis of histology, tumour grade, regional lymph node status, ER, PR and Her 2neu expression (positive vs negative).
Observations
There were 19 cases of MPD reported from 2006 to 2013. All but one of the MPD cases were associated with ductal carcinoma .The underlying breast malignancy was high grade with a significant proportion having axillary nodal involvement. One patient had underlying DCIS. On IHC , only two cases(10.5%) of MPD and underlying ductal carcinoma were ER and PR positive.There was a single triple negative MPD case. Conversely Her2 neu was strongly positive in sixteen cases(84.2%) of MPD .The same immunohistochemical spectrum was shared by underlying breast carcinoma including DCIS.
DISCUSSION
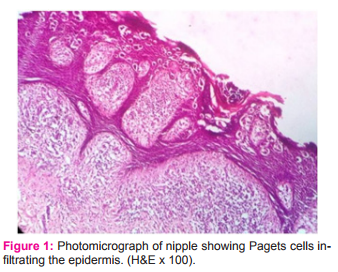
MPD is a rare disorder of the nipple-areola complex that is often associated with an underlying in situ or invasive carcinoma.6 The clinical appearance of MPD is usually a thickened, sometimes pigmented eczematoid, erythematous weeping or crusted lesion with irregular borders.3 Two theories have been proposed to explain the pathogenesis of MPD. The Epidermotropic theory which is the most accepted theory suggests that Paget cells originate from ductal cancer cells that had migrated from the underlying breast parenchyma. This theory is supported by the predominance of Breast cancer markers found in Paget disease.13 Although there are few articles in which MPD is reported in men, all of our 19 cases were women.14 The mean age of our patients was 60 years which was consistent with the findings of Chen,C-Y et al15 where the mean age at diagnosis for MPD was 60 years. In our study, all MPD cases were unilateral and more prevalent on left side. Not even a single case of bilateral MPD was seen in our study which is otherwise also extremely rare16 Mammary Paget disease is characterised by Paget cells. Paget cells are large cells with clear cytoplasm and eccentric, hyperchromatic nuclei found throughout the epidermis.17(Fig. 1)
Patients with Mammary Paget disease have a high incidence of an underlying breast carcinoma.18 The associated carcinoma can be either carcinoma in situ or invasive cancer.19 We found underlying duct carcinoma in 94.7%of cases which was comparable to a study by Lioyd et al where breast cancer was seen in 82%-92% of MPD cases.20 Caliskan M et al also observed in their study that MPD had underlying IDC in 93.8% of MPD cases.21 All the underlying breast tumours were high grade which was comparable to studies by Lester T et al where 93% of the MPD associated tumours had high nuclear grade.22 Axillary lymph node involvement was seen in 68.4% of MPD with underlying IDC. This was 44% in a study by Kothari AS et al.23 There are reports of positive lymph nodes even without any underlying malignancies.21,24 On immunohistochemical evaluation, 84.2%(16 cases) showed strong positivity for Her2 neu(Fig. 2).
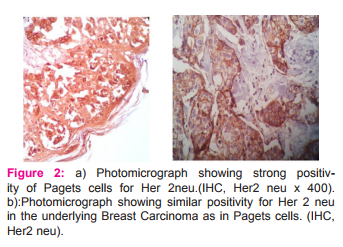
Sek P et al and Fu W et al reported Her 2neu positivity of Paget cells in 86% and 93% of cases respectively.11,25 The same immunohistochemical profile was shared by the underlying breast carcinoma including DCIS(fig 3).Two cases(10.5%) of MPD and associated ductal carcinoma was ER and PR +ve and Her2 neu –ve.In a study by Liegl B et al, ER positivity was seen in 10% of MPD cases.26 There was a single case with triple –ve immunohistochemical profile of the ductal carcinoma and Paget component.
CONCLUSION
MPD is often associated with extensive underlying malignancy which is difficult to assess accurately either clinically or mammographically. The underlying disease is of high grade and is frequently Her2neu positive with a resulting poor prognosis. Therefore for patients with clinical suspicion of MPD breast examination, mammography and even biopsy are highly recommended. Furthermore, larger studies of MPD and prospective follow-up of patients with ductal carcinomas may be useful in elucidating the molecular characteristics that are associated with greatest risk of developing MPD.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Kollmorgen DR, Varanasi JS, Edge SB, Carson WE 3rd. Paget’s disease of the breast: a 33-year experience. J Am Coll Surg. 1998;187:171-177.
2. Paget J. On the disease of the mammary areola preceding cancer of the mammary gland. St. Bartholomew Hosp. Rep. 1874;10:87-89.
3. Karakas C. Pagets disease of the breast.J carcinog 2011;10:31.
4. Kanitakis J. Mammary and extramammary Paget›s disease. J Eur Acad Dermatol Venereol 2007;21:581-90.
5. Yim JH, Wick MR, Philpott GW, Norton JA, Doherty GM. Underlying pathology in mammary Paget›s disease. Ann Surg Oncol 1997;4:287-92.
6. Sakorafas GH, Blanchard K, Sarr MG, Farley DR. Paget›s disease of the breast. Cancer Treat Rev 2001;27:9-18.
7. Martin VG, Pellettiere EV, Gress D, Miller AW. Paget›s disease in an adolescent arising in a supernumerary nipple. J Cutan Pathol 1994;21:283-6.
8. Elzbieta Marczyk,Anna kruczak,Aleksandra Ambicka et al.The routine immunohistochemical evaluation in Paget disease of the nipple.Pol J Pathol 2011;4:229-235.
9. Tanskanen M, Jahkola T, Asko-Seljavaara S, et al. Her2 oncogene amplification in extramammary Paget’s disease. Histopathology 2003; 42: 575-579.
10. Schelfhout VR, Coene ED, Delaey B, Thys S, Page DL, De Potter CR. Pathogenesis of Paget›s disease: epidermal heregulin-alpha, motility factor, and the HER receptor family. J Natl Cancer Inst 2000;92:622-8.
11. Sek P, Zawrocki A, Biernat W, Piekarski JH. HER2 molecular subtype is a dominant subtype of mammary Paget›s cells. An immunohistochemical study. Histopathology 2010;57:564-71.
12. Ling H, Hu X, Xu X-L, Liu Z-B, Shao Z-M (2013) Patients with Nipple-Areola Paget’s Disease and Underlying Invasive Breast Carcinoma Have Very Poor Survival: A Matched Cohort Study. PLOS ONE 8(4).
13. Sandoval Leon AC, Drews- Elger K, Gomez Fernandez CR et al. Paget’s disease of the nipple.Breast Cancer Res Treat.2013;141(1):1-12.
14. Fouad Dina. Paget›s disease of the breast in a male with lymphomatoid papulosis: a case report. Journal of Medical Case Reports 2011; 5:43.
15. Chen CY.,Sun L-M and Anderson B-O. Paget disease of the breast: changing patterns of incidence, clinical presentation, and treatment in the U.S. Cancer. 2006 Oct 1;107(7):1448-58.
16. Xie B, Zheng H, Lan H, Cui B, Jin K, Cao F. Synchronous bilateral Paget›s disease of the breast: A case report Oncol Lett. 2012 Jul; 4(1):83-85.
17. Marques-Costa, JC; Cuzzi, T; Carneiro, S; Parish, LC; Ramos-e-Silva, M (May–Jun 2012). «Paget›s disease of the breast.». Skinmed 10 (3): 160-5.
18. M Muttarak, B Siriya, P Kongmebhol, B Chaiwun, and N Sukhamwang.Paget’s disease of the breast: clinical, imaging and pathologic findings: a review of 16 patients Biomed Imaging Interv J. 2011 Apr-Jun; 7(2): e16.
19. Goro Amano,Mioko Yajima,Yasunori Moroboshi, Yoshiki kuriya and Noriaki Ohuchi. MRI Accurately Depicts Underlying DCIS in a Patient with Paget’s Disease of the Breast Without Palpable Mass and Mammography Findings. Jpn. J. Clin. Oncol. (2005) 35 (3):149-153.
20. Lioyd J and Flanagan AM. Mammary and extramammary Paget’s disease. J Clin Pathol. Oct 2000; 53(10): 742-749..
21. Caliskan M, Gatti G, Sosnovskikh I, et al. Paget’s disease of the breast: the experience of the European Institute of Oncology and review of the literature. Breast Cancer Research and Treatment 2008;112(3):513-521.
22. Lester T1, Wang J, Bourne P, Yang Q, Fu L, Tang P. Different panels of markers should be used to predict mammary Paget’s disease associated with in situ or invasive ductal carcinoma of the breast. Ann Clin Lab Sci. 2009 Winter;39(1):17-24.
23. Kothari AS., Beechey-Newman N, Hamed H, Fentiman IS, D›Arrigo C, Hanby AM, Ryder K. Paget disease of the nipple: a multifocal manifestation of higher-risk disease. Cancer. 2002 Jul 1;95(1):1-7.
24. Siponen E1, Hukkinen K, Heikkilä P, Joensuu H, Leidenius M Surgical treatment in Paget›s disease of the breast Am J Surg. 2010 Aug;200(2):241-6.
25. Fu W1, Lobocki CA, Silberberg BK, Chelladurai M, Young SC Molecular markers in Paget disease of the breast.J Surg Oncol. 2001 Jul;77(3):171-8.
26. Liegl B,Horn LC,Moifar F.Androgen receptors are frequently expressed in mammary and extramammary Paget’s disease.Mod Pathol 2005Oct;18(10):1283-8.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License