IJCRR - 7(9), May, 2015
Pages: 52-60
Print Article
Download XML Download PDF
FINE NEEDLE ASPIRATION CYTOLOGY VERSES CORE NEEDLE BIOPSY IN BREAST LESIONS - A COMPARATIVE STUDY
Author: Siddavatam Supriya, C. Nirmala, Lakshmi S. A. R. Raghupathi
Category: Healthcare
Abstract:Background and Objectives: Fine needle aspiration cytology (FNAC) is a part of triple assessment in evaluation of breast lesions in our country. In the western countries, core needle biopsy (CNB) is fast replacing FNAC as part of screening programmes and early detection of cancer. This study was undertaken to know the advantages, limitations of each procedure and their diagnostic utility in patients in and around Bangalore. Methodology: 50 female patients presenting with breast lesion were subjected to both FNAC and CNB. Grades were assigned as C1-C5 for FNAC and B1-B5 for CNB. Statistical analysis was done using kappa correlation score and the concordance rate between the two procedures was determined. Results: The most common age group was between 21-40 years and left sided lesions were more common. Out of 50 cases, there was concordance between FNAC and CNB in 38 cases and 12 cases were discordant. Kappa score of agreement was 0.559 indicating a moderate degree of concordance between the two tests. Conclusion: Both FNAC and CNB are equally good in assessment of breast lesions. However, FNAC is more suitable in the developing counties, for palpable lesions due to better turnaround time and it is cost effective. Whenever there is discrepancy between clinical findings, imaging studies and FNAC, CNB can be used as the next step in assessment before definitive treatment. Also, it can be used in cases of low grade malignancies, where it is difficult to give a diagnosis of malignancy on FNAC alone.
Keywords: Fine needle aspiration cytology (FNAC), Core needle biopsy(CNB), Breast lesions
Full Text:
INTRODUCTION
The breast is one of the common sites of cancer, mostly in women. It is also a common site for different types of benign lesions, like benign tumors, and inflammatory processes. FNAC has been used since a long time for this purpose, along with clinical examination and mammography. It is popular because of its accuracy, cost effectiveness, and ease of use1 . However, it has certain limitations like inability to differentiate between invasive and in situ carcinomas, insufficient samples and false negative results2 . Core Needle Biopsy has recently gained popularity, especially in the evaluation of non-palpable breast lesions3 . It has the advantages of lower inadequacy rates, allowing of ancillary methods, grading and typing of cancer2 . However, it is more time-consuming and expensive2 . The present study was taken up to compare and analyze the advantages and limitations of FNAC and CNB in patients in preoperative assessment and in diagnosing breast lesions.
MATERIALS AND METHODS
A prospective study was done, patients presenting with a breast lesion to Department of Pathology, Victoria and Bowring and Lady Curzon Hospitals during the period of November 2013 to October 2014.All the patients were subjected to both FNAC and CNB.
Procedure of FNAC
The breast lump is palpated and fixed between 2 fingers. After observing aseptic conditions, a 22-24 gauge disposable sterile needle with 10ml disposable syringe was used to enter the swelling and multiple passes were given. Smears were made, air dried and wet fixed, stained with Giemsa stain and Haematoxylin and Eosin stains. The samples were categorized from C1 to C5. [Table 1]
Procedure of core needle biopsy
Following xylocaine test dose the area to be biopsied was cleaned and depending on the case, 2 to 4 ml of 2% xylocaine was injected into the swelling and the overlying skin for local anaesthesia. After 5-8 minutes, the sterile automated 18 gauge core biopsy gun with a 20mm throw is introduced into the breast and keeping the direction of the gun away from the chest wall, it was released so that a core of tissue of breast nodule is taken into the gun. The device is removed and the core transferred to a container having 10% formalin solution. For each patient, 2 to 3 cores are taken. The biopsies are fixed in 10% formalin 8-12hrs and processed routine histopathology. Sections taken at 3 to 4 micron thickness, and stained with Hematoxylin and Eosin stains. The biopsy slides were categorized from B1 to B5. Statistical analysis was performed using med-calc and open epi software and results were tabulated. [Table 2]
RESULT
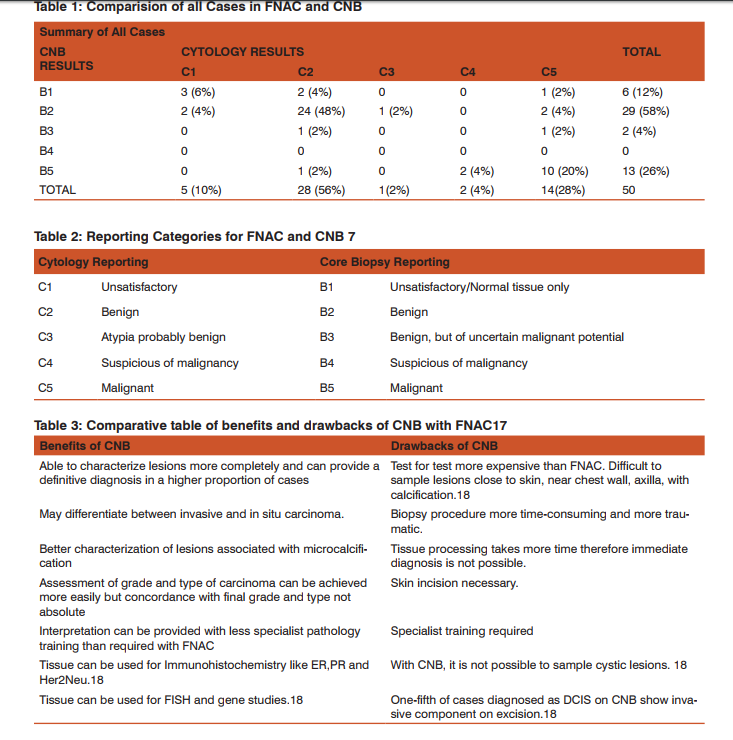
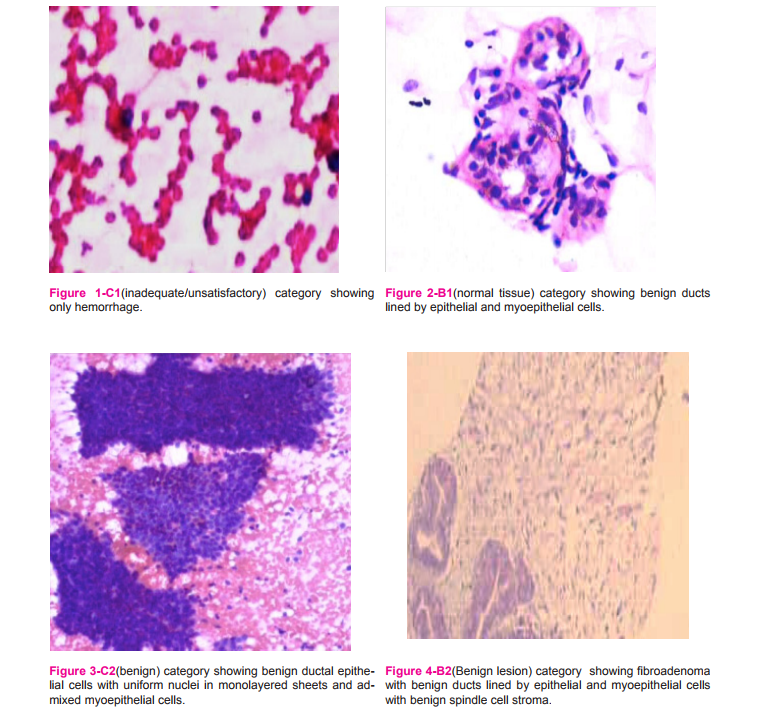
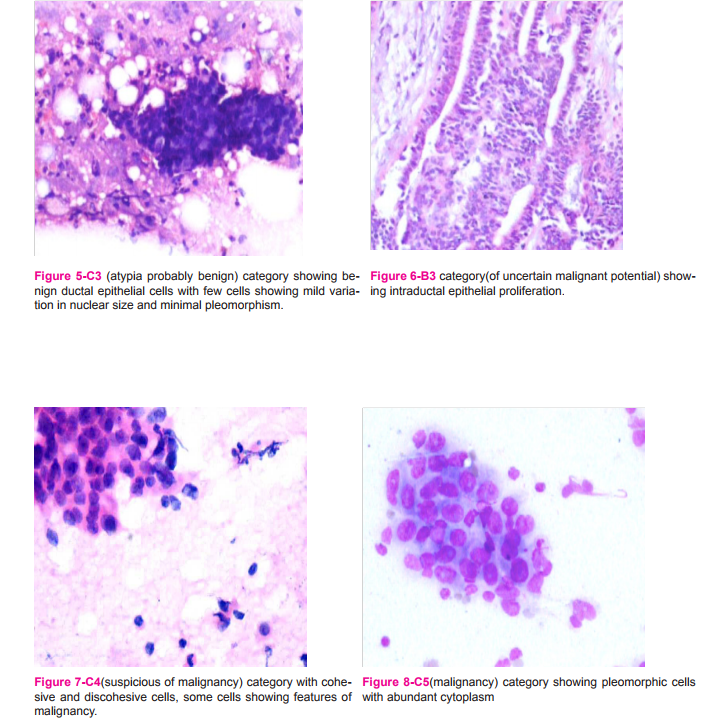
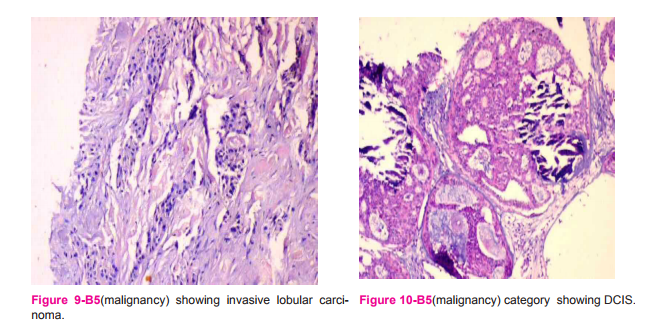
In our study, 10% cases were in C1 category,(fig 1) (inadequate/unsatisfactory aspirate) on CNB showed 3 cases in B1 category (fig 2) (normal tissue) and 2 cases in B2(benign) category. C2 category (fig 3) (benign) composed of maximum number of cases, that correlated well with B2 category (fig 4)with few cases in B1, B3,(fig 6) and 1 malignant lesion on biopsy was also diagnosed as C2 on cytology. This was a case of DCIS on biopsy cohesiveness of tumor cells and minimal pleomorphism was seen, it was misplaced in C2 category. [Table 3] 3 cases of inflammatory breast lesions were diagnosed on FNAC as well as CNB, these were Breast Abscess, Fat necrosis and Granulomatous mastitis. One case in our study belonged to C3 category(fig 5) (atypia probably benign) due to cellularity and nuclear pleomorphism which was categorized as B2 on CNB. 2 cases were categorized as C4 (fig 7)(suspicious of malignancy) due to discohesive cells and minimal pleomorphism was diagnosed as malignant lobular carcinomas on CNB. 14 cases were diagnosed in C5 category(fig 8) (malignant), out of which 10 cases were diagnosed malignant on CNB. 4 cases were in B1, B2 and B3 category, misdiagnosed due to absence of malignant tissue in the core biopsy which can be attributed to the sampling error. As all our cases underwent biopsy without guidance the malignancy was missed on CNB this error could be reduced by radiological guidance. Cytology showed more sensitivity in the diagnosis of malignancy than CNB in our study. In a study by Chuo et al, the 68 cases diagnosed as C5 category all proved to be malignant on CNB and were classified under B5 category4 (fig 9 and 10).This could be attributed to usage of guided biopsy wherever necessary.
DISCUSSION
Both FNAC and CNB are useful in the preoperative assessment of breast lesions, in both palpable and nonpalpable lesions, with or without radiological guidance. Both procedures have their own advantages and limitations, when judiciously used can complement each other and increase the pre-operative diagnostic accuracy considerably. While there is widespread preference for CNB in most developed countries, FNA is still valuable initial procedure for evaluating palpable breast lesions5 . FNAC is a well accepted procedure in developing countries due to its low cost, safe and affordable with rapid results5 , pain is minimal and no further care is needed6 . FNAC requires an excellent aspirator to obtain satisfactory material and breast cytopathologic expertise in interpreting breast aspirates. The narrow gauge needle used in FNAC can be directed into different areas of the lesion and the tissue is sampled in more than one plane. It is said that FNAC sees 10 times more tissue than CNB, due to the multiple passes, also because all the aspirated material can be studied at once and hence incidence of missing the diagnosis due to sampling error is less compared to CNB. FNAC selectively samples tumor cells in sclerotic tumors. FNAC is an excellent method of obtaining cells for microarray transcriptional profiling studies. Core biopsy was introduced in the late 1990s in the assessment process of screen-detected abnormalities of breast, and later was followed in symptomatic breast clinics as well7 . The various devices available include 14 to 18 gauge core biopsy guns which can be done with or without image guidance by either ultrasound or mammography8 . The gauge of needle used for CNB is also important, 14 gauge needle offers more tissue and hence better sensitivity and specificity9 .
Core biopsies are done under local anesthesia with or without a skin incision. The biopsy gun has a spring mechanism. The trocar is present inside, which is thrust forward approximately 2cm, depending on the gun and at almost same time, the cutting cannula present outside is thrust over the inner trocar filling the inside notch with the breast tissue specimen8 . The CNB procedure is expensive due to the higher cost of the biopsy gun. The biopsy guns are available as disposable guns and guns with disposable needles. The biopsy procedure is more time consuming and traumatic due to use of larger bore needles. CNB can be associated with complications like vasovagal reaction, infection, pneumothorax, infarction, epithelial displacement and needle tract malignant seeding are rarely seen and described in literature5 . However no such complications were encountered during our study. Difficulties are encountered while doing CNB in lesions close to the skin, chest wall, in axilla, with calcification and in small lesions due to less control over the needle in automated guns used for CNB whereas these lesions can be satisfactorily sampled on FNAC. Care needs to be taken while doing the CNB procedure near vital organs, chest wall, large blood vessels with automatic CNB guns .The needle has a fixed throw, the direction and depth of penetration of the needle should be calculated before doing the procedure to avoid damage to vital organs. FNAC is at less risk of penetrating the vital organs as the needle is more under the control of the operator. The depth and direction can be changed by the feel of the tissue while doing the procedure. FNAC is suitable in aspiration of benign cystic lesions where as it is not possible to obtain tissue sample on CNB. Fine-needle aspiration (FNA) can be used for the diagnosis of inflammatory swellings of breasts such as abscess, granulomatous diseases including tuberculosis, where the aspirates can be used for culture of organisms and special stains like Ziehl-Neelsen, Gram’s stain can be used to identify bacilli10. FNA is preferred in sampling multifocal lesions. It can be reliably used for pathologic confirmation of an inoperable advanced stage breast cancer before systemic therapy. It is also preferred during post surgery followup of breast cancer patients, to sample chest wall lesions and to determine whether they are due to recurrence or reactive in nature. Preoperative evaluation of axillary, supraclavicular nodes is preferably conducted with FNA, which also eliminates the need for sentinel node biopsy. FNAC can be used to diagnose metastatic tumors to breast5 . In a study by Willems et al, FNAC is more suitable for patients on anticoagulants and for lesions close to the skin, chest wall, vessels and implants or very small lesions. However, popularity of FNAC is decreasing due to paucity of well trained cytopathologists at individual centers, leading to more diagnostic errors. It may yield low cellular aspirates in cases which have abundant fibrotic or desmoplastic stroma. CNB may be used as a second line diagnostic tool in lesions which FNA yields insufficient cells and equivocal diagnosis. Since there is lack of histologic architecture, sometimes, even a cellular smear cannot yield an accurate diagnosis18 .But it has not achieved surgical decision making and management process for both the surgeon and oncologist at the expected level11. Also, Surgeons find it difficult to accept FNAC reports for making a definitive diagnosis as they lack important information about features like histopathological type, grade, intrinsic behavior of tumor etc12.
CORE NEEDLE BIOPSY
CNB is more accurate than FNAC13 and in screen detected lesions, it is reasonable to undertake CNB14. It may be used as a second line diagnostic tool for lesions in which FNAC yields an equivocal diagnosis or insufficient cells. It is also preferred when determination of in-situ versus invasive carcinoma/tumor sub typing is required5 . CNB is more invasive and time consuming than FNAC but less invasive and time-consuming than excisional biopsy. It has similar limitations like FNAC such as sampling errors. It requires local anesthesia and on-site immediate assessment of material is not available. With CNB it is not possible to aspirate fluid collections. CNB can be associated with subsequent histologic changes such as hemosiderin deposits, fibrosis, foreign body reaction and infarction of lesion like papilloma. Post VACB, there can be ultrasound appearance mimicking malignancy5 . The pathologist should correlate the histopathological findings with radiological abnormality. For routine breast cancer patients, the types of carcinoma and lymphovascular invasion are assessed. Receptor analysis is done. Prognostic factors derived from core biopsies correlate well with surgically excised specimens but the grade may be underestimated because of low mitotic rate estimated on a smaller sample. Pure Ductal Carcinoma In Situ is usually detected as microcalcifications on mammography and less commonly as mass lesion15.
LIMITATIONS OF FNAC ASPIRATES
A definite diagnosis is not possible sometimes by FNAC either due to inherent limitations of cytological examination or by inability to obtain adequate material for diagnosis16. By FNAC it may be difficult to distinguish between fibroadenoma and phyllodes tumor, fibroadenoma and fibrocystic change, fibroadenoma and papillary lesions.
Occasionally, it may be difficult to distinguish between myxoid change in fibroadenoma and mucinous carcinoma, and benign sclerosing lesions from low-grade carcinoma. It may be difficult to give a definitive diagnosis on FNAC alone in cases of low grade or borderline lesions such as Atypical Ductal Hyperplasia, Atypical Lobular Hyperplasia, papillary lesions, tubular carcinoma and invasive lobular carcinoma5 . Apocrine cells in smears may appear rather pleomorphic and may dissociate. Recognition of the dusty blue cytoplasm, with or without cytoplasmic granules with Giemsa stains or pink cytoplasm on Papanicolaou or Haematoxylin and Eosin stains coupled with a prominent central nucleolus is the key to identifying cells as apocrine17. Aspirates from lobular carcinoma are sometimes difficult to interpret. In the present study all cases diagnosed as lobular carcinoma on CNB were interpreted as suspicious of malignancy (C4). The cellularity of these specimens is usually less than that seen in ‘Ductal’ carcinoma and can appear small benign-looking uniform to atypical. The presence of small three-dimensional collections of cells with only slightly enlarged nuclei is a helpful clue. A large number of cells with intracytoplasmic lumina in association with the above features is an indication of lobular carcinoma, although not specific17. Also, Ductal Carcinoma In Situ and Invasive ‘Ductal’ carcinoma cannot be distinguished accurately by cytology alone18. While some of the cases of Ductal carcinoma in situ are overtly malignant, the small cell type may present a diagnostic dilemma. The cellularity of these samples are moderate, they are never as cellular as frank carcinomas. One should be guided by the increased nuclear/cytoplasmic ratio in the presence of normal size cells. The abnormal nuclear chromatin pattern is a clue to the real nature of the lesion. The presence of some necrotic debris in the background should alert the interpreter to the possible malignant nature of the lesion. A clue in some cases can be obtained from the architectural pattern within the rather rigid and monomorphic clumps. In some cases a report of intraductal proliferation (atypical or suspicious) may be all that can be given, and in such cases biopsy may be the only way to resolve the problem17.
LIMITATIONS OF CORE NEEDLE BIOPSIES
Interpretational errors are seen with CNB such as distinguishing between Fibroadenoma and Phyllodes tumor, benign and atypical or malignant papillary lesions, between Atypical Ductal hyperplasia and low-grade Ductal Carcinoma In Situ and between complex sclerosing lesion / radial scar and tubular carcinoma5 . Certain lesions diagnosed on core biopsies can be associated with pitfalls and may require excision. These lesions include fibroepithelial lesions such as pseudoangiomatous hyperplasia, atypia including flat epithelial atypia, papillary lesions, mucinous lesions, radial scar, complex sclerosing lesion, malignant processes that mimic benign lesions15. Also, in cases diagnosed as Atypical Ductal Hyperplasia on CNB, excision is recommended19. Mild atypia of epithelium within lobular units is one of the commonest problems encountered in core biopsy samples. These should not be overdiagnosed, as epithelial hyperplasia, apocrine change or reactive changes. Conversely, more severe degrees of atypia must be looked for, as these may reflect cancerization of lobules by high grade DCIS. The degree of atypia should be helpful in distinguishing the process, and the nuclear chromatin and presence of mitoses (although rarely seen) may aid in the diagnosis17. Proliferations of stroma may cause difficulties in diagnosis in core biopsy samples. Sometimes, a second biopsy sample taken from a patient may show fibroblastic proliferation; this may represent the target lesion but could also reflect tissue reaction and repair at the previous biopsy site. If the lesion is from the core site, an associated histiocyte reaction or fat necrosis may be present and hemosiderin-laden macrophages may be seen. A stromal proliferation may also be seen in phyllodes tumor and evidence for an epithelial component should be looked for, for example by taking deeper sections17. Immunohistochemistry(IHC) may not prove helpful and the multidisciplinary approach must be applied to the clinical, radiological and histopathological features. When a definitive histological diagnosis cannot be made, the abnormality should be reported as a spindle cell lesion of uncertain histogenesis or nature and classified as B317. A phyllodes tumor may rarely be difficult to distinguish from other stromal lesions. Usually, the differential diagnosis lies between a cellular fibroadenoma and a phyllodes tumor. Features including stromal atypia, if present, can be helpful, but the degree of cellularity of the stroma is the most valuable feature to assess. In rare cases, it is not possible to distinguish between these two lesions and the sample should be reported as a ‘fibroepithelial lesion’ and classified under B317. Small foci of invasive lobular carcinoma can be missed in histological sections and be dismissed as chronic inflammation of stromal cells. The targetoid infiltrative pattern of classical lobular carcinoma may be helpful, but a reactive process containing lymphocytes can also have a periductal or perilobular distribution. IHC with cytokeratin, to demonstrate the neoplastic cells is of value in difficult cases17.
CONCLUSION
Both FNAC and CNB are useful in the preoperative assessment of breast lesions, in both palpable and nonpalpable lesions with or without radiological guidance. Both procedures have their own advantages and limitations, they can complement each other. While there is widespread preference for CNB in most developed countries, FNA is still valuable initial procedure for evaluating palpable breast lesions5 , in view of its ease, simplicity, affordability, safety, and rapidity, low-cost and high degree of accuracy In cystic lesions, CNB procedure is not possible whereas, FNAC gives sufficient material to diagnose these cases. Malignancy can also be made out accurately by FNAC. However, it cannot distinguish between in-situ and invasive components with ease. FNAC requires an excellent aspirator to obtain satisfactory material and breast cytopathologic expertise in interpreting breast aspirates and in countries with limited resources like India, FNAC may be used as the sole sampling technique or first line of diagnostic tool for pathologic evaluation. Unsatisfactory samples are obtained on FNAC when the lesions contain abundant fibrotic or desmoplastic stroma leading to sampling error even in the hands of experienced pathologists. CNB proves to be very useful in such cases in obtaining the sample5 . CNB can further classify benign lesions in subtypes which is difficult to classify on cytology. The cases in C3 (atypia probably benign) and C4 (suspicious, probably malignant) category, indecisive on cytology could be given a definitive diagnosis on CNB. Hence CNB can be used as a confirmation test in such cases where definite opinion cannot be given on cytology. Tissue obtained by CNB can be used for IHC and genetic studies. With image guidance, the sensitivity rate increases and sampling error can be reduced. It should be determined by patient’s economic status, preference of managing surgeon, need for biomarker studies, availability of equipment and expertise, clinical and radiological indications5 . Both FNAC and CNB are complimentary to each other and are useful in diagnosis of breast lesions. Both procedures have specific advantages and limitations. CNB cannot replace FNAC, it is not needed to diagnose all breast lesions. It can be used as an adjunct in cases indecisive on cytology and those cases requiring biomarker studies.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.

References:
1. Rikabi A, Hussain S. Diagnostic Usefulness of Tru-Cut Biopsy in the Diagnosis of Breast Lesions. Oman Med J. 2013; 28:125-27
2. Ghaemian N, Siadati S, Nikbakhsh N, Mirzapour M, Askari H, Asgari S. Concordance rate between Fine Needle Aspiration Biopsy and Core Needle Biopsy In Breast lesions. Iranian Journal of Pathology 2013; 8: 241-246
3. Ballo MS, Sneige N. Can Core Needle Biopsy Replace Fine Needle Aspiration Cytology in the Diagnosis of Palpable Breast Carcinoma. American Cancer Society 1996; 773-77.
4. Chuo CB and Corder AP. Core biopsy vs fine needle aspiration cytology in a symptomatic breast clinic. EJSO. 2003; 29: 374-78
5. GongY. Breast Cancer: Pathology, Cytology, and Core Needle Biopsy. Methods for Diagnosis Breast and Gynecological Cancers: An Integrated Approach for Screening and Early Diagnosis in Developing Countries. 2013; 19-37
6. Outpatient Cytopathology Center(US). FNA or Core Needle Biopsy? Johnson City; 2004.
7. Pilgrim S, Ravichandran D. Fine needle aspiration cytology as an adjunct to core biopsy in the assessment of symptomatic breast carcinoma. Breast. 2005; 14: 411–14
8. Kass RB, Lind DS, Souba WW, Breast Procedures- 1[Internet]. North Carolina: WebMD;2007. Available from http://www.med.unc.edu/surgery/education/files/articles/ACS%20surgery%20breast%20procedures.pdf
9. Luechakiettisak P, Rungkaew P. Breast Biopsy: Accuracy of Core Needle Biopsy Compared with Excisional or Incisional Biopsy: A Prospective Study. The THAI J SURGERY. 2008; 29:6-10
10. Bukhari MH, Arshad M, Jamal S, et al., Use of Fine-Needle Aspiration in the Evaluation of Breast Lumps.Pathology Research International 2011; Article ID 689521, 10 pages, 2011. doi:10.4061/2011/689521
11. Hassan TMM, Rao AM. S Does Final-Needle Aspiration Cytology Of The Breast Is Still An Accurate Diagnostic Technique for Breast Lumps? IOSR JDMS. 2014; 13: 37-44
12. Bdour M, Hourani S, Mefleh W, Shabatat A, Karadsheh S, Nawaiseh O et al. Comparision Between Fine Needle Aspiration Cytology And Tru-Cut Biops In The Diagnosis Of Breast Cancer .Journal of Surgery Pakistan 2008; 13: 19-21
13. Homesh NA, Issa MA, El-Sofiani HA. The diagnostic accuracy of fine needle aspiration cytology versus core needle biopsy for palpable breast lumps. Saudi Med J. 2005; 26: 42-46
14. Lieske B, Ravichandran D, Wright D. Role of fine-needle aspiration cytology and core biopsy in the pre-operative di-agnosis of screen-detected breast carcinoma. Br J Cancer. 2006; 95(1): 62-66.
15. Joshi M, Reddy SJ, Nanavidekar M, Russo JP. Russo AV, Pathak R. Core biopsies of the breast: Diagnostic pitfalls. IJPM. 2011; 54: 671-682
16. Bajwa R, Zulfiqar T. Association of Fine Needle Aspiration Cytology with tumor size in palpable breast lesions. Biomedica 2010; 26: 124-129
17. Non operative diagnosis subgroup of the National Coordinating Committee for Breast Screening Pathology. Guidelines for non-operative diagnostic procedures and reporting in breast cancer screening. NHSBSP publication number 50. Sheffield, NHS Breast Screening Programme Publications, 2001.
18. Radhakrishna S, Gayathri A, Chegu D. Needle core biopsy for breast lesions: An audit of 467 needle core biopsies. Indian J Med Paediatr Oncol. 2013; 34: 252–56.
19. Koo JS, Kim MJ, Kim E, Jung W. Factors in the Breast Core Needle Biopsies of Atypical Ductal Hyperplasia that can predict Carcinoma in the Subsequent Surgical Excision Specimens. J Breast Cancer 2010; 13: 132-137
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License