IJCRR - 7(12), June, 2015
Pages: 60-63
Print Article
Download XML Download PDF
CLINICAL PRESENTATION AND MANAGEMENT OF 100 CONSECUTIVE CASES OF THYROID
ASSOCIATED OPHTHALMOPATHY SEEN IN THE OUT- PATIENT DEPARTMENT OF A REGIONAL INSTITUTE OF OPHTHALMOLOGY
Author: Garima Agrawal
Category: Healthcare
Abstract:Introduction: Thyroid associated ophthalmopathy is an autoimmune disorder. It is a life -long disease with systemic and ocular manifestations. Early diagnosis and appropriate management of this disorder are essential. Aim: Clinical presentation and management of 100 consecutive cases of Thyroid associated ophthalmopathy seen in the outpatient department of a regional institute of ophthalmology. Material and Methods: All patients of Thyroid associated ophthalmopathyseen in our institute were subjected to a complete clinical work up, ultrasonography B scan, computed tomographic scan, triiodothronine, thyroxine and thyroid stimulating hormone assays. Treatment of thyroid dysfunction and thyroid ophthalmopathy were given as per protocol. Observation and Results: Age of patients ranged from 17-63 years. The female:male ratio was 1.7:1. Distribution of thyroid dysfunction was hyperthyroidism (96%), hypothyroidism(3%) and euthyroid(1%). Majority of patients had mild (68%) and /or quiescent disease(77%). Eyelid retraction was the most common presentation (88%). Other presentations were exophthalmos( 63%), extraocular myopathy(37%), soft tissue inflammation (23%) and optic neuropathy (12%). Thyroid dysfunction was treated with anti thyroid drugs(100%), thyroidectomy(12%), radioactive iodine(1%). Thyroid ophthalmopathy was treated with supportive therapy(100%), glucocorticoids(32%), ocular surgery(27%), orbital radiotherapy (1%), cyclosporine(1%).
Conclusion: We present the clinical manifestations and management of Thyroid associated ophthalmopathy patients at a regionalinstitute of ophthalmology. A larger percent of patients required glucocorticoids reflecting the referral of moderate-severe and/or active patients to our tertiary care centre.
Keywords: Thyroid associated ophthalmopathy, Clinical presentation, Management
Full Text:
INTRODUCTION
Thyroid associated ophthalmopathy is an auto immune disorder involving the orbital muscles and orbital fat.1 It presents clinically as lid retraction, exophthalmos, extraocular muscle involvement, optic neuropathy and inflammation. Management includes serum levels of triiodothyronine, thyroxine, thyroid stimulating hormone and imaging in the form of computed tomography scan and B scan ultrasonography. Treatment includes treatment of thyroid dysfunction and treatment of ophthalmopathy. Treatment of ophthalmopathy includes supportive treatment, glucocorticoids, surgery, orbital radiotherapy and other immunosuppressive agents.2,3,4 We designed a study to document the clinical presentation and management of 100 consecutive cases of thyroid associated ophthalmopathy seen in the out-patient department of our regional institute of ophthalmology.
AIM
Clinical presentation and management of 100 consecutive cases of Thyroid associated ophthalmopathy seen in the out-patient department of a regional institute of ophthalmology.
MATERIAL AND METHODS
100 consecutive cases of thyroid associated ophthalmopathy were studied. The study was carried out at our Regional Institute of Ophthalmology. All patients were subjected to history taking, visual acuity examination, Intraocular pressure measurement, slit lamp examination, dilated fundus examination, ocular movements and colour vision. The patients were classified as mild and moderate-severe1 . Clinical activity score was used to classify disease as active or quiescent. Presence or absence of optic neuropathy was documented on basis of vision, colour vision, afferent pupillary defect and optic disc edema or pallor. Extraocular myopathy as evidenced by enlargement of muscle bellies was documented on ultrasonography B scan and non contrast computed tomographic scan. Apical crowding on computed tomographic scan provided an additional documentation of optic neuropathy. Thyroid dysfunction was documented by triiodothyronine, thyroxine and thyroid stimulating hormone assays. Informed consent was taken from all patients. Treatment included treatment of thyroid dysfunction using anti thyroid drugs, thyroidectomy, radio active iodine(single fixed dose of 370 Mbq). Treatment of thyroid ophthalmopathy was done. This included patient counselling, stopping smoking, lubrication, nocturnal head elevation, cool compresses, dark glasses, prisms(where required) and taping of lid at night as per patient presentation. Sight threatening optic neuropathy was treated with intravenous corticosteroids followed by oral steroids. Patients with moderate to severe and/or active ophthalmopathy were also treated with intravenous steroids followed by oral steroids. Intravenous steroids were given as a pulse therapy i.e. 4 cycles of 15 mg/kg followed by 4 cycles of 7.5 mg/kg. Oral steroids were given in a dose of 1mg/kg followed by tapering as per response. Surgery of orbital decompression was reserved for unresponsive patients (no response after 2 weeks of steroids in optic neuropathy).Cosmetic surgery was reserved for patients whose disease has been inactive for at least 6 months .Orbital radiotherapy was an option in patients with active Graves ophthalmopathy resistant to steroids. Retro orbital radiotherapy was used in a dose of 20Gy in 12 fractions over 2 weeks. Cyclosporine in an initial dose of 7.5 mg/kg body weight per day followed by tapering as per response was used in cases resistant to steroids.
OBSERVATIONS AND RESULTS
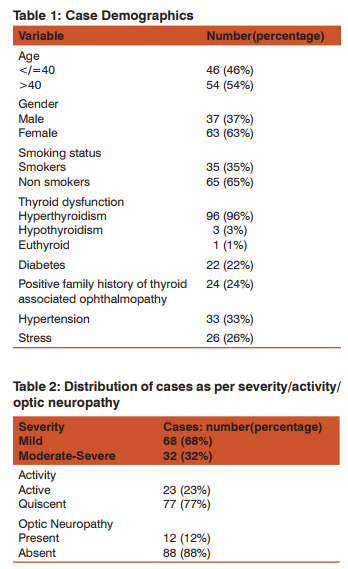
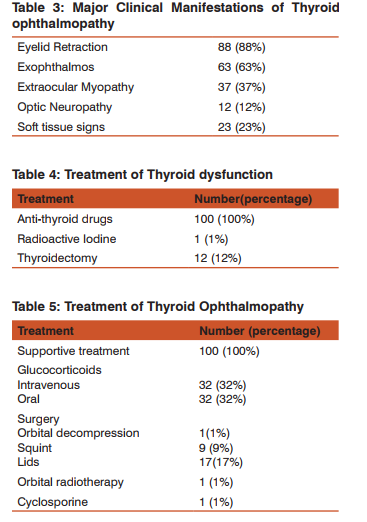
Table 1 shows the case demographics. 46 out of 100 patients were 40 years of age. Range was 17-63 years. There were 63 females and 37 males with female: male ratio of 1.7:1.35(35%) patients were smokers. All of these patients were male. Hyperthyroidism was seen in 96% and hypothyroidism in 3%. 1 patient was euthyroid. The diagnosis of thyroid opthalmopathy followed or preceded the diagnosis of thyroid dysfunction by +/- 24 months. 22 % patients were diabetic, 24% patients had positive family history of Thyroid associated ophthalmopathy. 33% patients had hypertension. 26 patients gave a concurrent history of some associated stress as illness, pregnancy etc. Table 2 shows the distribution of cases as per severity/ activity/optic neuropathy. 68 out of 100 cases had mild Graves ophthalmopathy. 32 patients had moderate- severe disease. The ophthalmopathy was active in 23 patients while majority of patients (77) had quiescent disease. 12 cases had optic neuropathy. Table 3 shows the major clinical manifestations of Thyroid Ophthalmopathy. Eyelid retraction was the most common presentation seen in seen in 88 patients followed by exophthalmos in 63 patients. Extraocular myopathy as evidenced by restricted ocular movements and enlarged muscle bellies on ultrasonography B scan and computed tomography scan was seen in 37 patients. The most frequently enlarged muscles were medial rectus and inferior rectus. Optic neuropathy was uncommon and seen in 12 out of 100 patients. Soft tissue signs of active Graves ophthalmopathy were seen in 23 patients. All these five presentations together were seen infrequently in 7% patients. Table 4 shows the treatment of thyroid dysfunction. Anti -thyroid drugs were used in all cases. 12 cases required thyroidectomy. 1 patient was given radioactive iodine. Table 5 shows the treatment of Thyroid Ophthalmopathy. Supportive treatment was given in all cases. 32 patients received treatment with intravenous or oral glucocorticoids. These were patients with moderate-severe and/or active disease. Ocular surgery was required infrequently. Lid lengthening was done in 17 cases. Squint surgery was required in 9 cases. Orbital decompression surgery was done in one case for optic neuropathy. Orbital radiotherapy was given in one case. Cyclosporine was given in one case.
DISCUSSION
We report the clinical presentation and management of 100 consecutive cases of Thyroid associated Ophthalmopathy in a regional Institute of Ophthalmology. The disease was found in all age groups (17-63 years). Female:male ratio was 1.7:1. 96% patients had hyper-thyroidism, 3% had hypothyroidism and 1% were euthyroid. The diagnosis of thyroid ophthalmopathy followed or preceded the diagnosis of thyroid dysfunction by +/- 24 months. Majority of the patients had mild (68 patients) and/or quiescent disease (77 patients). Moderate- severe disease was observed in 32% and/or active disease in 23% cases. All active cases fitted into the moderate to severe category while not all moderate to severe patients had active inflammation. The most common clinical presentation was eyelid retraction (88%). The other presentations were exophthalmos(63%), extraocular myopathy (37%), soft tissue inflammation(23%) and optic neuropathy(12%). Only 7% patients had all five clinical presentations. Thyroid dysfunction was treated with anti thyroid drugs with 12 cases requiring thyroidectomy and one patient radioactive iodine. Thyroid ophthalmopathy was treated as per protocol. Supportive therapy was given in all cases.32% patients were treated with glucocorticoids (higher % as compared to other studies).Ocular surgery distribution was lids(17%), squint(9%) and orbital decompression (1%). Bartley GB et al reported that eyelid retraction is the most common clinical sign of Graves’ ophthalmopathy. The complete constellation of typical features (hyperthyroidism, eyelid retraction, exophthalmos, restrictive extraocular myopathy, and optic nerve dysfunction) occurs relatively infrequently.5 Bartley GB reported incident cases of Graves ophthalmopathy in Olmsted city, Minnesota. Female: Male ratio was 6:1. 90% had Graves hyperthyroidism, 1% had primary hypothyroidism, 3% Hashimoto’s thyroiditis and 5% were euthyroid. Clinical features seen were eyelid retraction (90%), exophthalmos(60%), restrictive extraocular myopathy (40%)and optic nerve dysfunction (6%). Only 5% patients had complete constellation of clinical findings.6 Bartley GB et al reported the chronology of Graves ophthalmopathy in an incident cohort. Median age at time of diagnosis of Graves ophthalmopathy was 43 years(8 – 88 years).There is a strong temporal relationship between thyroid and eye manifestations of Graves disease. The diagnosis of Graves ophththalmopathy tends to follow the diagnosis of hyperthyroidism (either concurrent with diagnosis of thyroid dysfunction or six months before or after the diagnosis of thyroid dysfunction).7 Jankauskiene J et al reported that in patients with active Graves ophthalmopathy there was increase of proptosis, periorbital edema, chemosis and injection of conjunctiva. On ultrsonography B scan there was a marked increase in the volume of medial rectus and inferior rectus eye muscles.8 Bartley GB et al reported the treatment of Graves ophthalmopathy in an incident cohort.74.2% required no therapy or only supportive measures. 5 % patients were treated with systemic steroids. One patient had orbital radiotherapy. 24 patients (20%) underwent one or more surgical procedures. The probability of surgical intervention was significantly related to patient age (older than 50 years) but it was not related to gender or smoking.9 Marcocci C et al reported the occurrence of ophthalmopathy in Graves disease. They reported that active Graves ophthalmopathy was associated with hyperthyroidism in 91.4% patients. It was not accompanied by thyroid dysfunction in 8.6% cases. Female:Male ratio was 2:1. Age distribution revealed a peak prevalence in the fifth decade of life. In 85% patients the first ocular manifestations occurred within +/- 18 months around the onset of hyperthyroidism, 10
CONCLUSION
We present the clinical manifestations and management of 100 consecutive cases of Thyroid associated ophthalmopathy in a regional institute of ophthalmology. The findings are concurrent with other studies on the topic though we report a higher percentage of use of glucocorticoids. This reflects the referral of difficult cases with active and/or moderate-severe disease to our tertiary care centre. We have also distributed patients as per activity and severity not seen in the studies cited in this article. Thyroid associated ophthalmopathy is a life long disease and appropriate diagnosis and treatment are crucial for the management of this auto immune disorder.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Bartalena Luigi, Tanda Maria Laura. Grave’s Ophthalmopathy. N Engl J Med 2009;360:994-1001.
2. Bartalena L, Baldeschi L,Dickinson A et al.Consensus statement of the European Group on Grave’s Orbitopathy (EUGOGO) on management of Graves orbitopathy. Eur J Endocrinol 2008;158:273-285.
3. Bartalena L, Baldeschi L, Dickinson A et al. Consensus statement of the European Group on Grave’s Orbitopathy(EUGOGO) on management of Graves orbitopathy. Thyroid 2008;18:333-346.
4. Zang S, Ponto KA, Kahaly GJ. Clinical review:I ntravenous glucocorticoids for Graves Orbitopathy:efficacy and morbidity. J ClinEndocrinol Metab 2011;96(2): 320-32.
5. Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, Gorman CA. Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol 1996 Mar;121(3):284-90.
6. Bartley GB. The epidemiologic characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc. 1994;92:477-588.
7. Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, Gorman CA. Chronology of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol. 1996 Apr;121(4):426-34.
8. Jankauskiene J, Imbrasiene D. Investigations of ocular changes, extraocular muscle thickness, and eye movements in Graves’ ophthalmopathy. JhnMedicina (Kaunas). 2006;42(11):900-3.
9. Bartley GB1, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, Gorman CA. The treatment of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol. 1996 Feb;121(2):200-6.
10. Marcocci C1, Bartalena L, Bogazzi F, Panicucci M, Pinchera A. Studies on the occurrence of ophthalmopathy in Graves’ disease. ActaEndocrinol (Copenh). 1989 Apr;120(4):473.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License